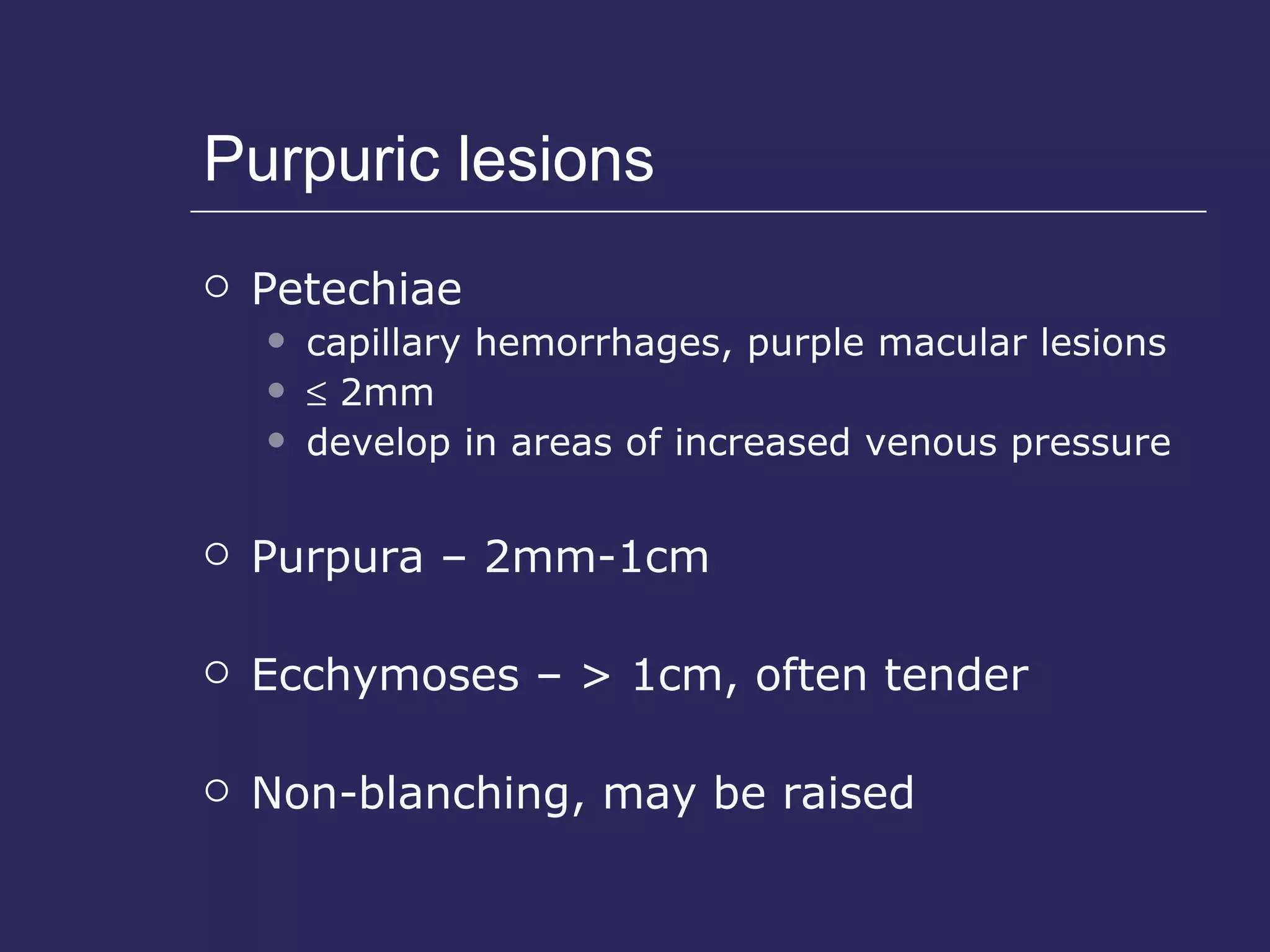
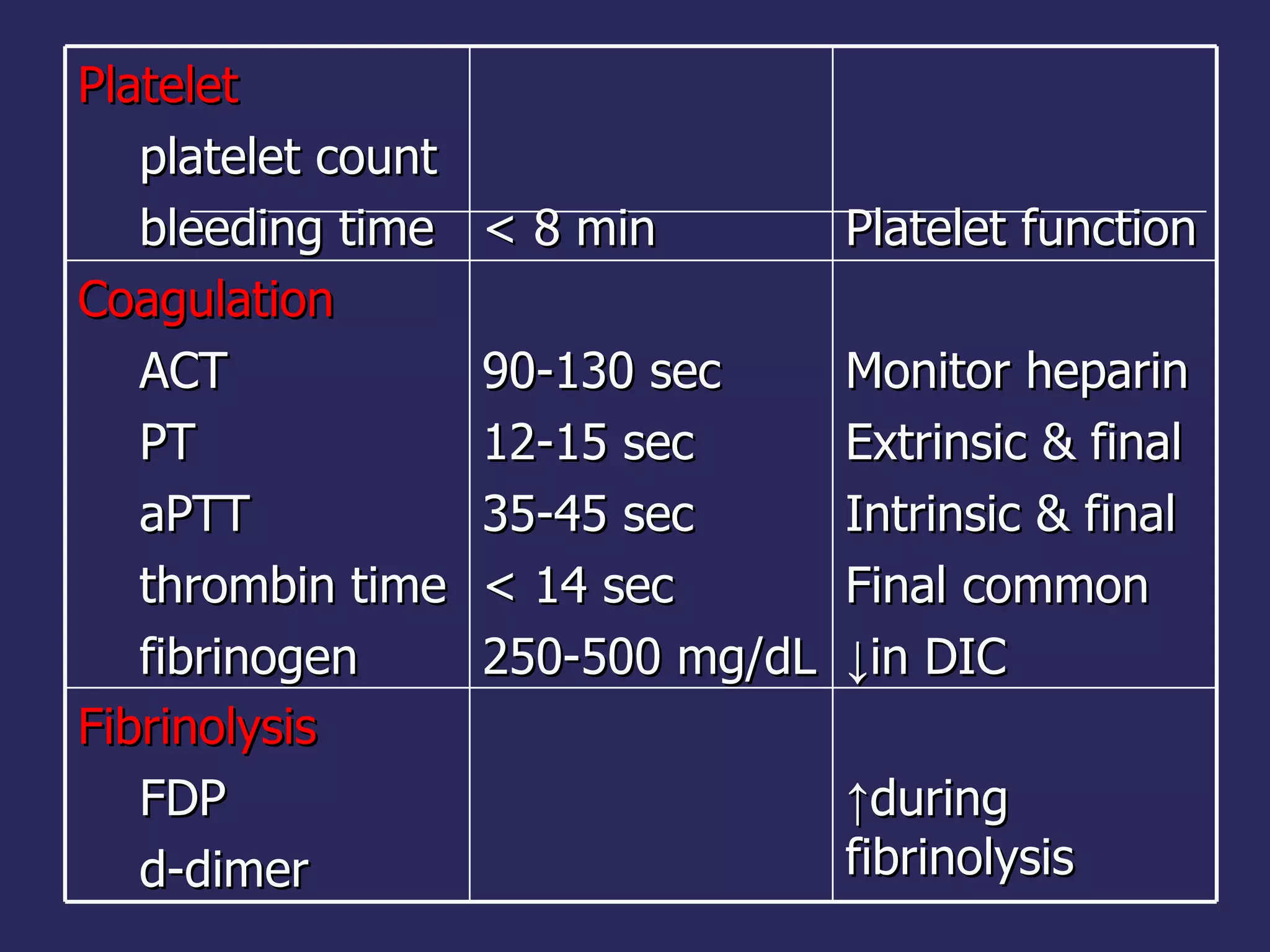
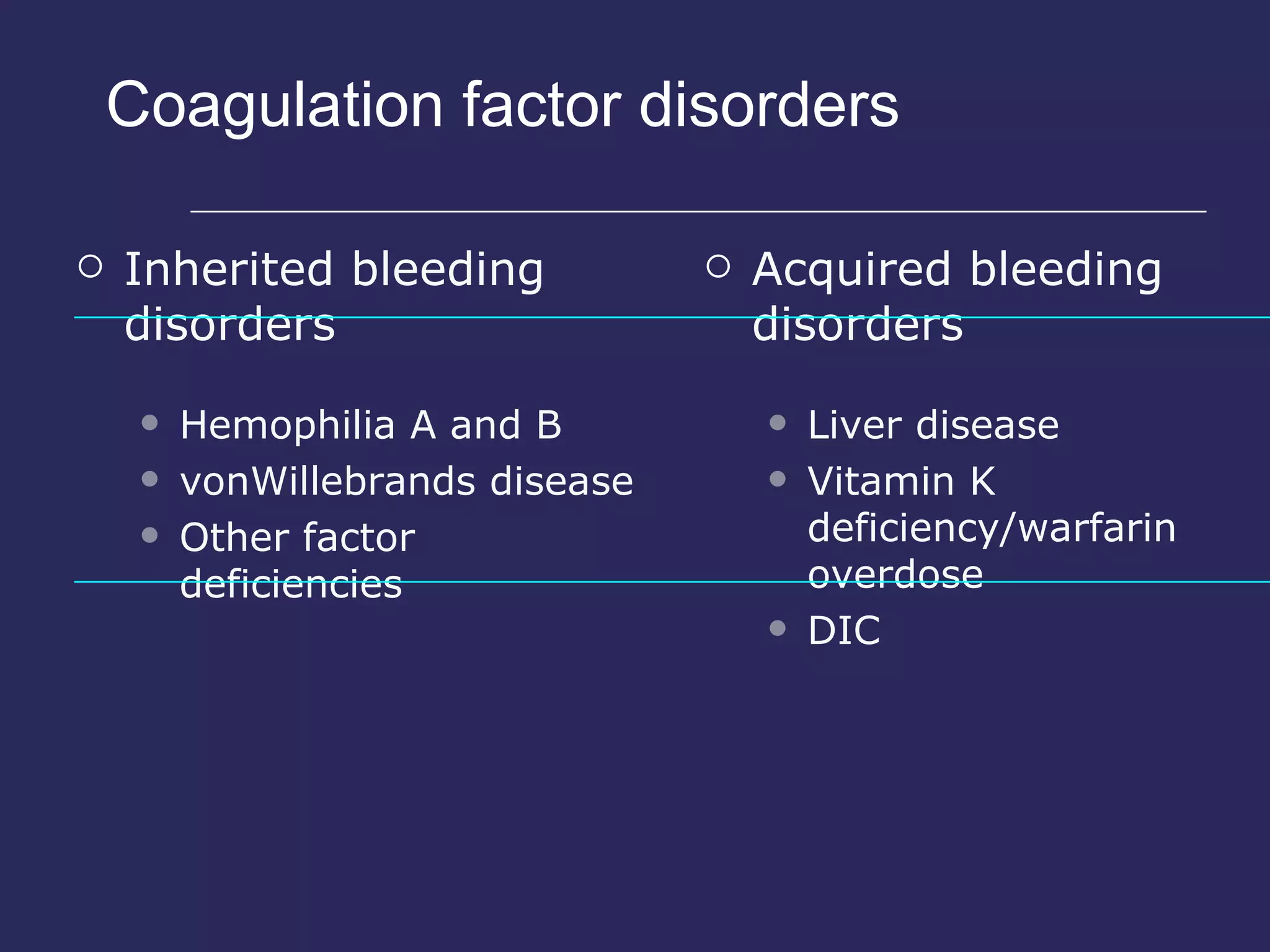
