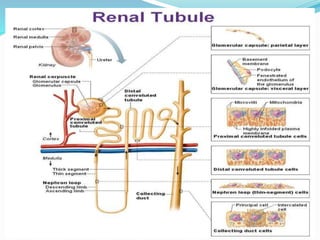
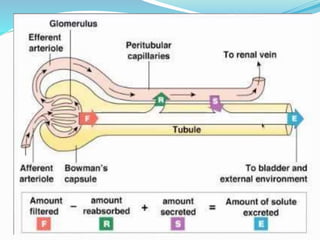
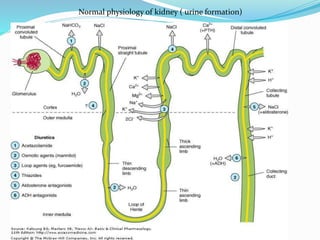
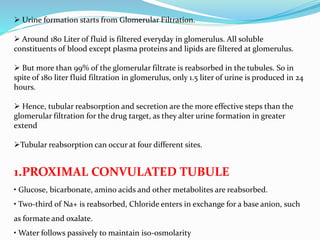
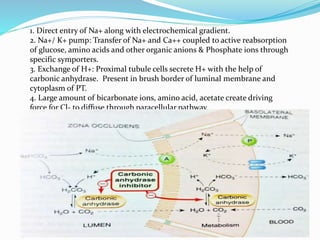
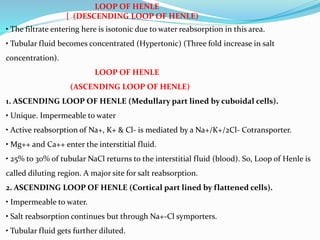
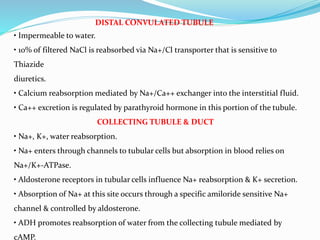
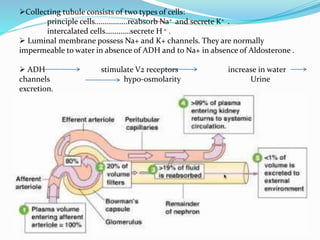
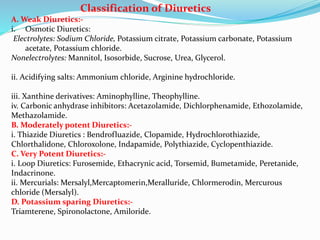
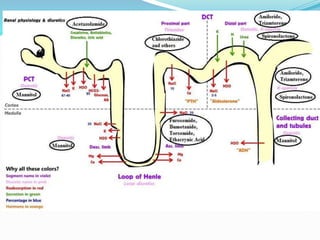
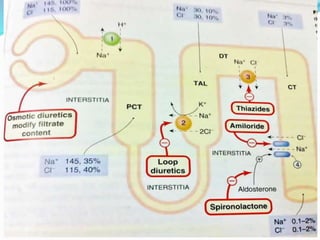
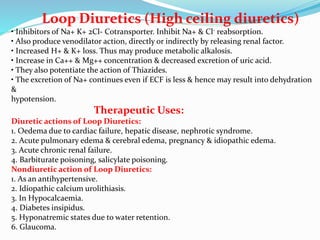
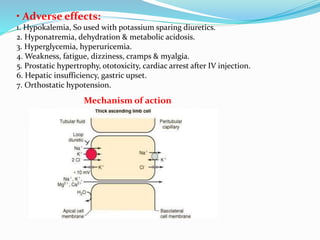
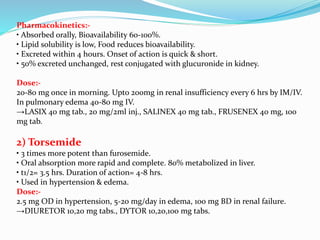
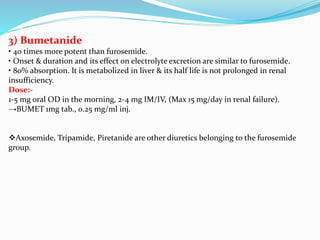
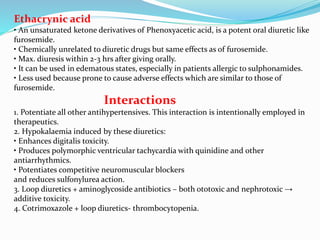
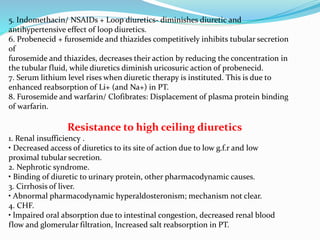
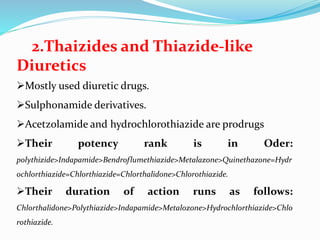
This document discusses the mechanism of action and classification of diuretic drugs. It begins by explaining the normal physiology of urine formation in the kidney and sites of tubular reabsorption. It then classifies diuretics based on potency and site of action. Loop diuretics such as furosemide are described as very potent diuretics that act in the thick ascending loop of Henle by inhibiting sodium-potassium-chloride reabsorption. Their pharmacological effects and mechanisms are explained in detail. Other loop diuretics including torsemide and bumetanide are also briefly discussed. The document concludes by noting some important drug interactions with loop diuretics.