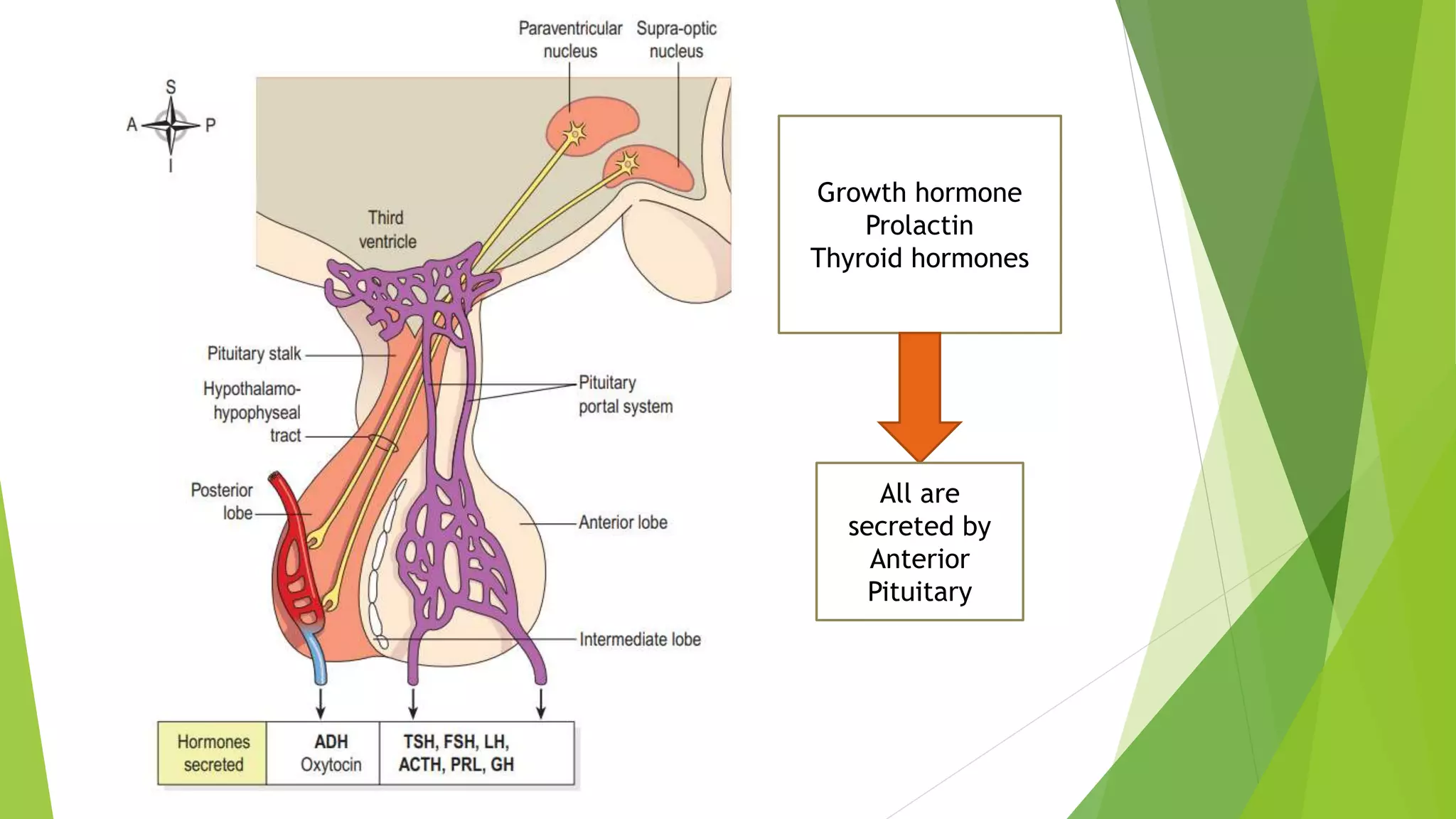
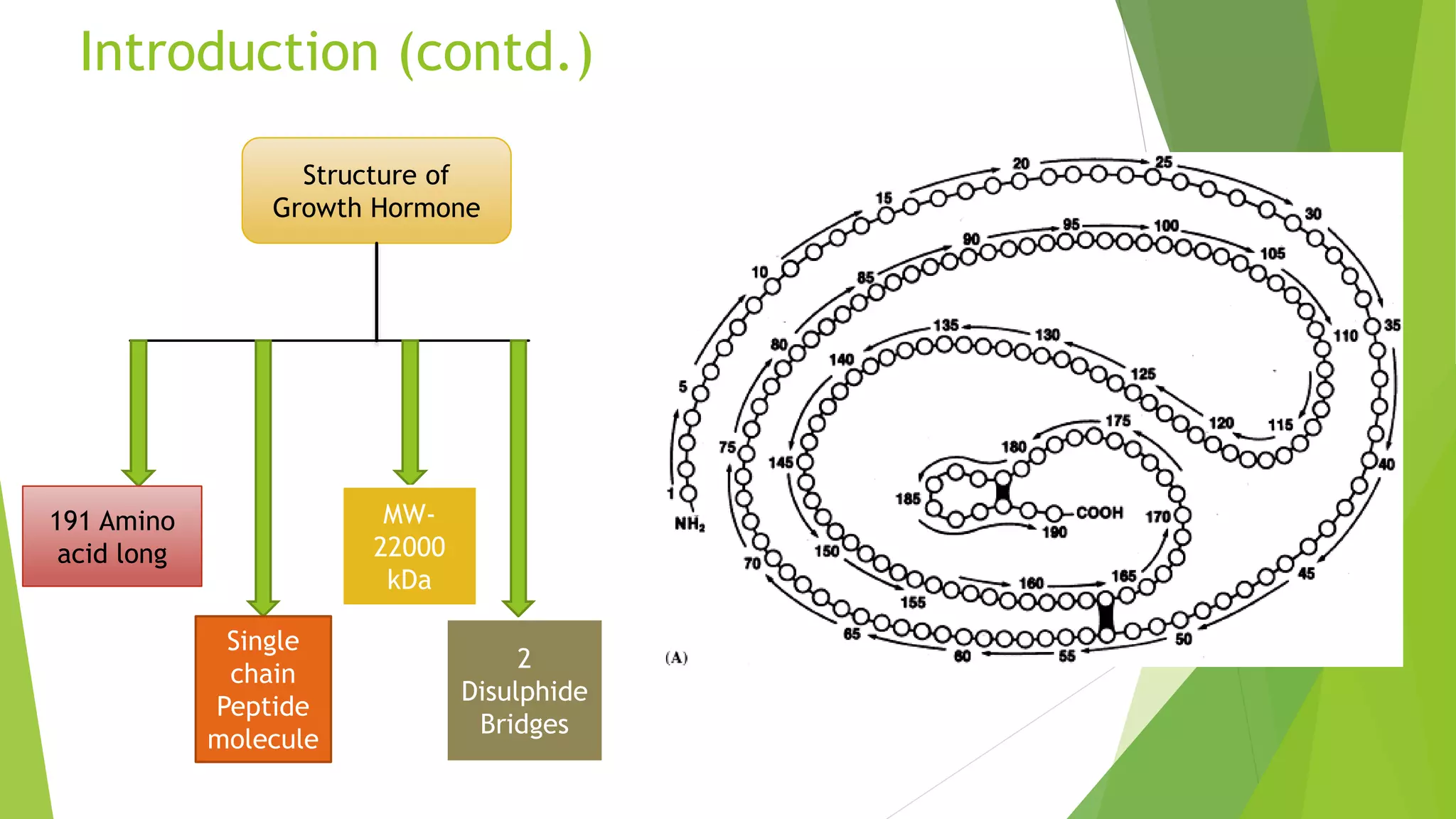
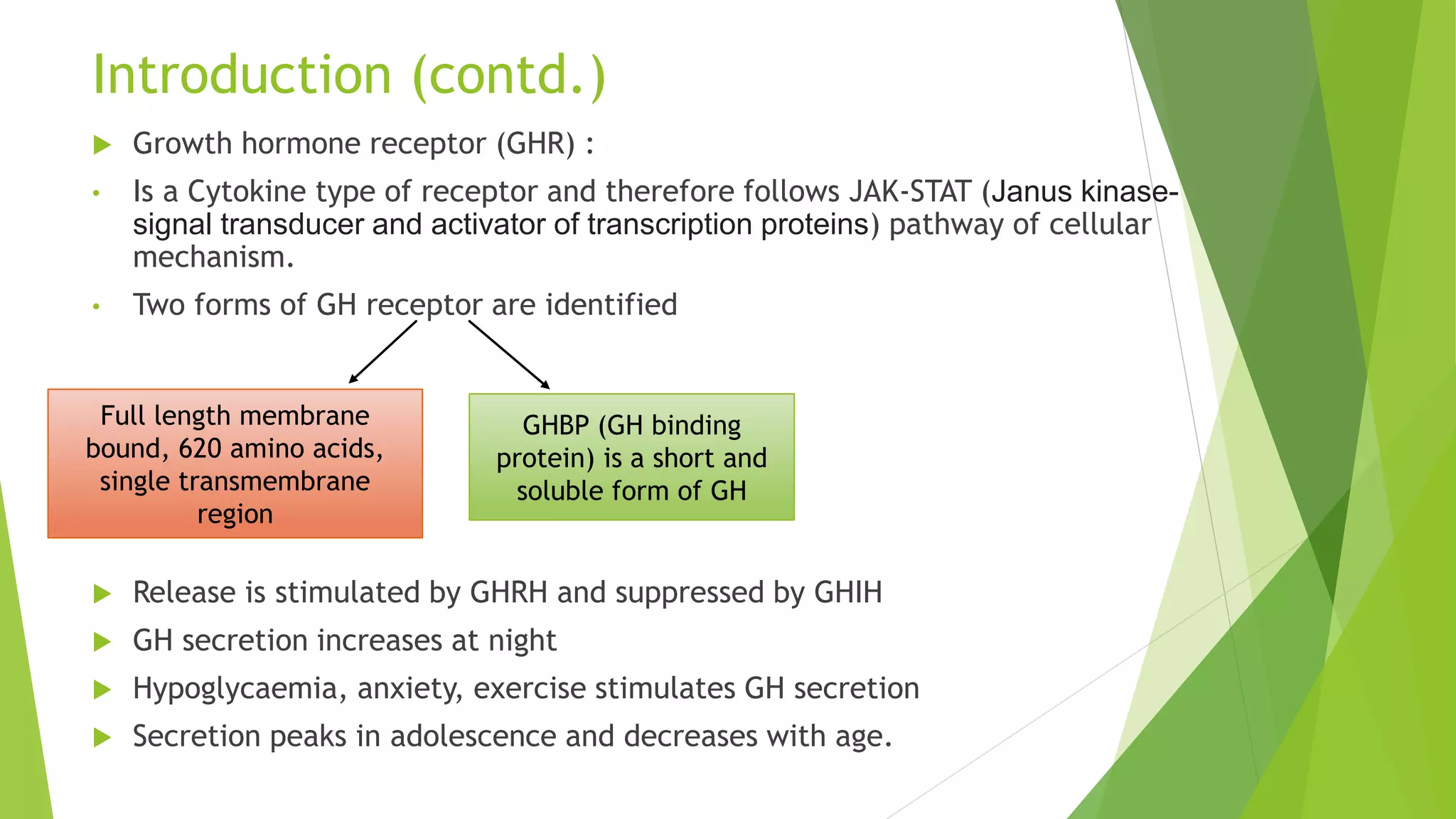