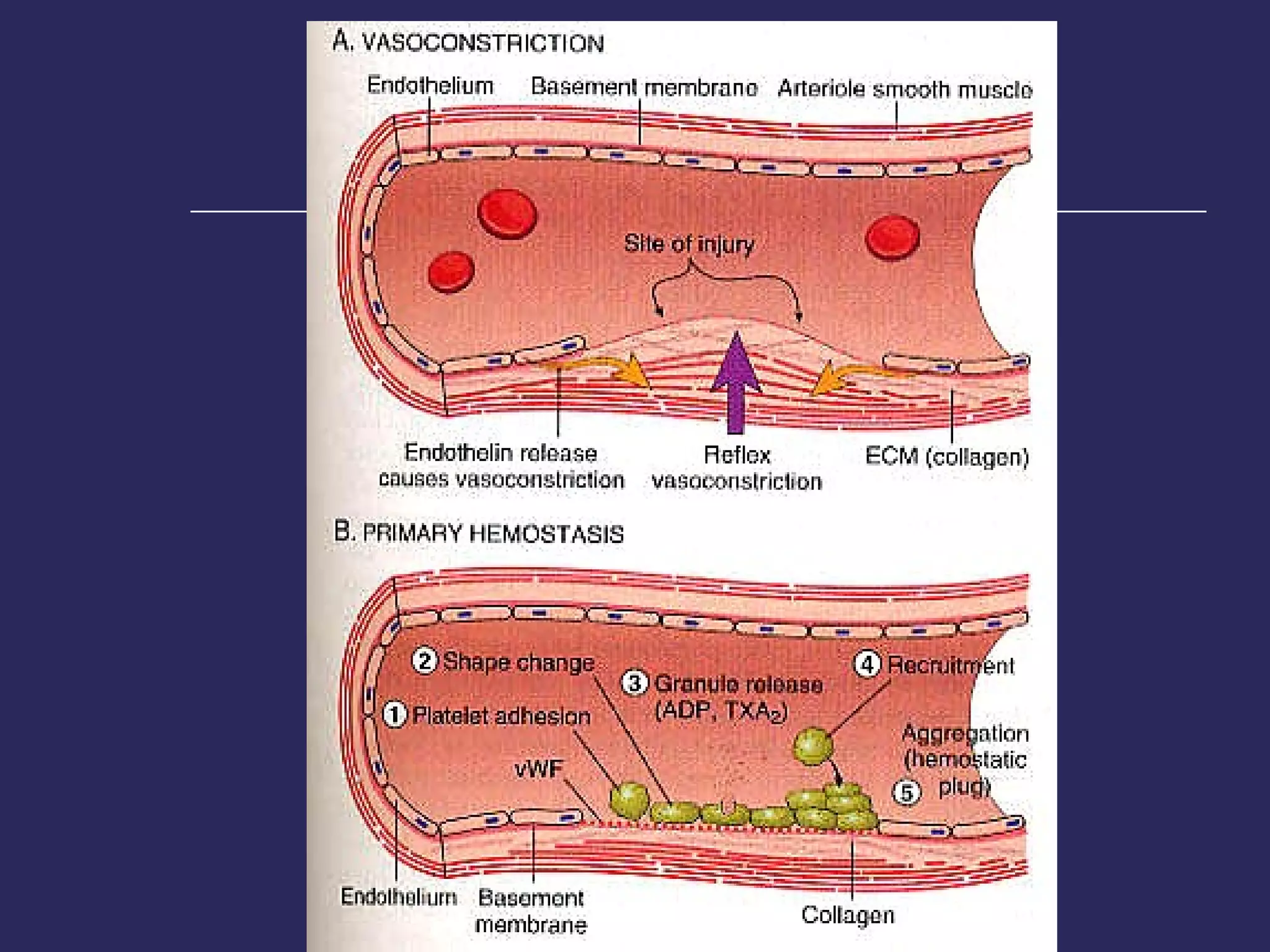
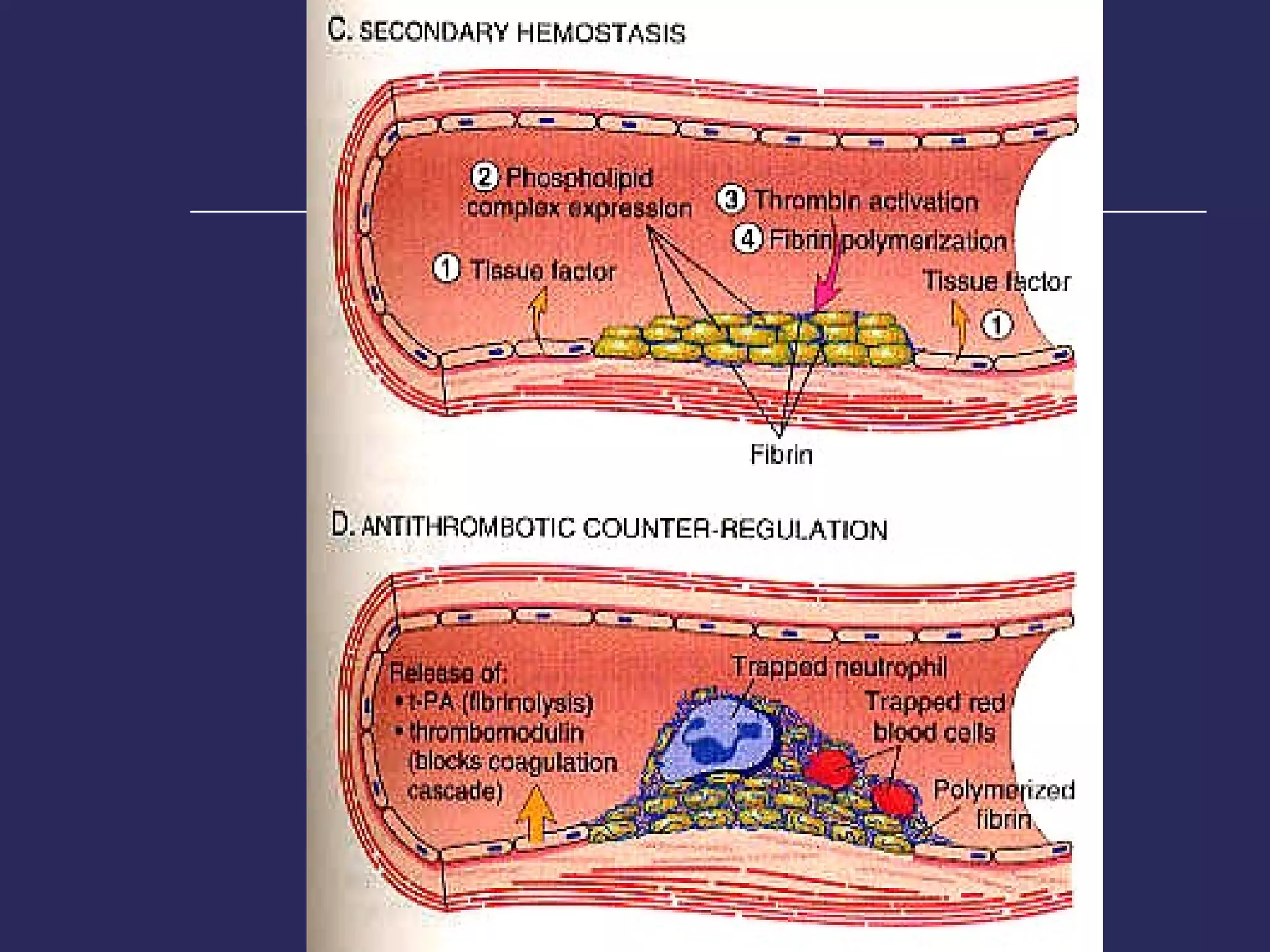
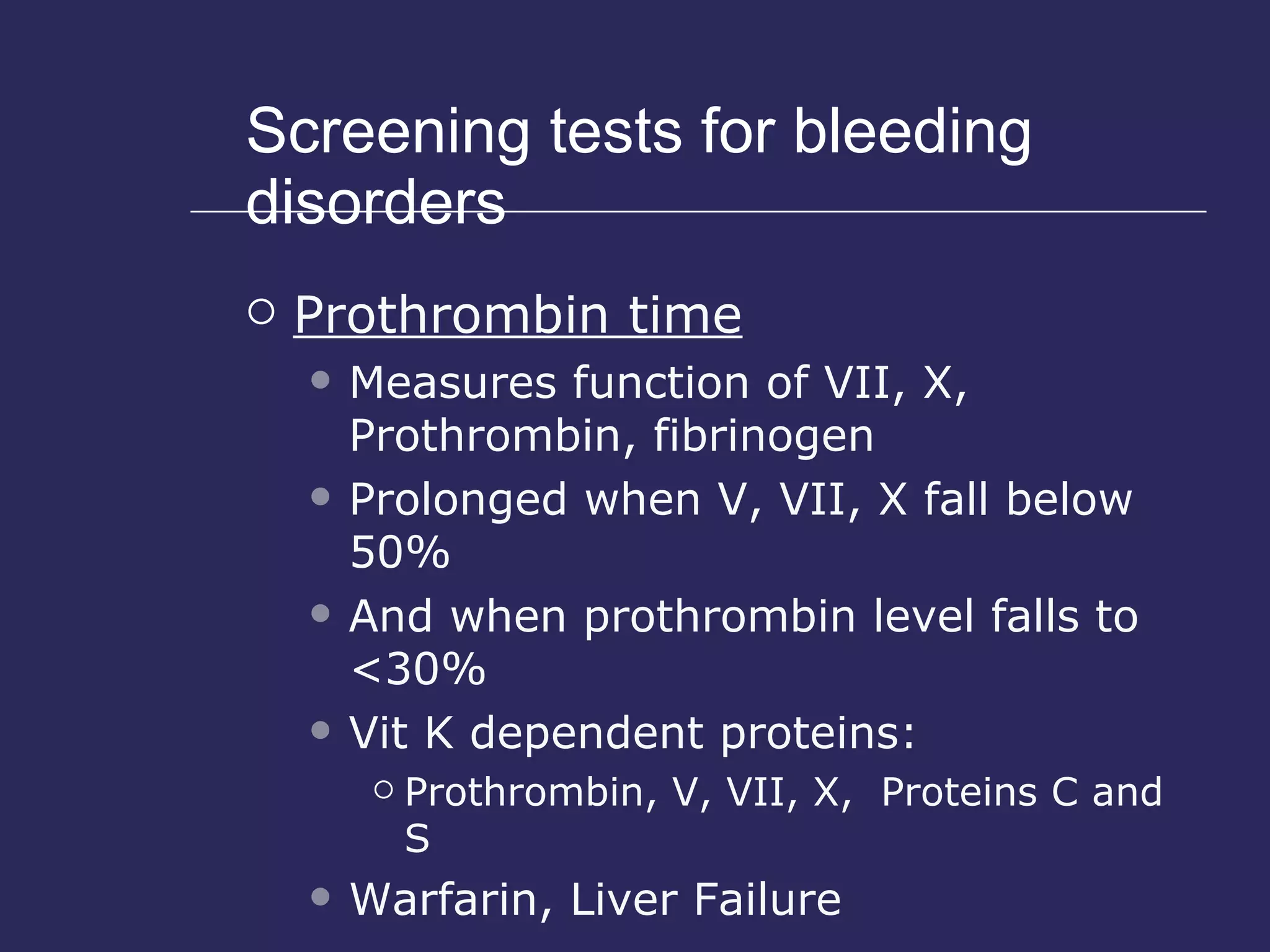
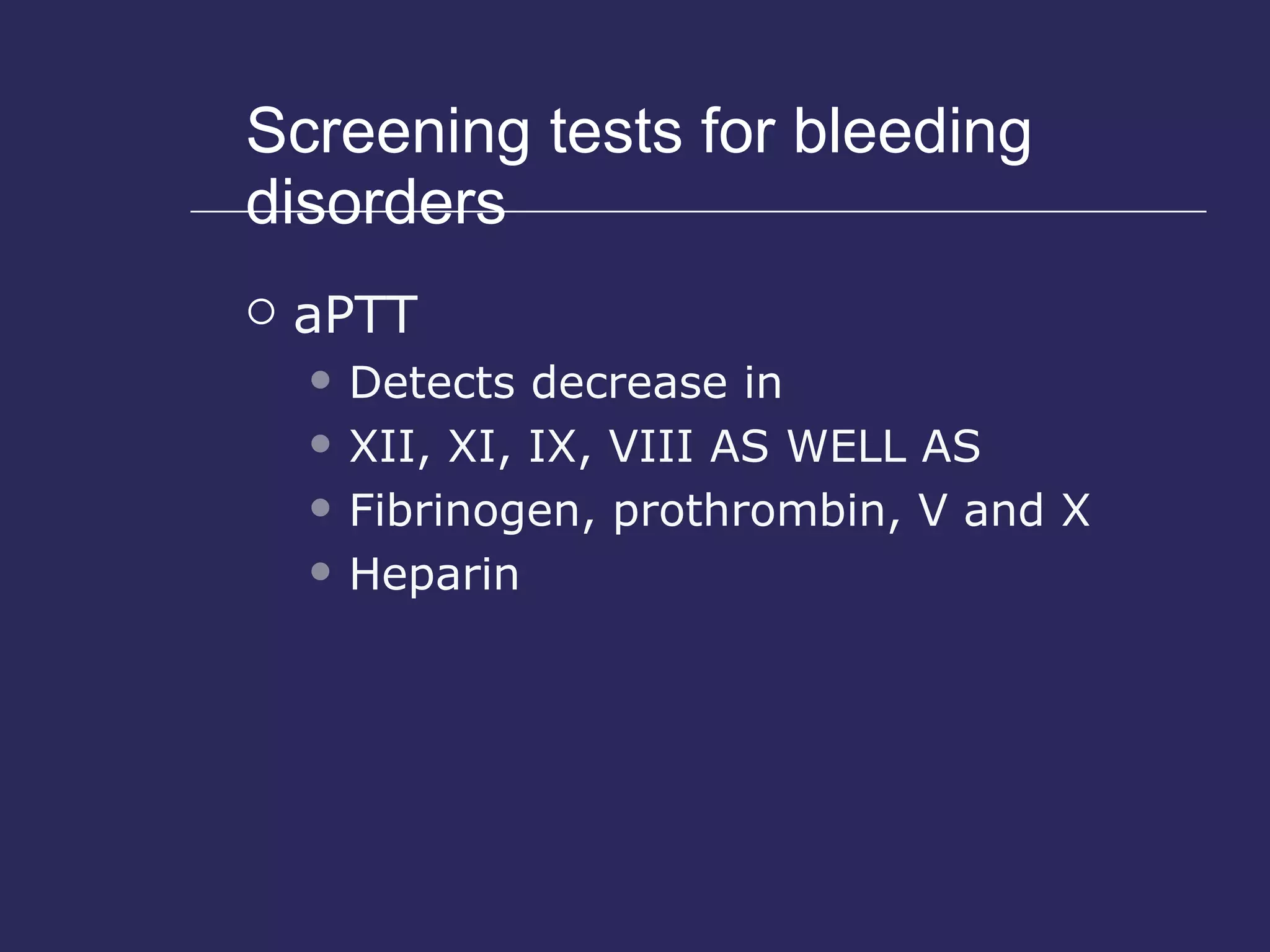
