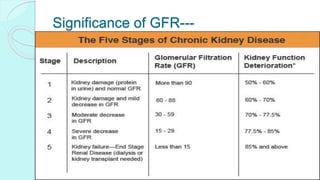
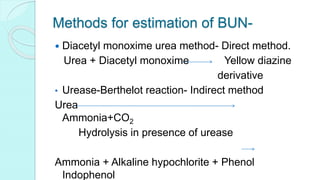
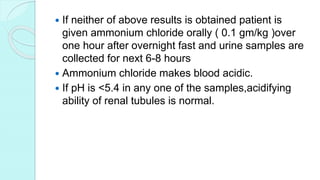
This document discusses renal function tests and their use in evaluating kidney function. It describes the key functions of the kidney including fluid balance, waste excretion, blood pressure regulation, vitamin D and erythropoietin production. Tests are classified as evaluating glomerular function like glomerular filtration rate (GFR) tests or tubular function. GFR is best measured by creatinine clearance or equations using creatinine, age, and other factors. Urine and blood tests can indicate glomerular or tubular dysfunction. Clearance tests measure the removal of substances from blood by the kidneys. Renal biopsy may be used to diagnose kidney disease when function tests are unclear.