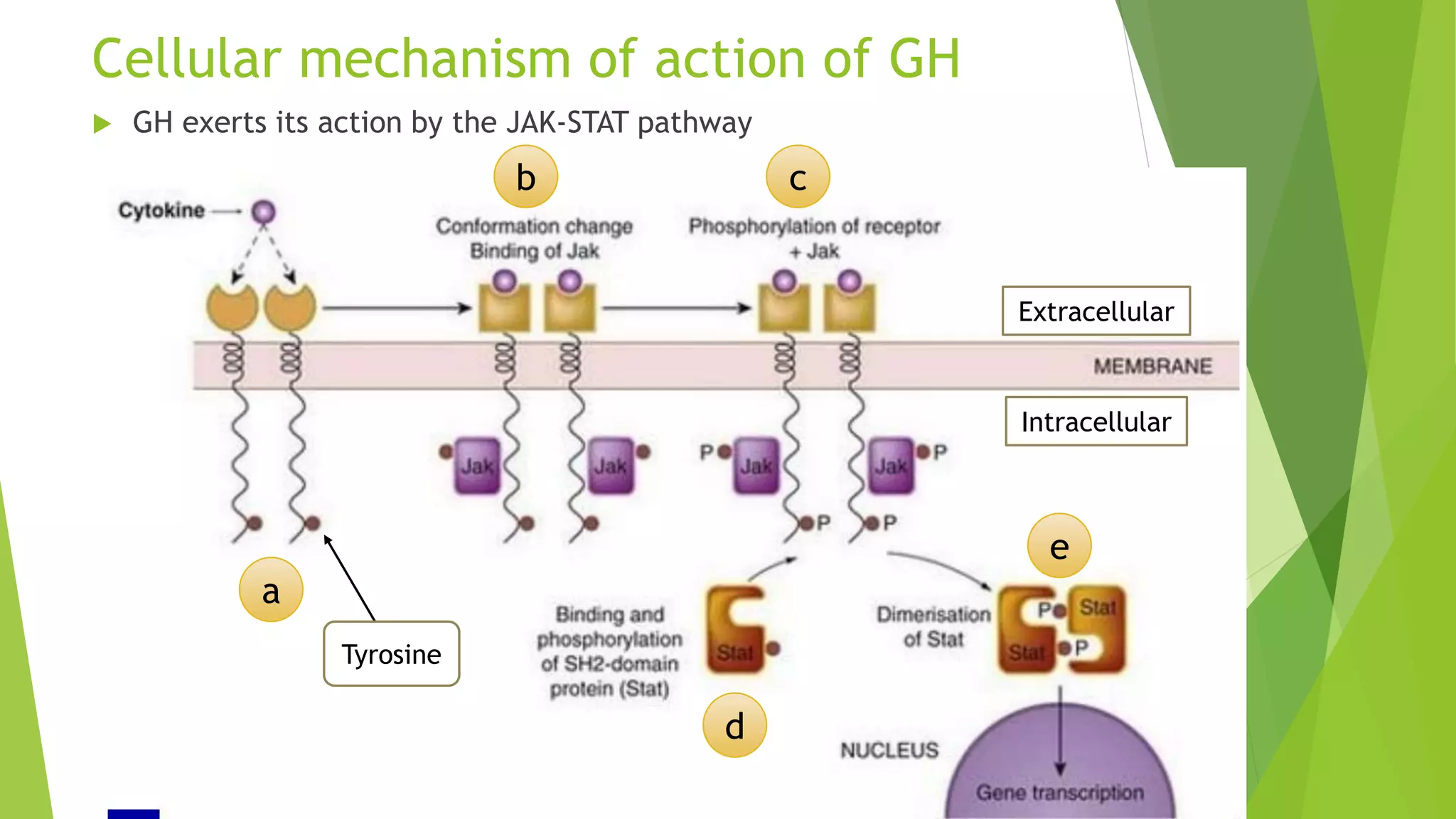
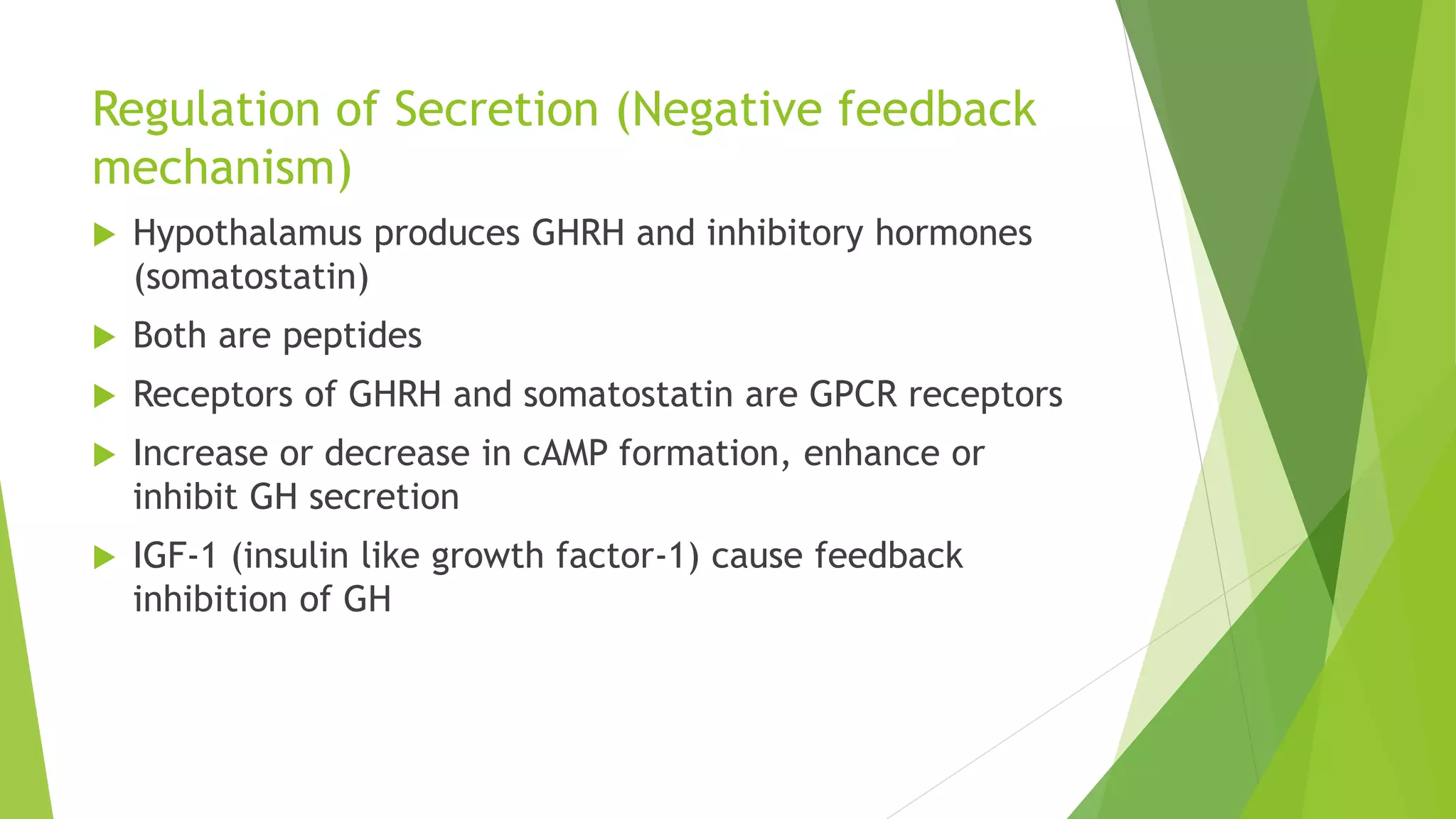