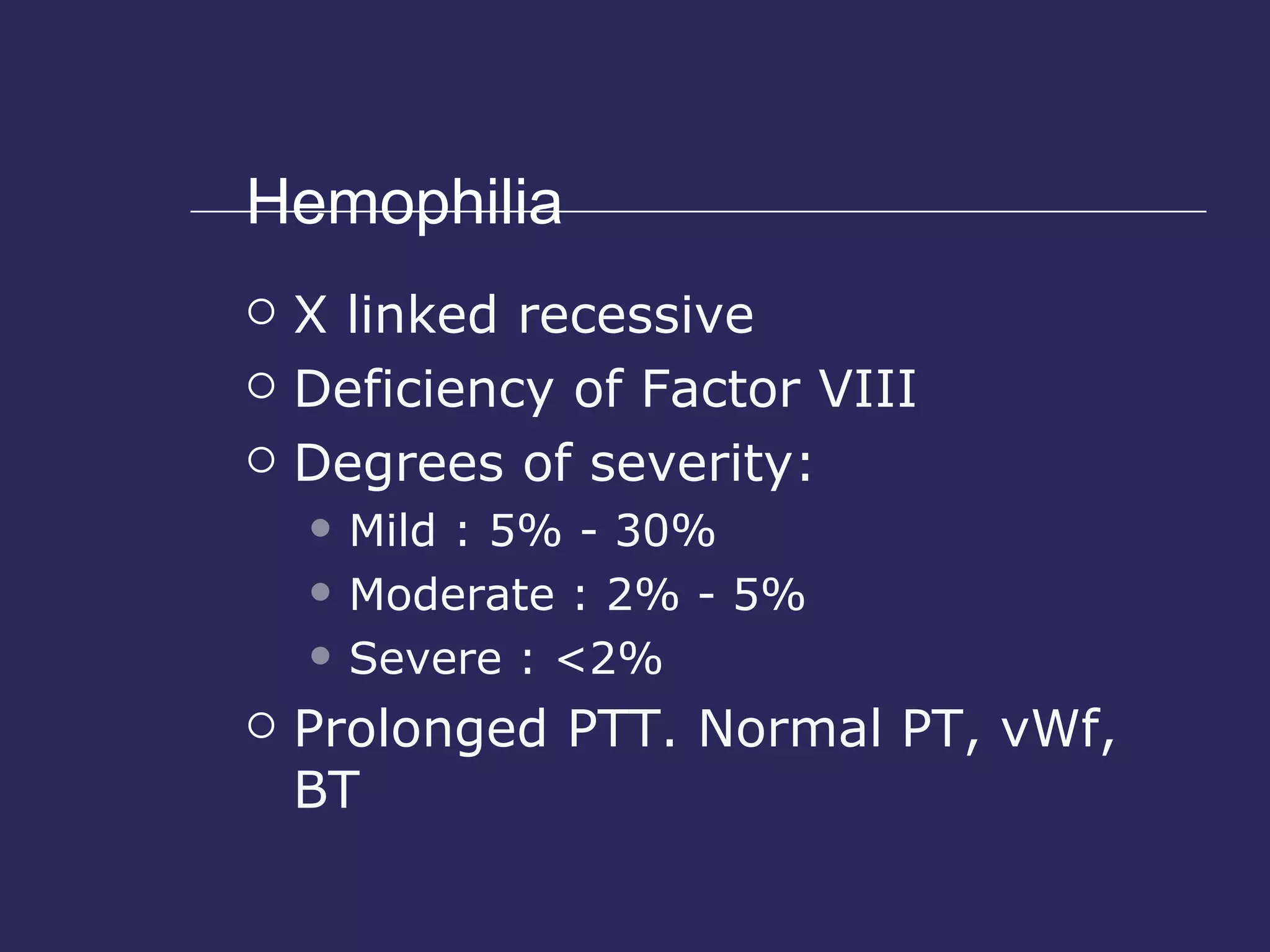
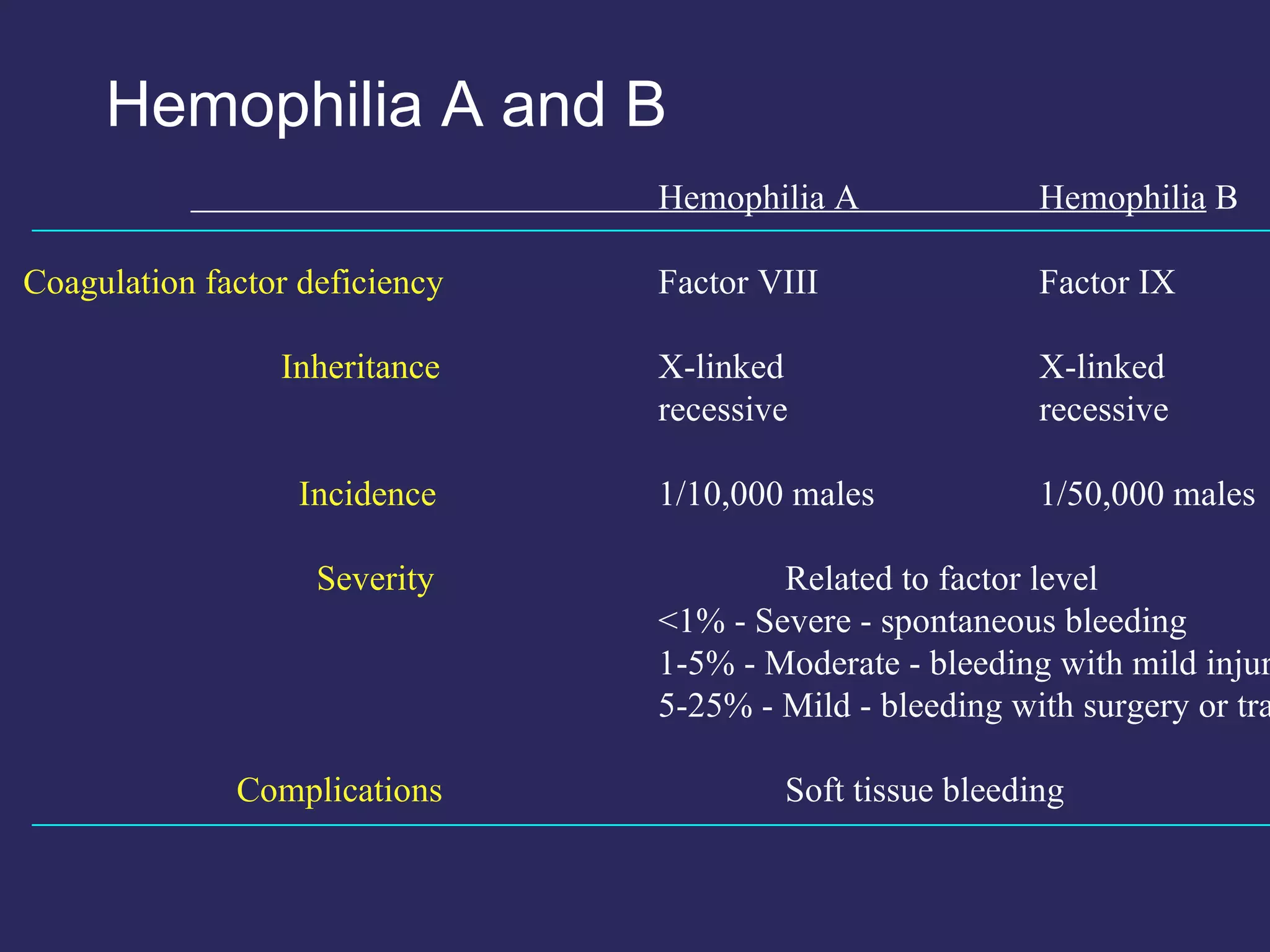
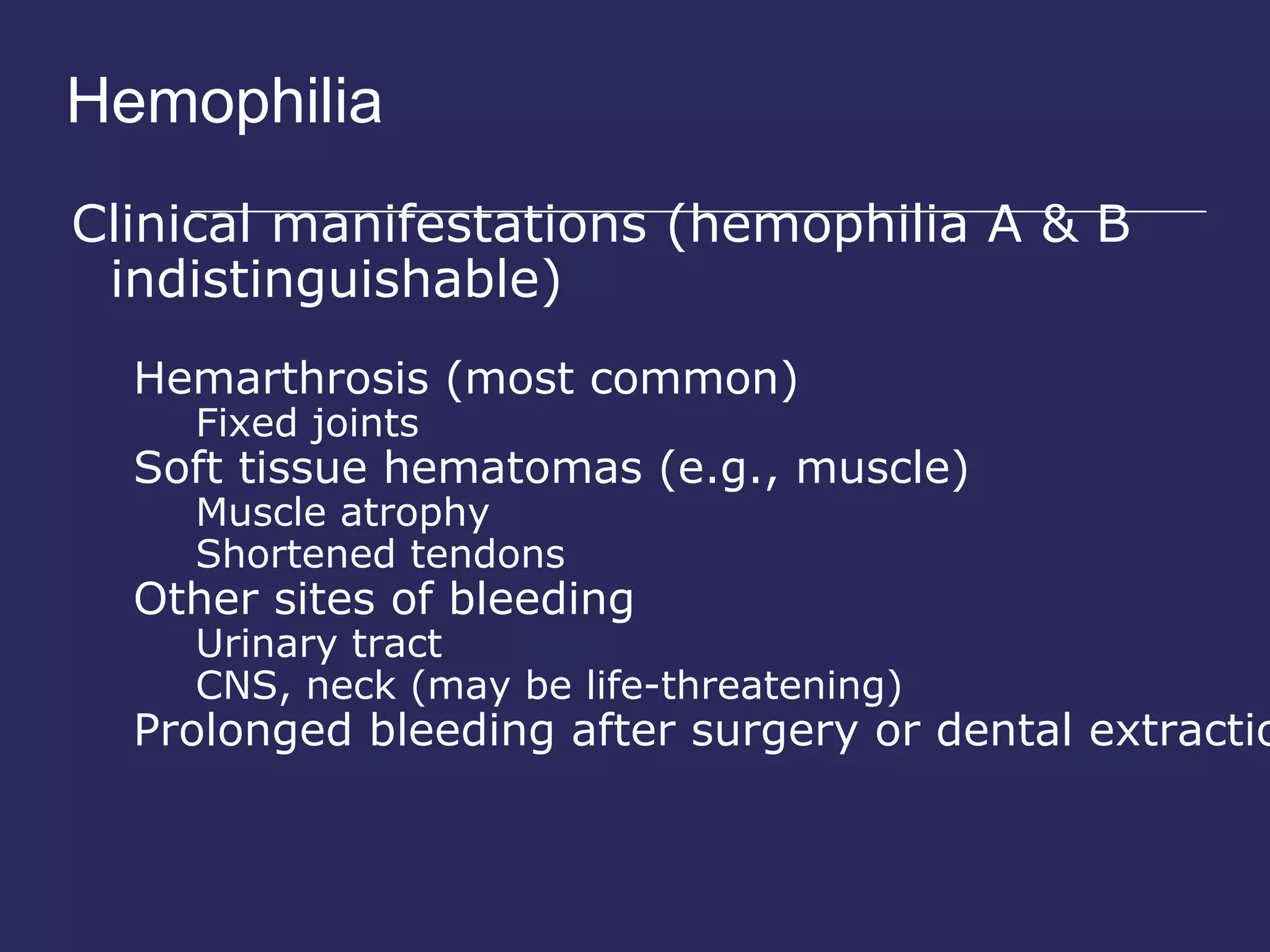
