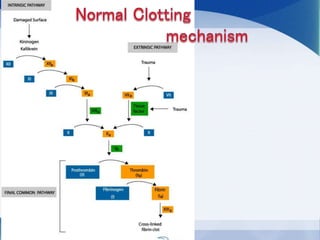
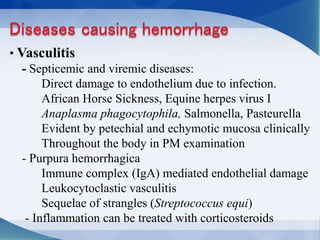
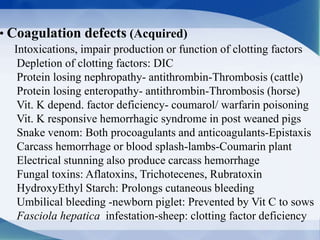
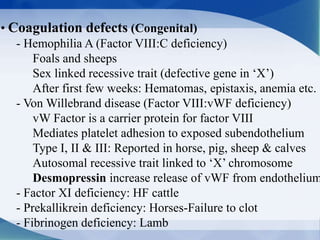
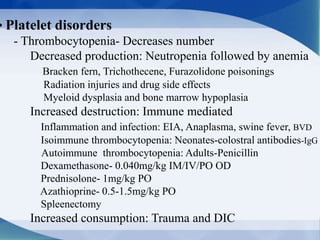
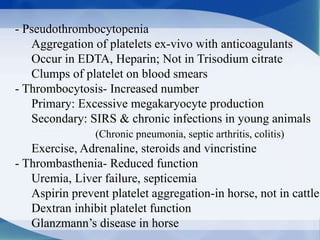
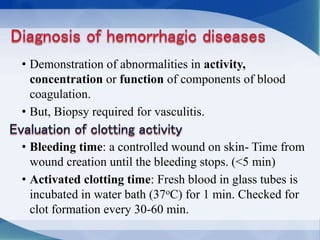
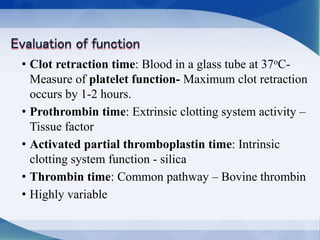
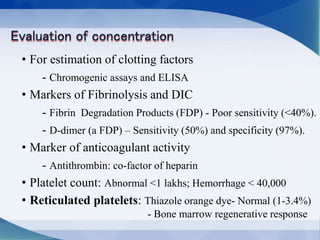
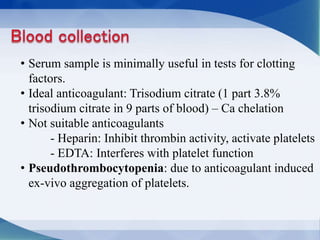
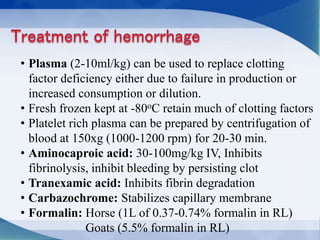
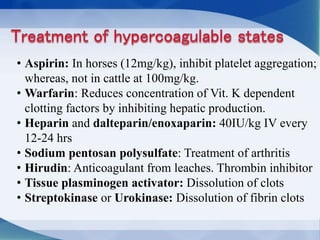
This document discusses hemorrhage in animals, which can occur due to vasculitis, coagulation defects, or platelet disorders. Vasculitis can be caused by infectious diseases damaging blood vessel endothelium. Coagulation defects can be acquired from intoxications impairing clotting factor production or function, or congenital like hemophilia. Platelet disorders include thrombocytopenia from decreased production or increased destruction, and pseudothrombocytopenia seen with some anticoagulants. Various tests can evaluate coagulation and platelet function abnormalities. Treatment depends on the underlying cause but may include plasma transfusion, antifibrinolytic drugs, heparin, or drugs targeting specific clotting defects.