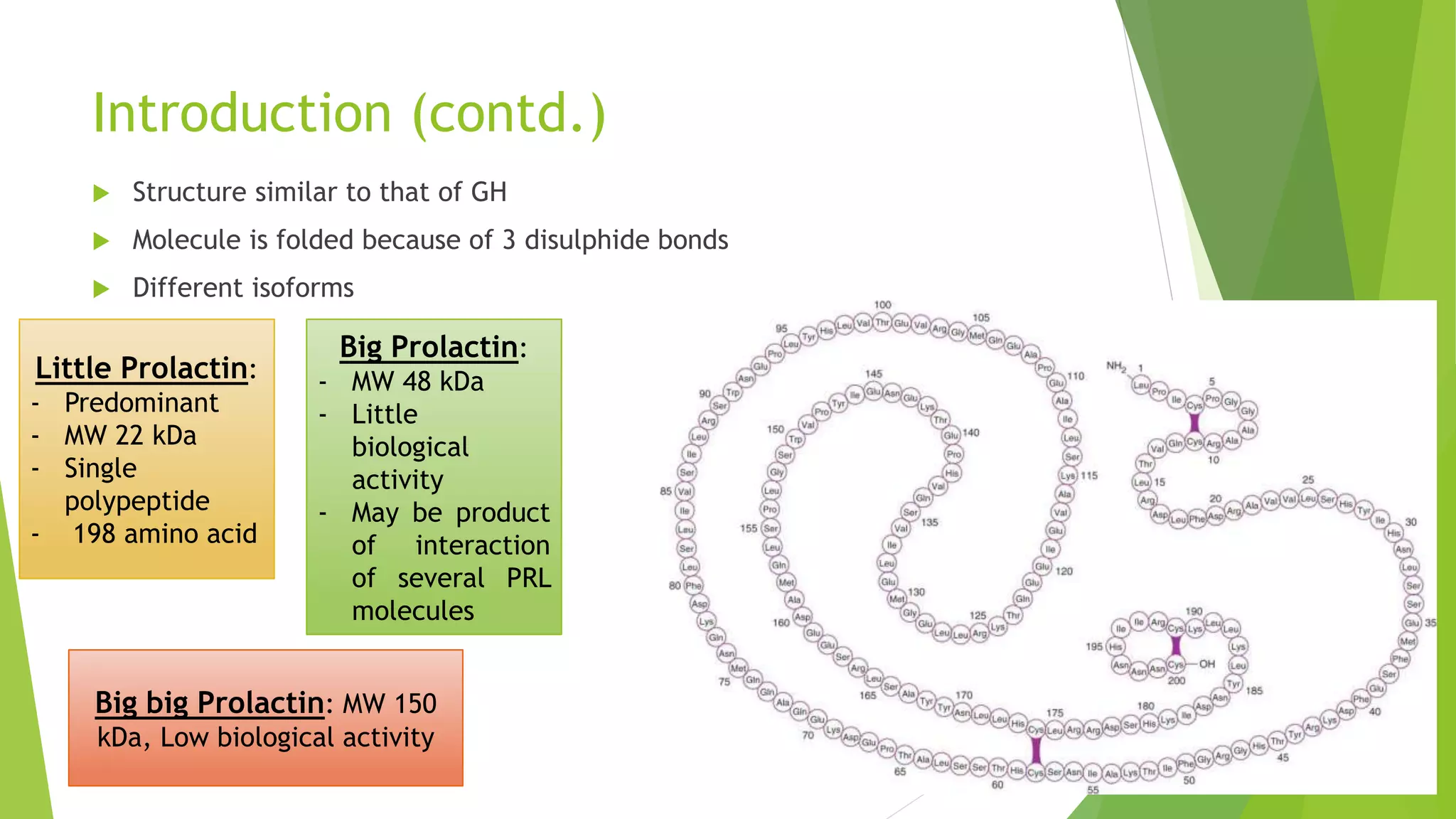
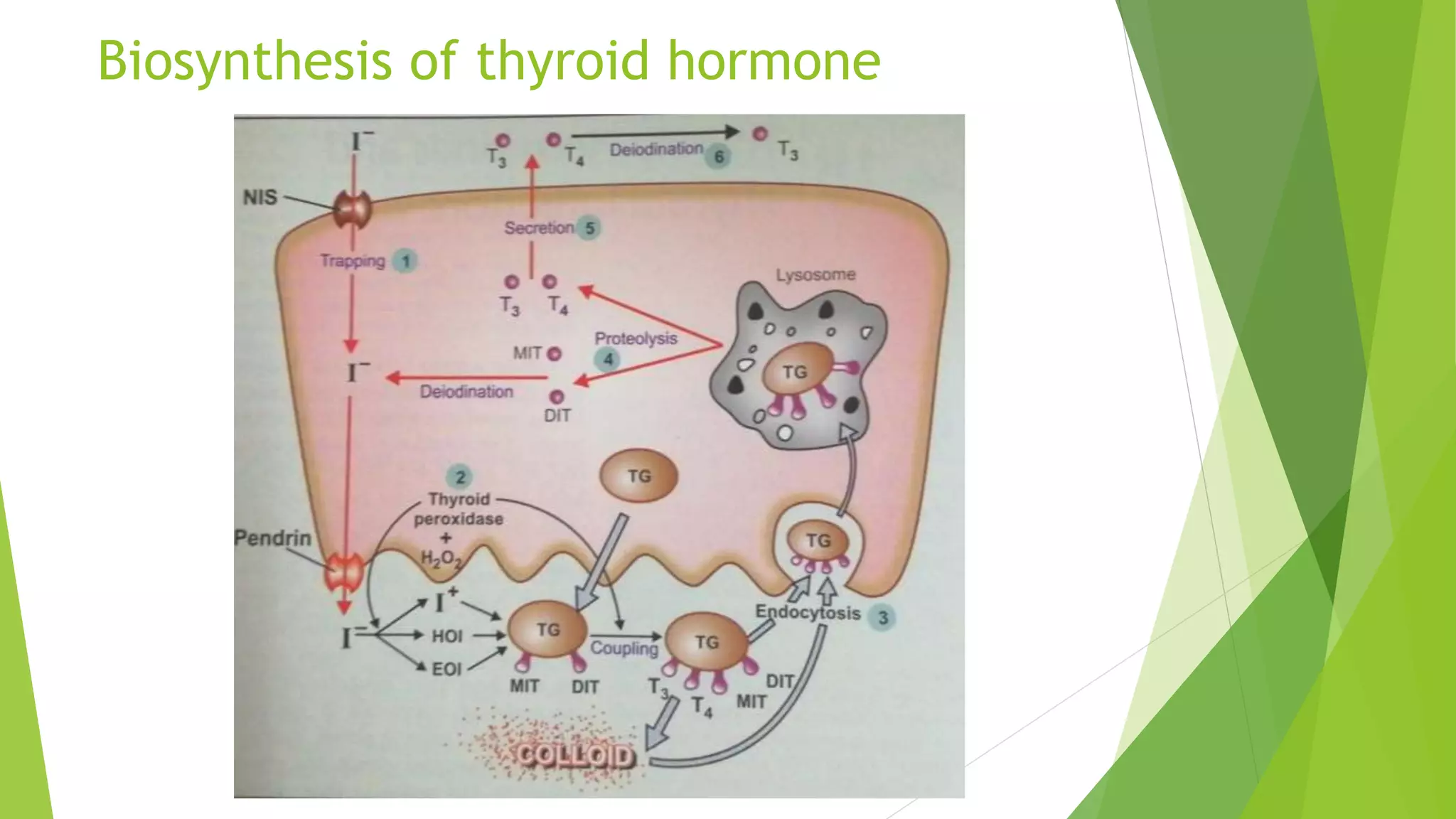
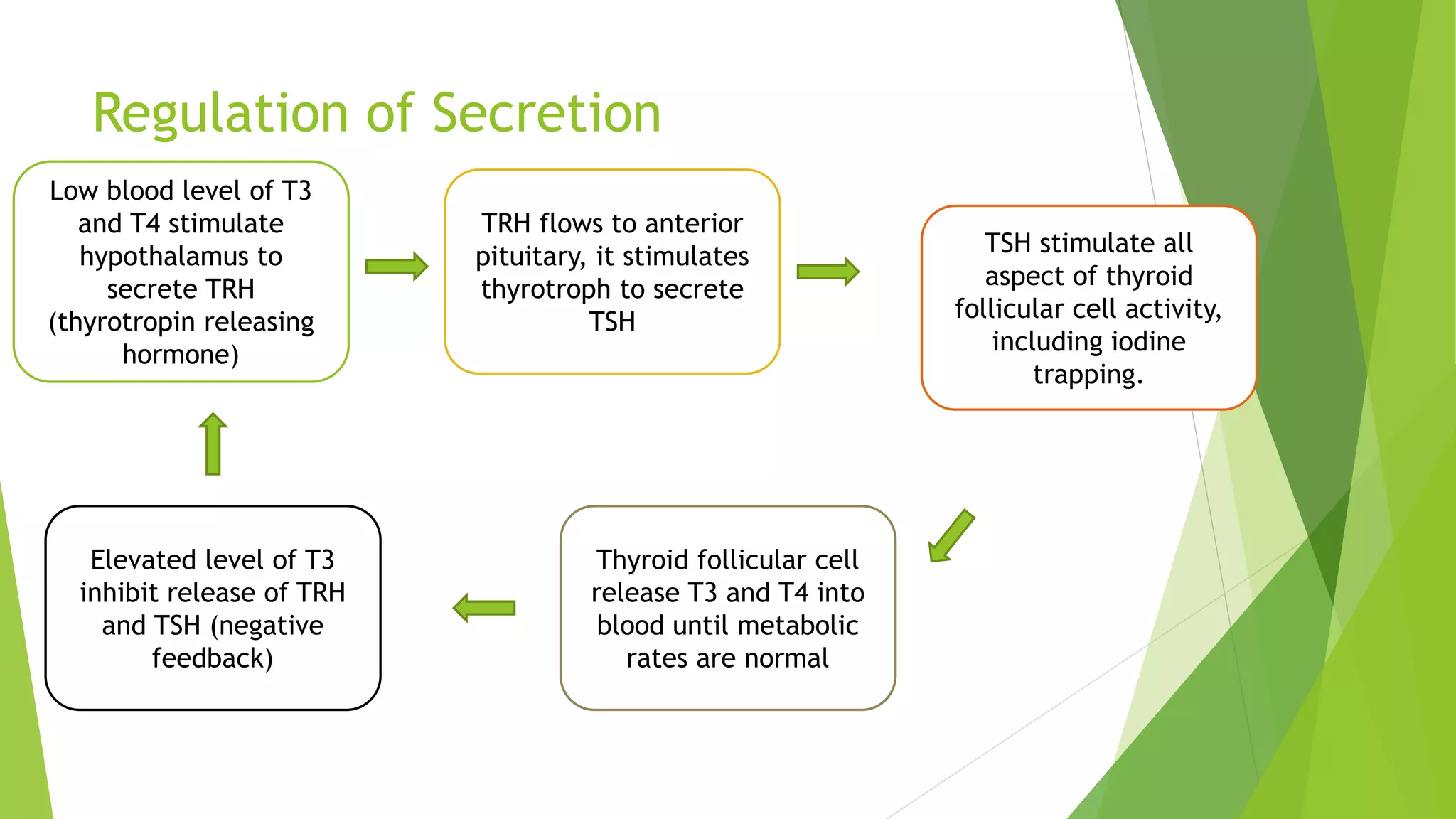