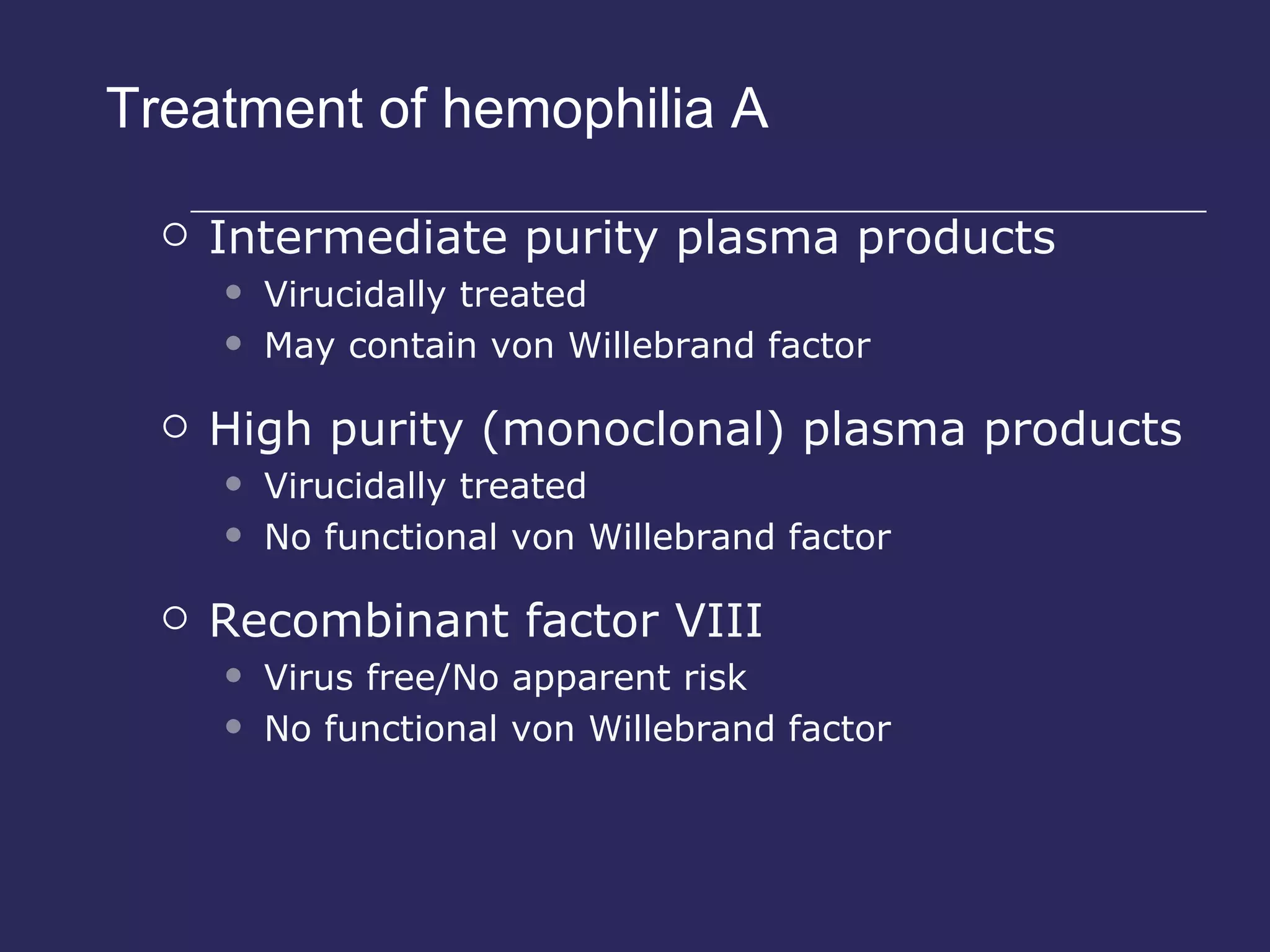
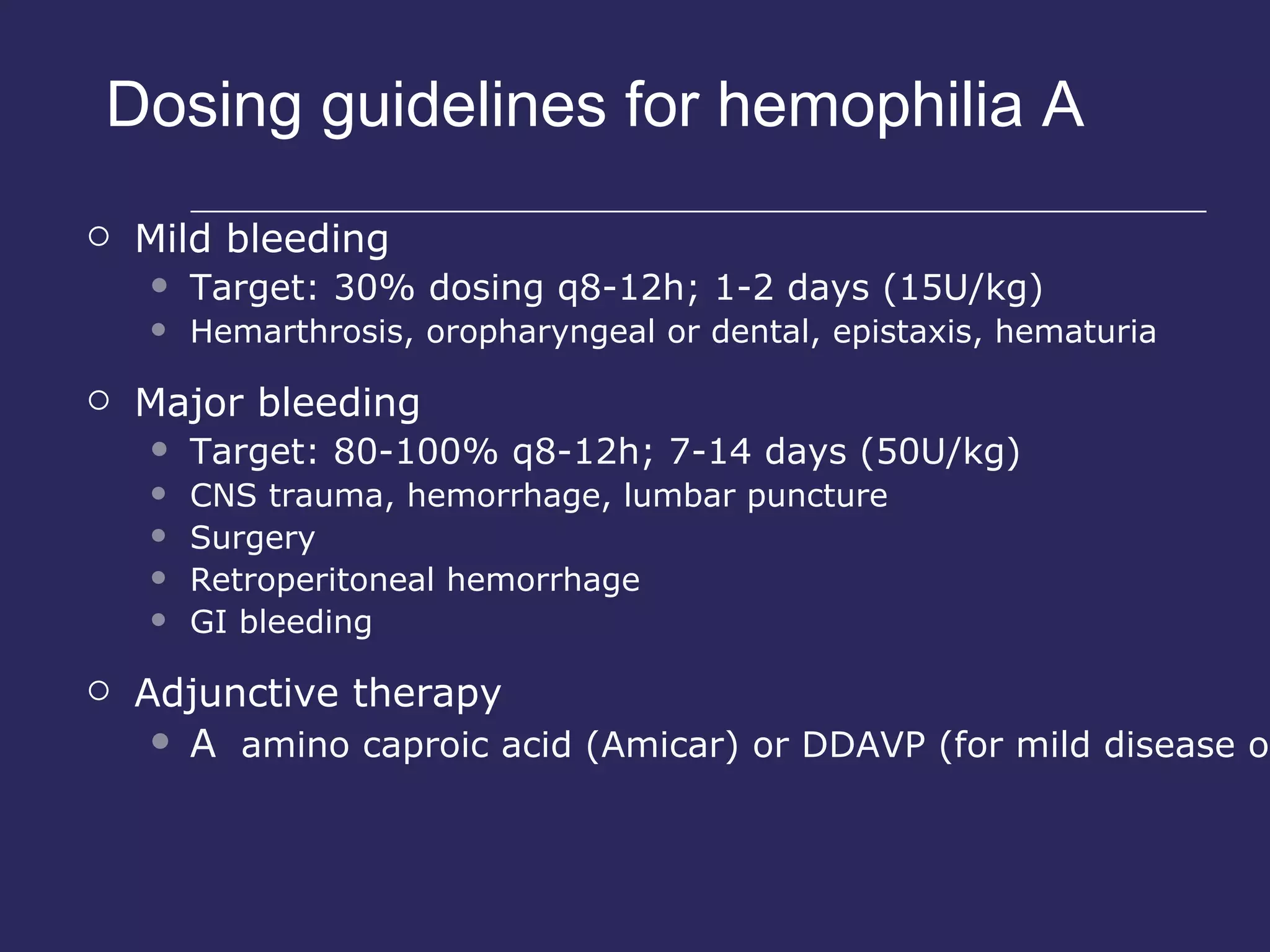
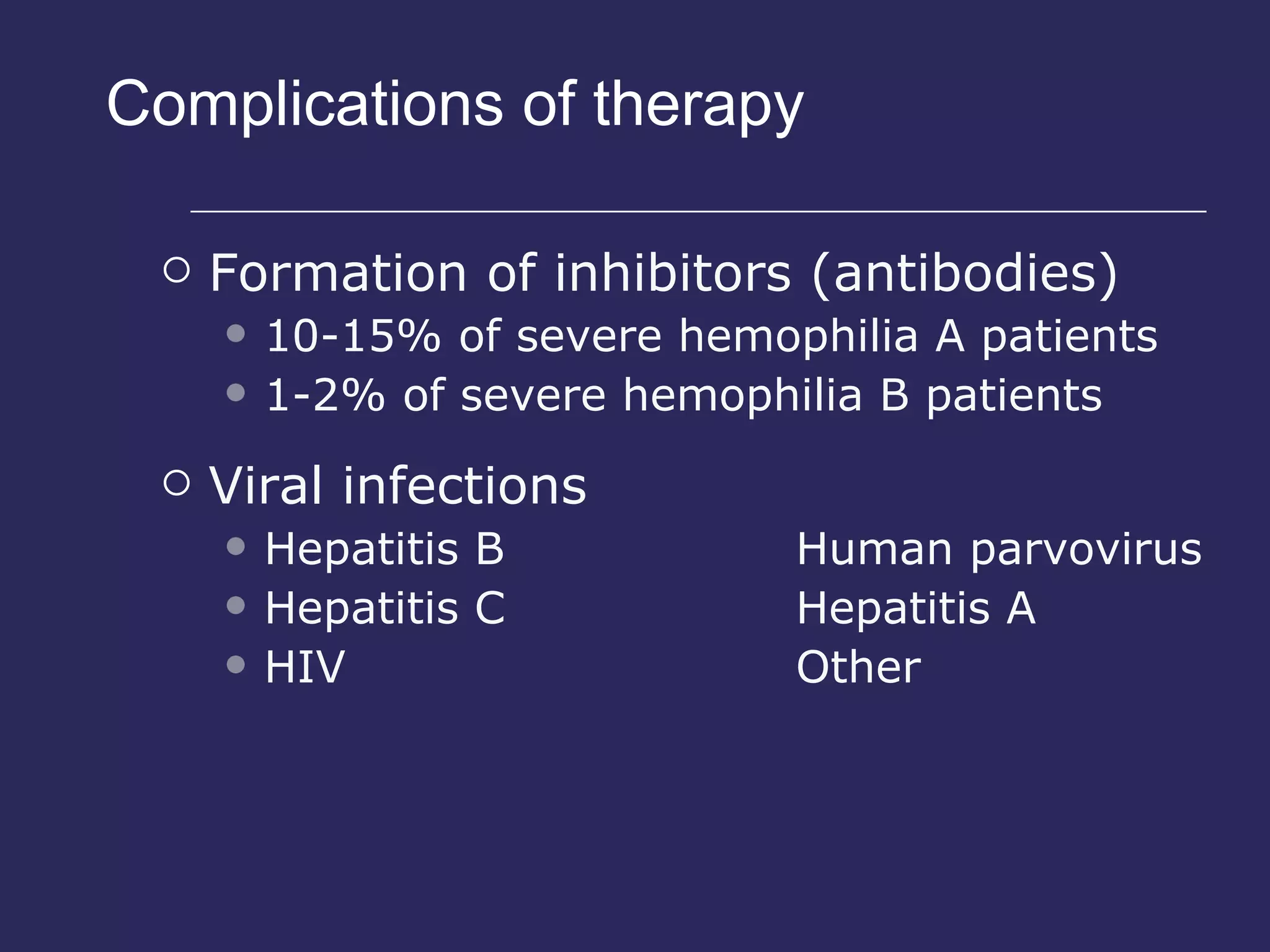
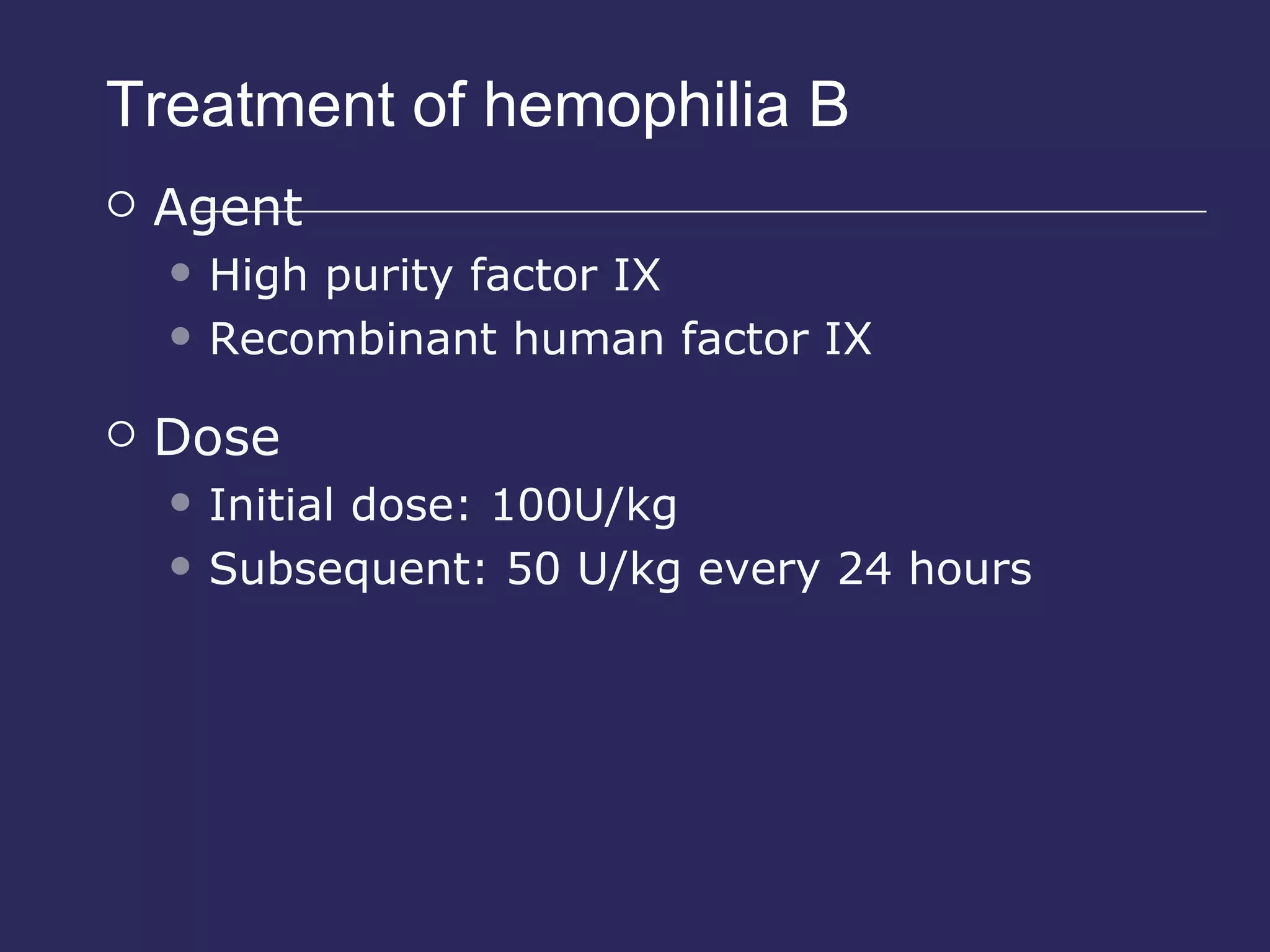
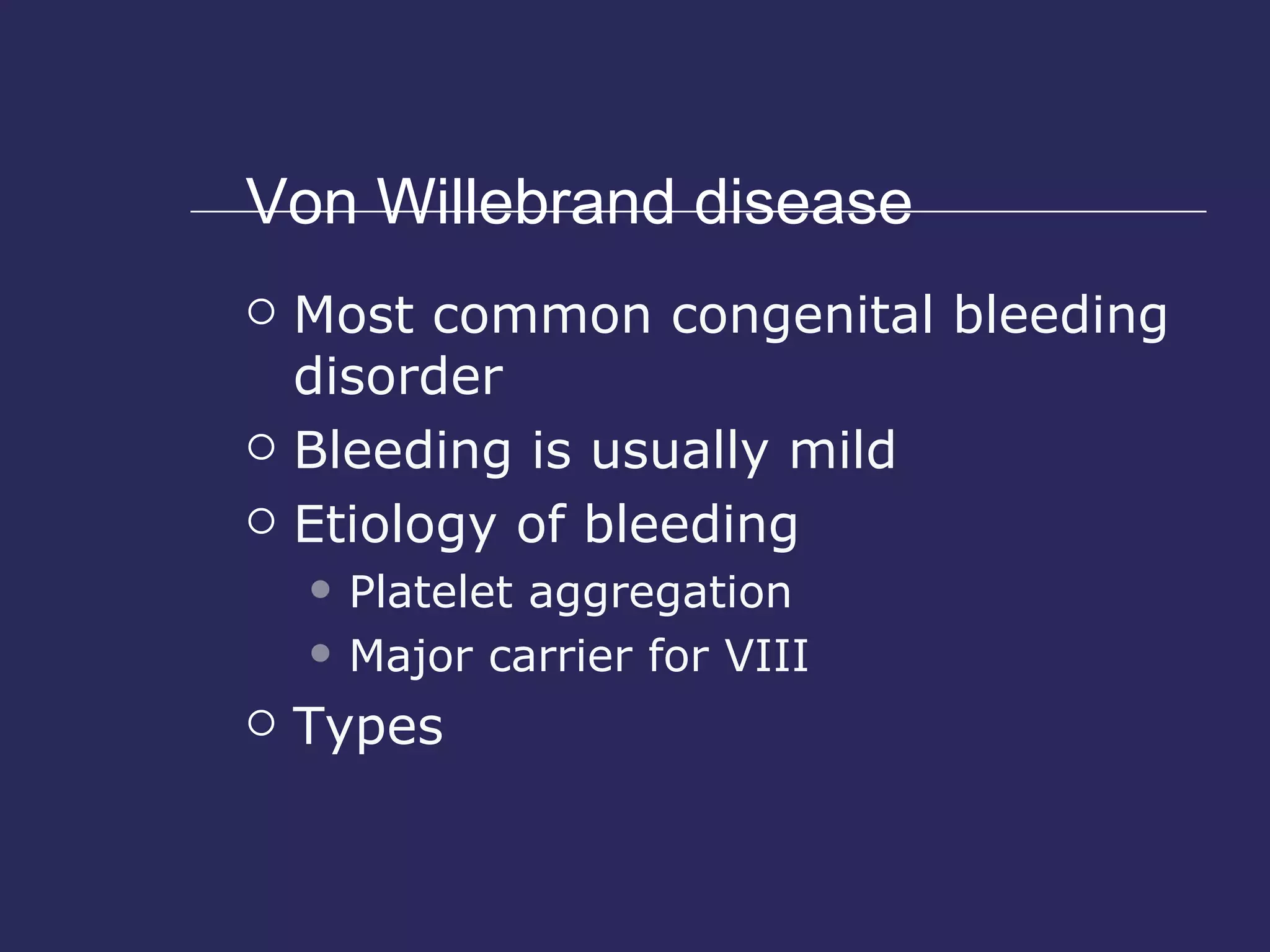
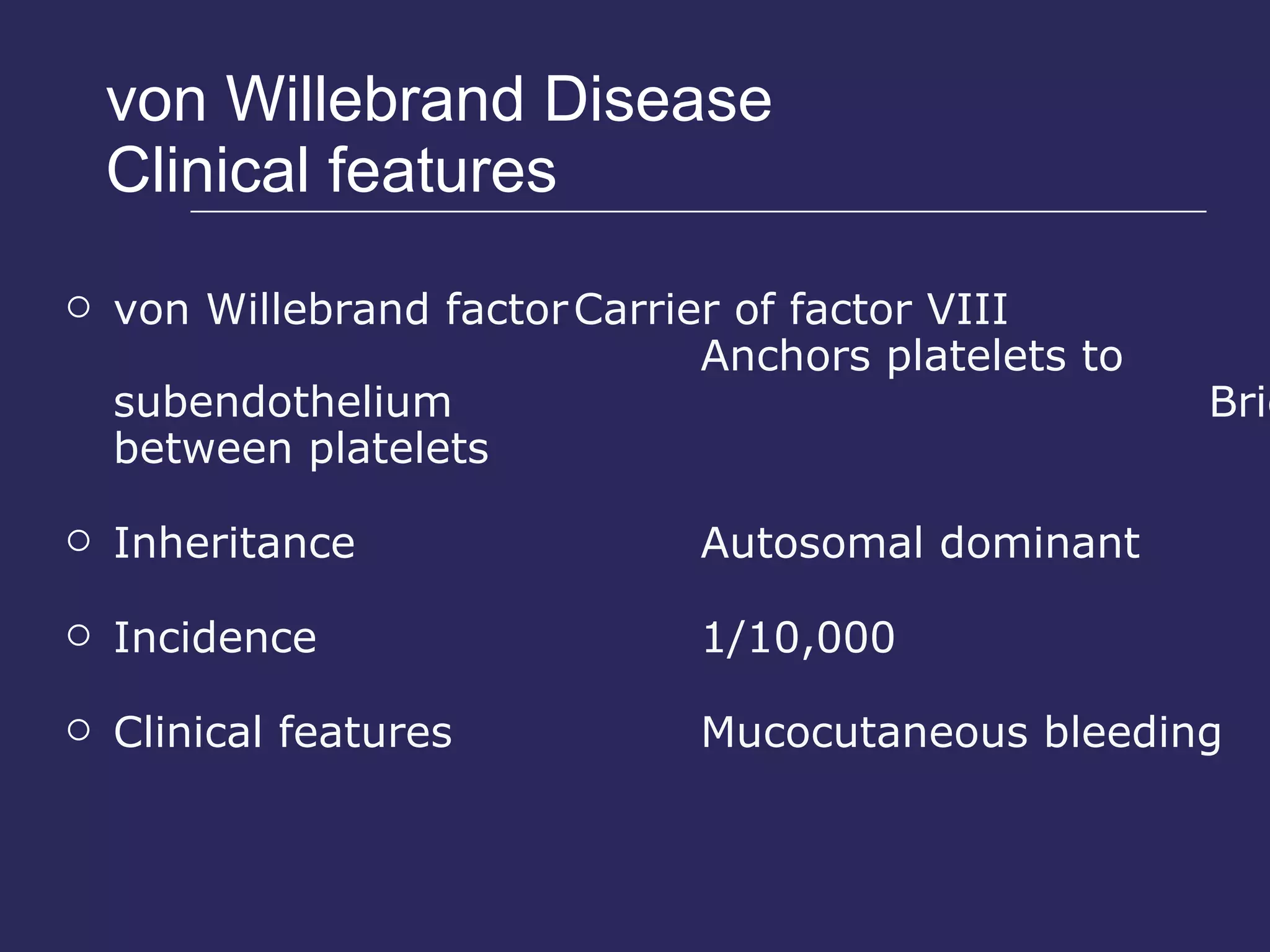
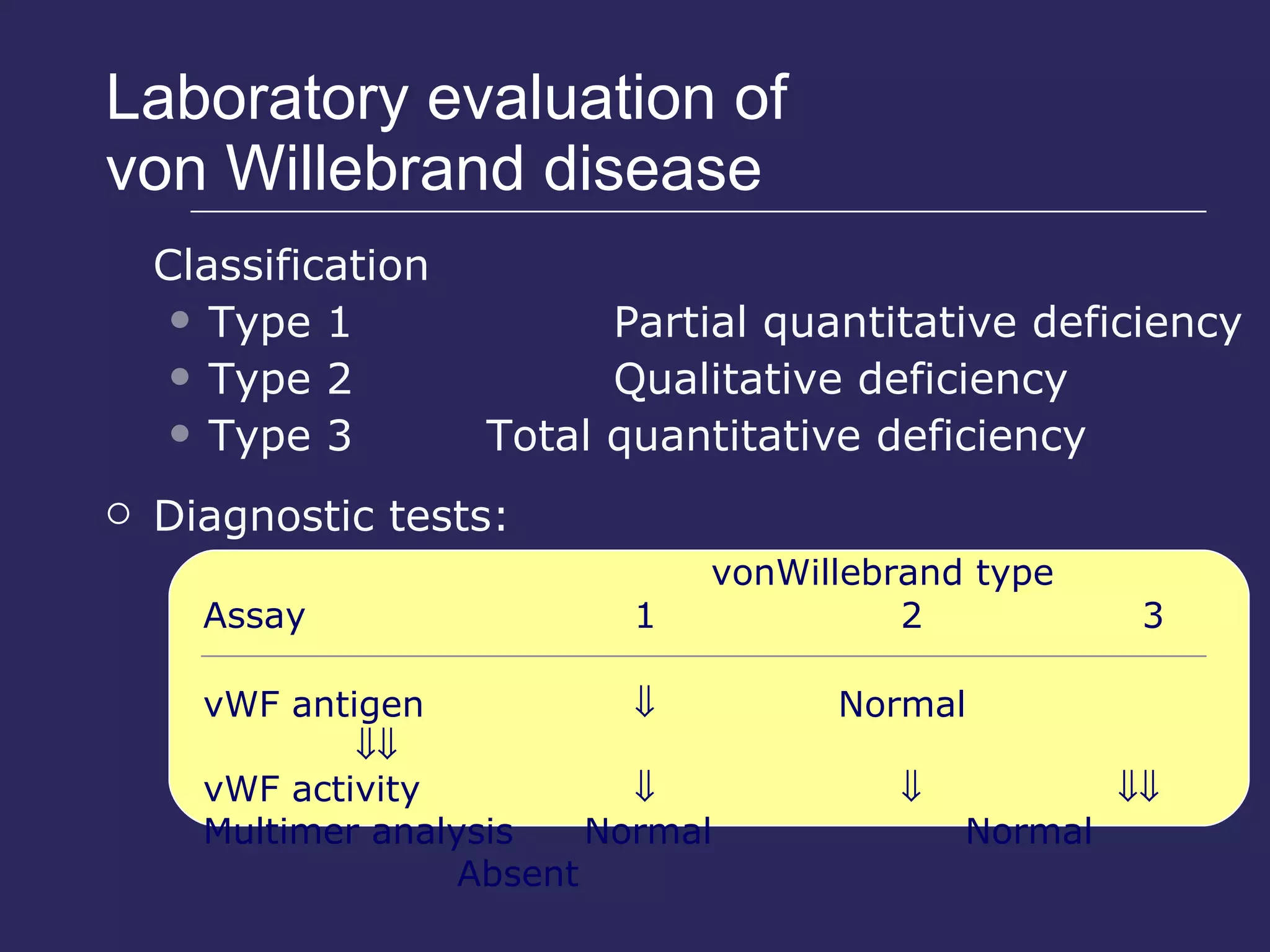