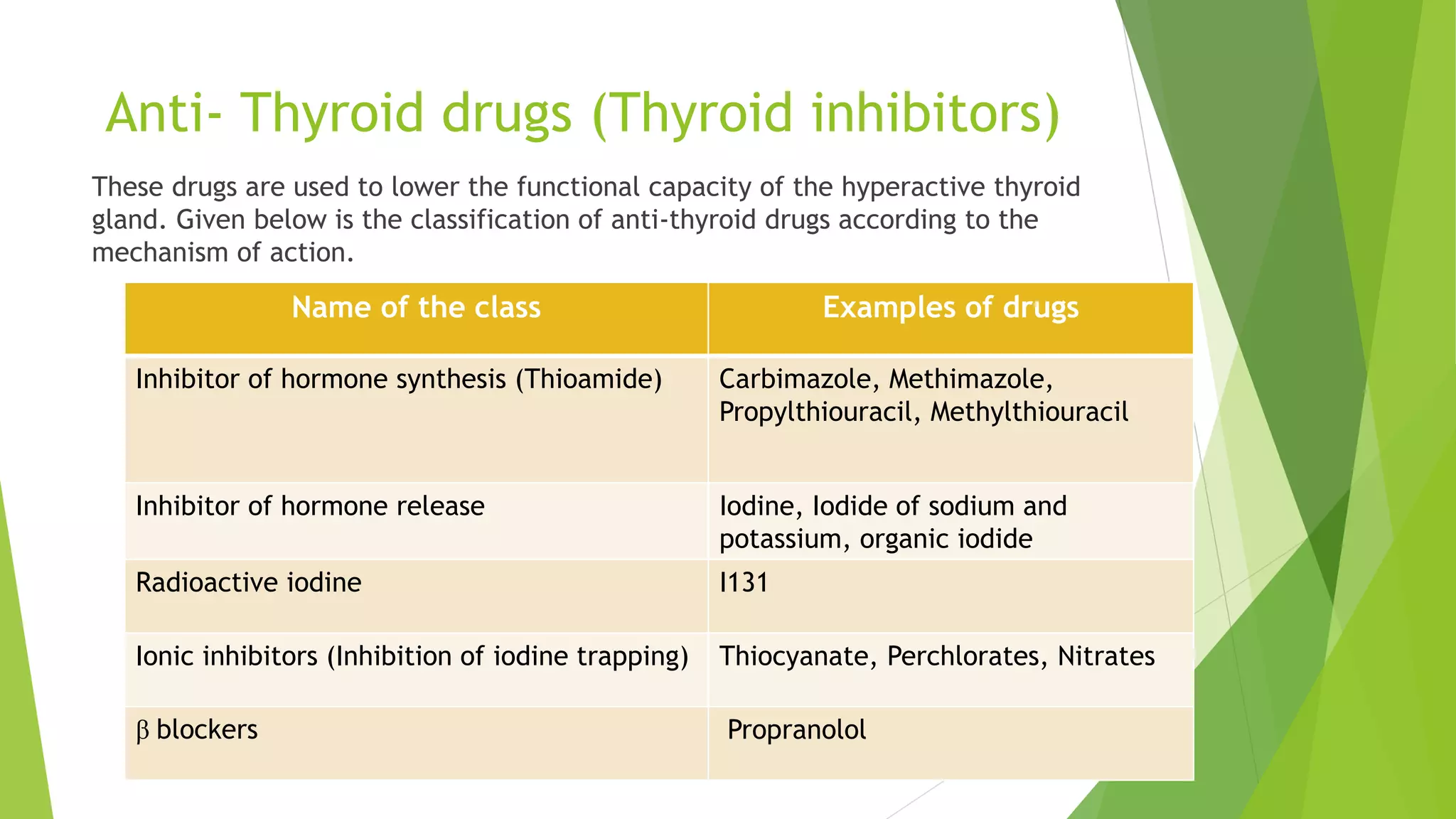
The document details the molecular and cellular mechanisms of action of hormones such as growth hormone, prolactin, and thyroid hormones, focusing on their synthesis, secretion, and physiological effects. It outlines the regulation of these hormones, their receptors, and therapeutic uses, along with associated inhibitors and anti-thyroid drugs. Additionally, it discusses various conditions related to hormone deficiency and excess, as well as the mechanisms and classifications of drugs used to manage these conditions.