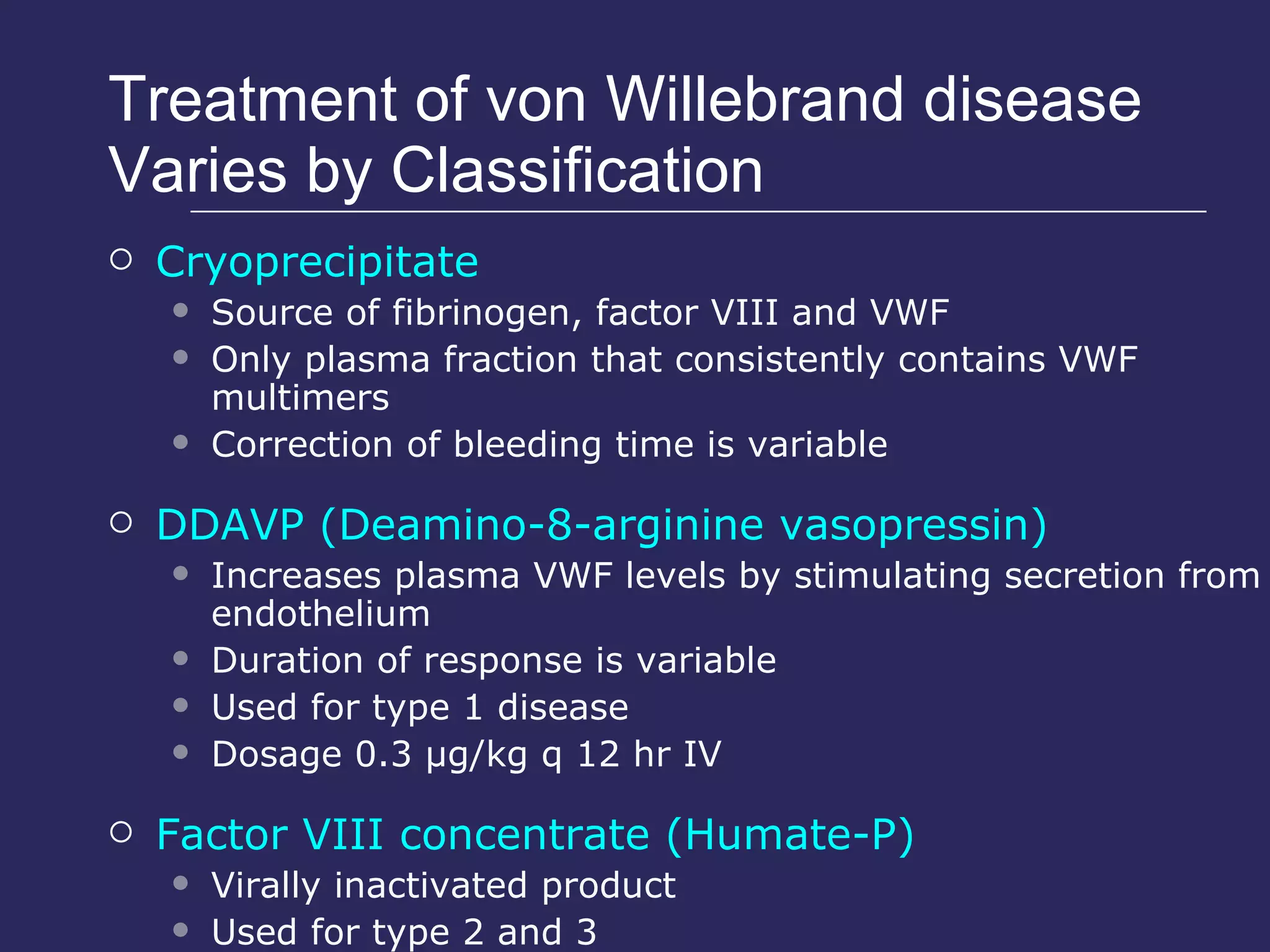
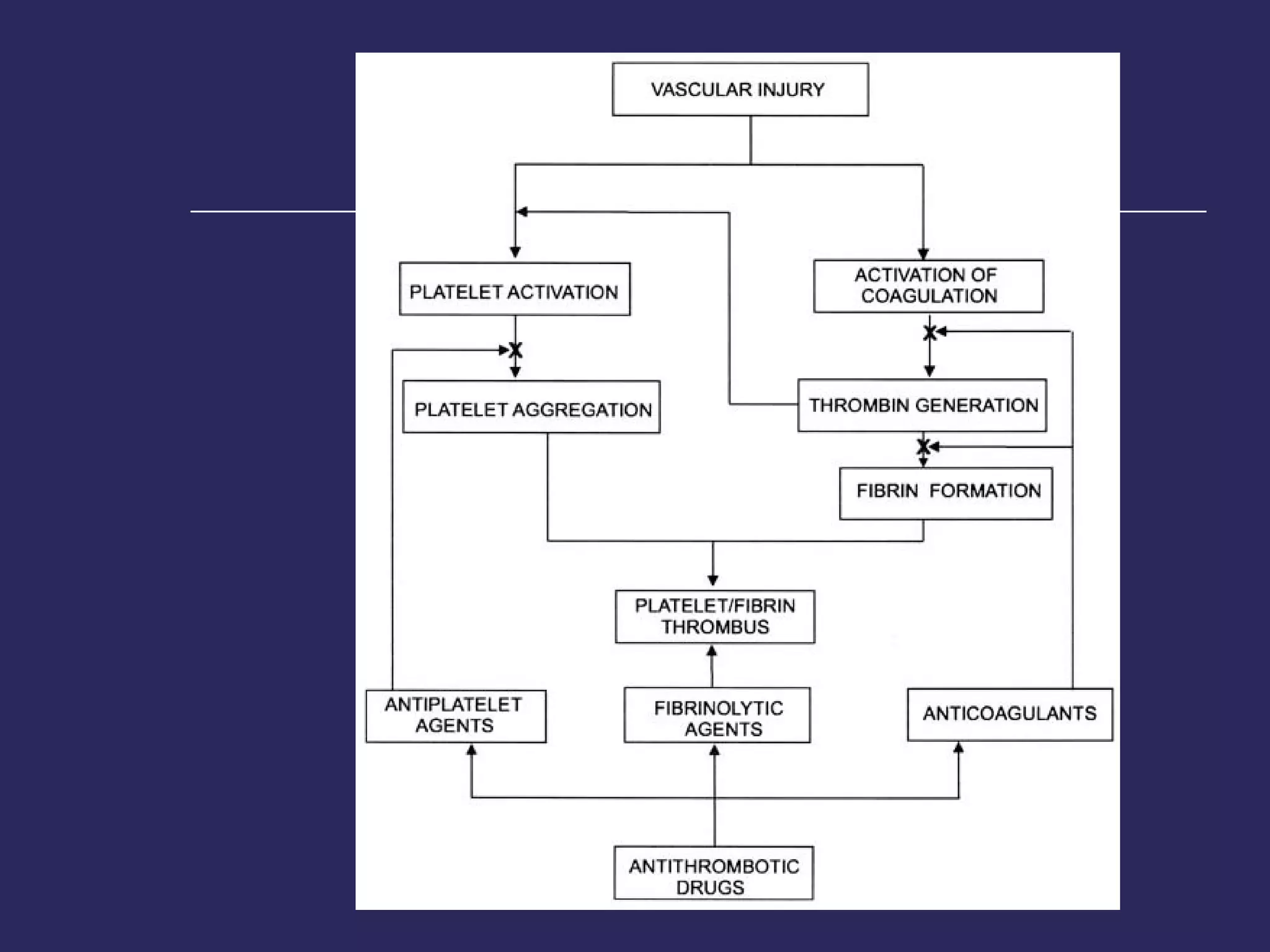
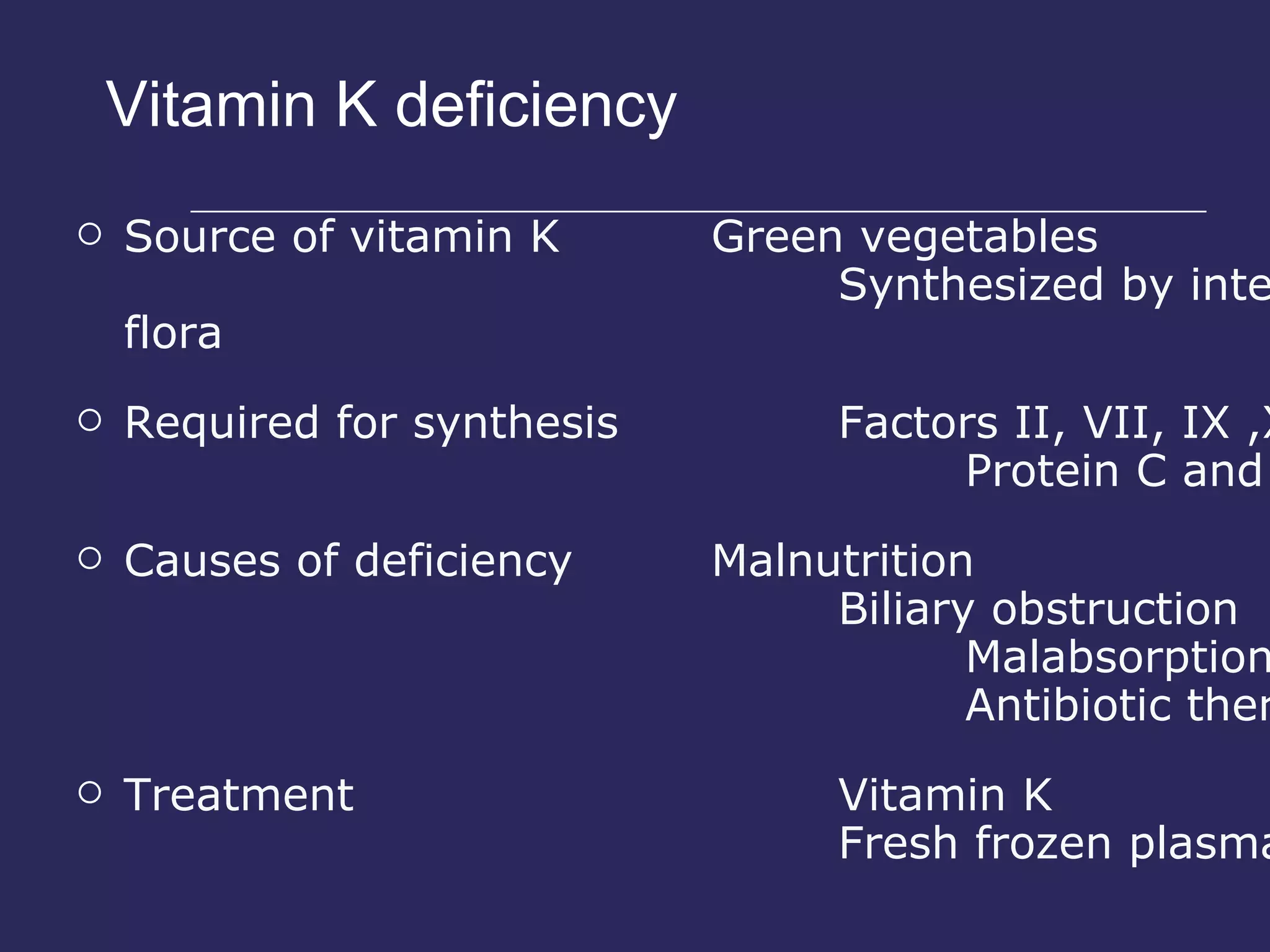
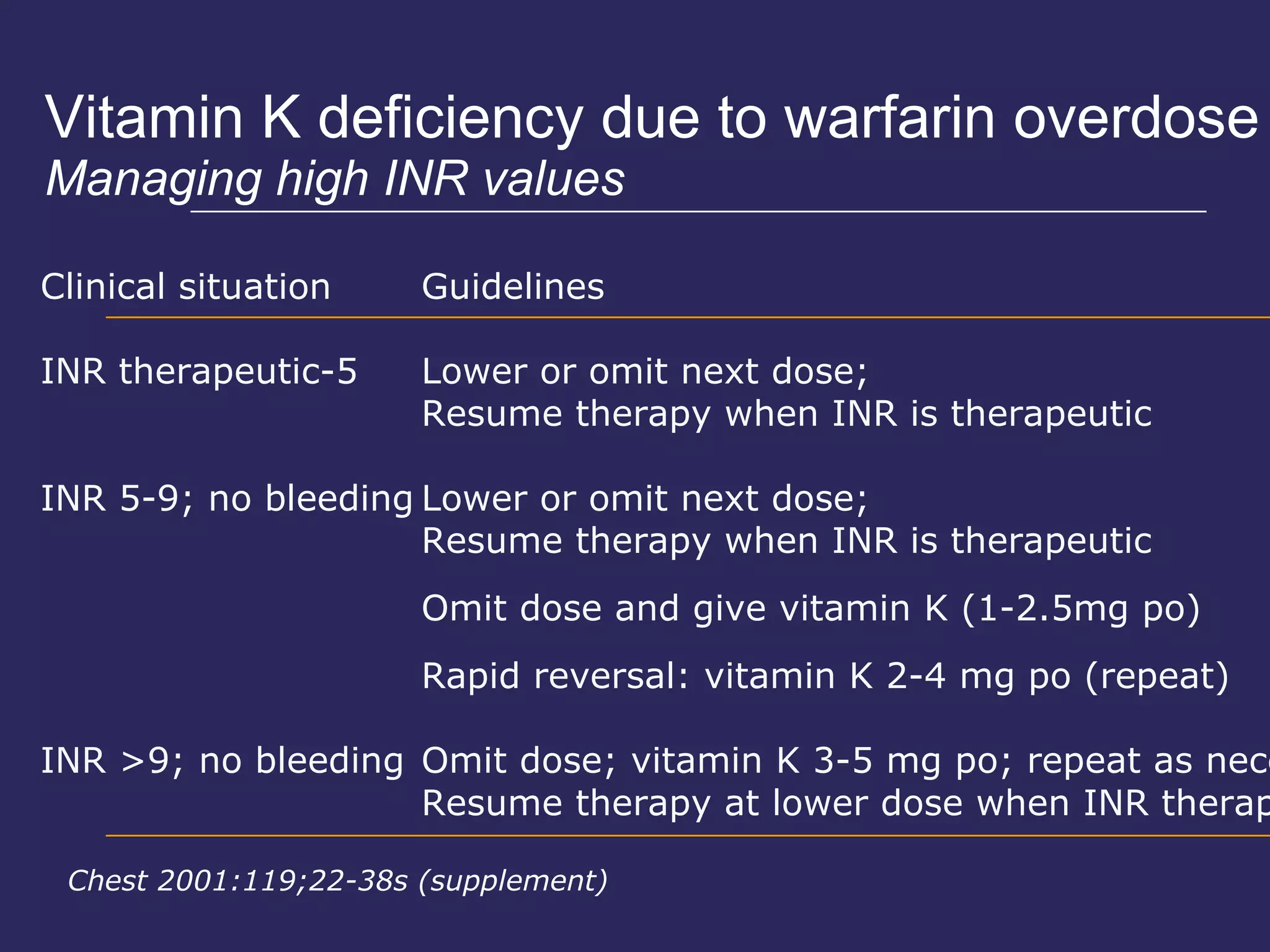
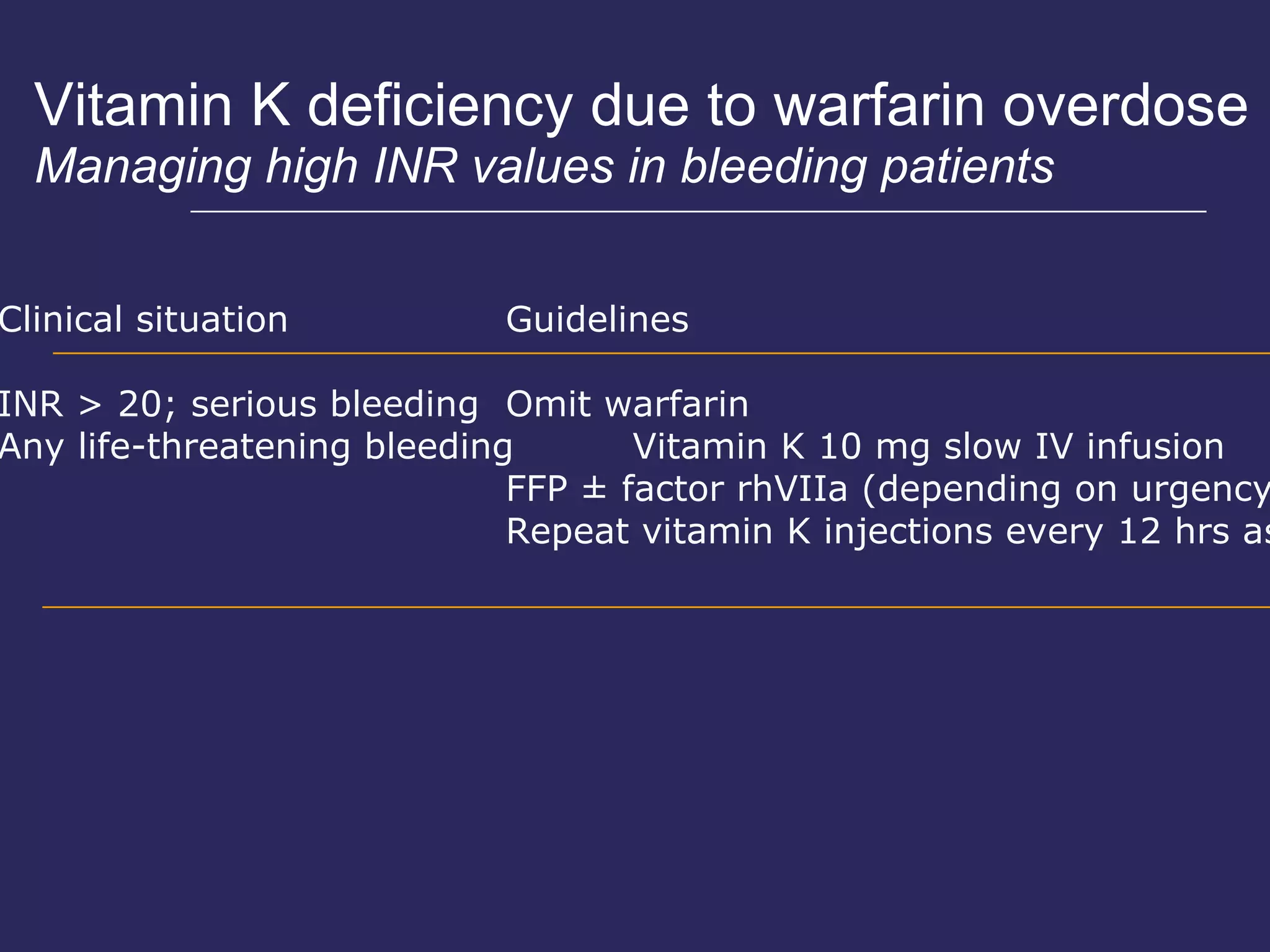
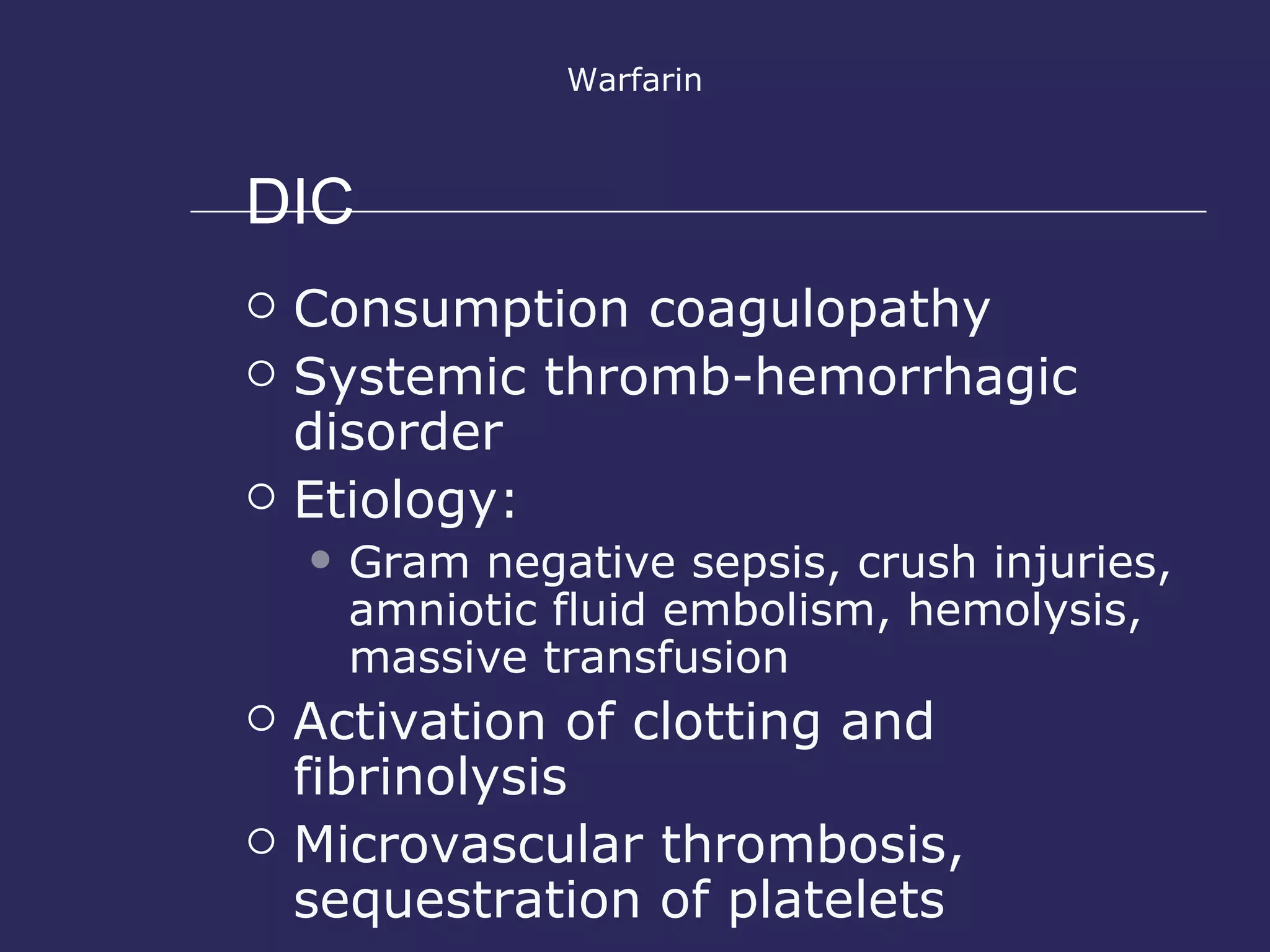
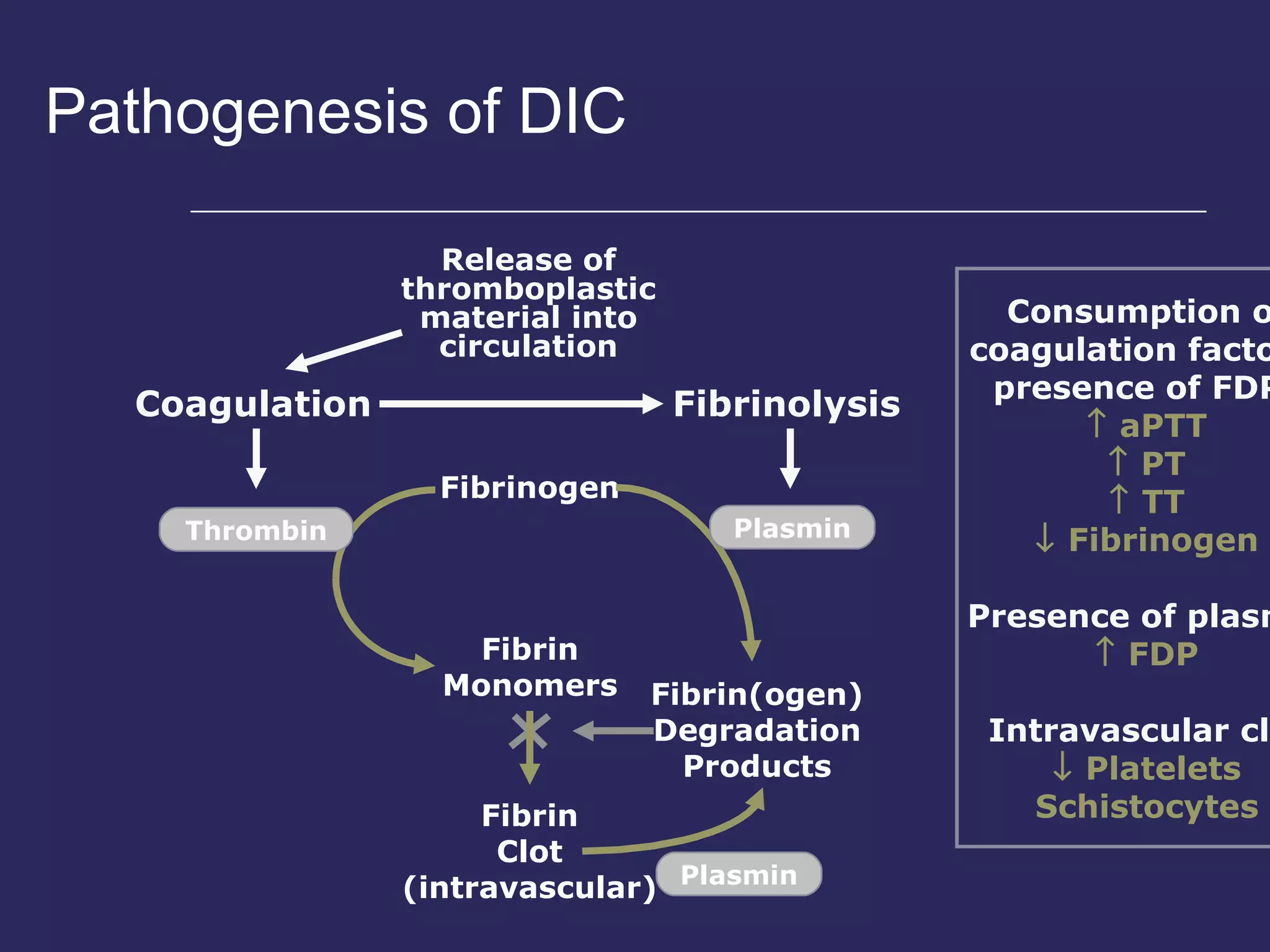
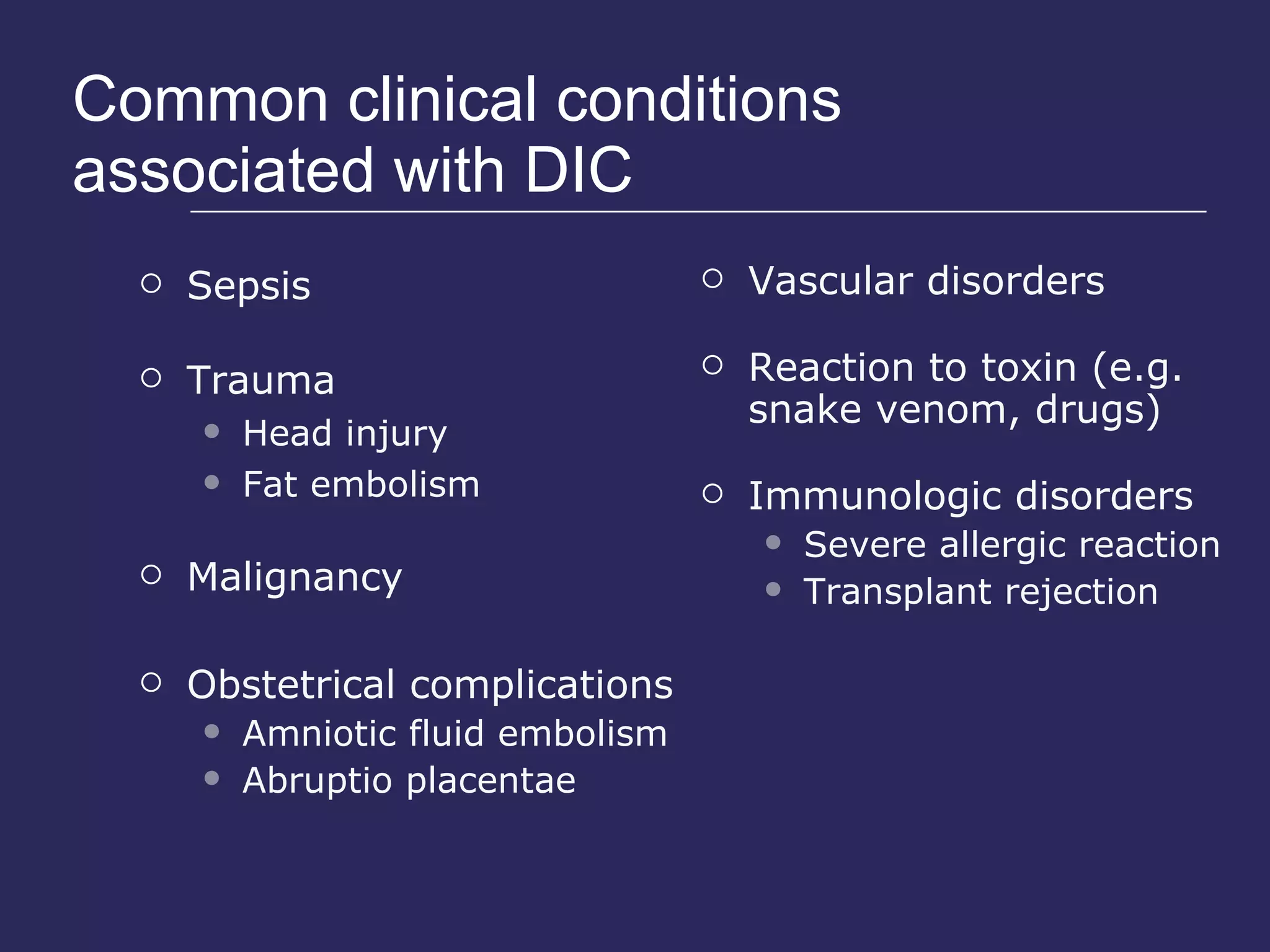
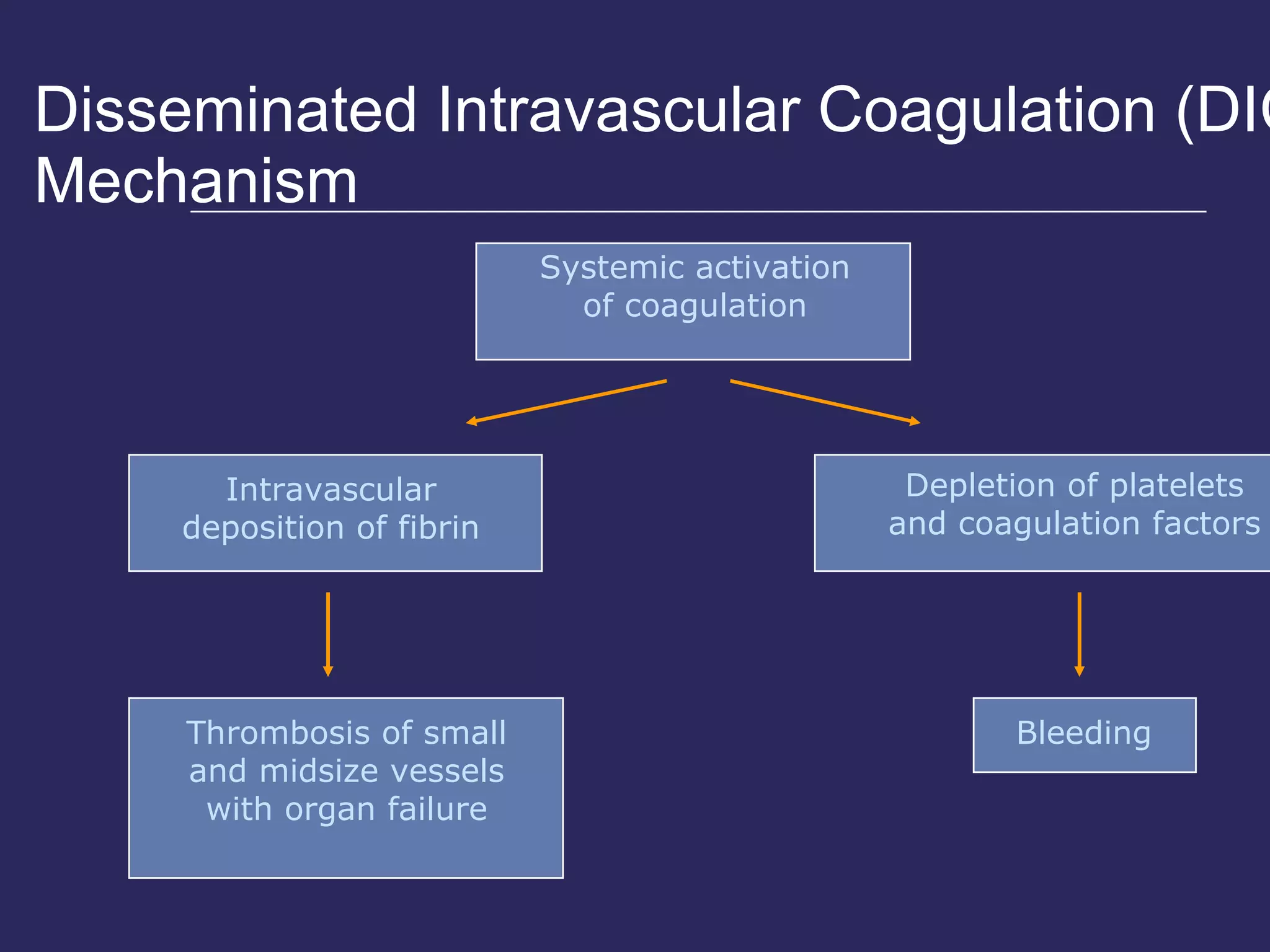
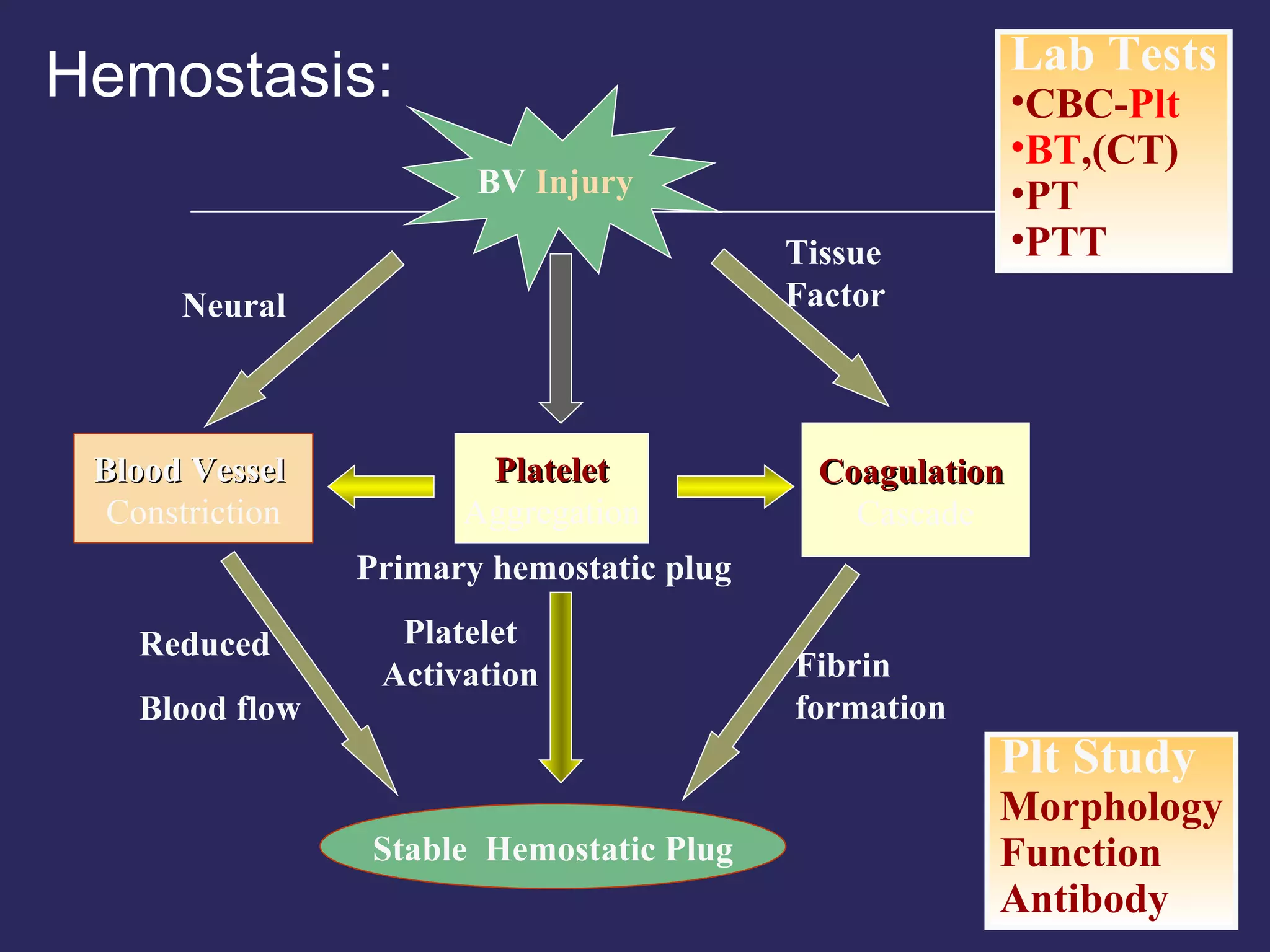
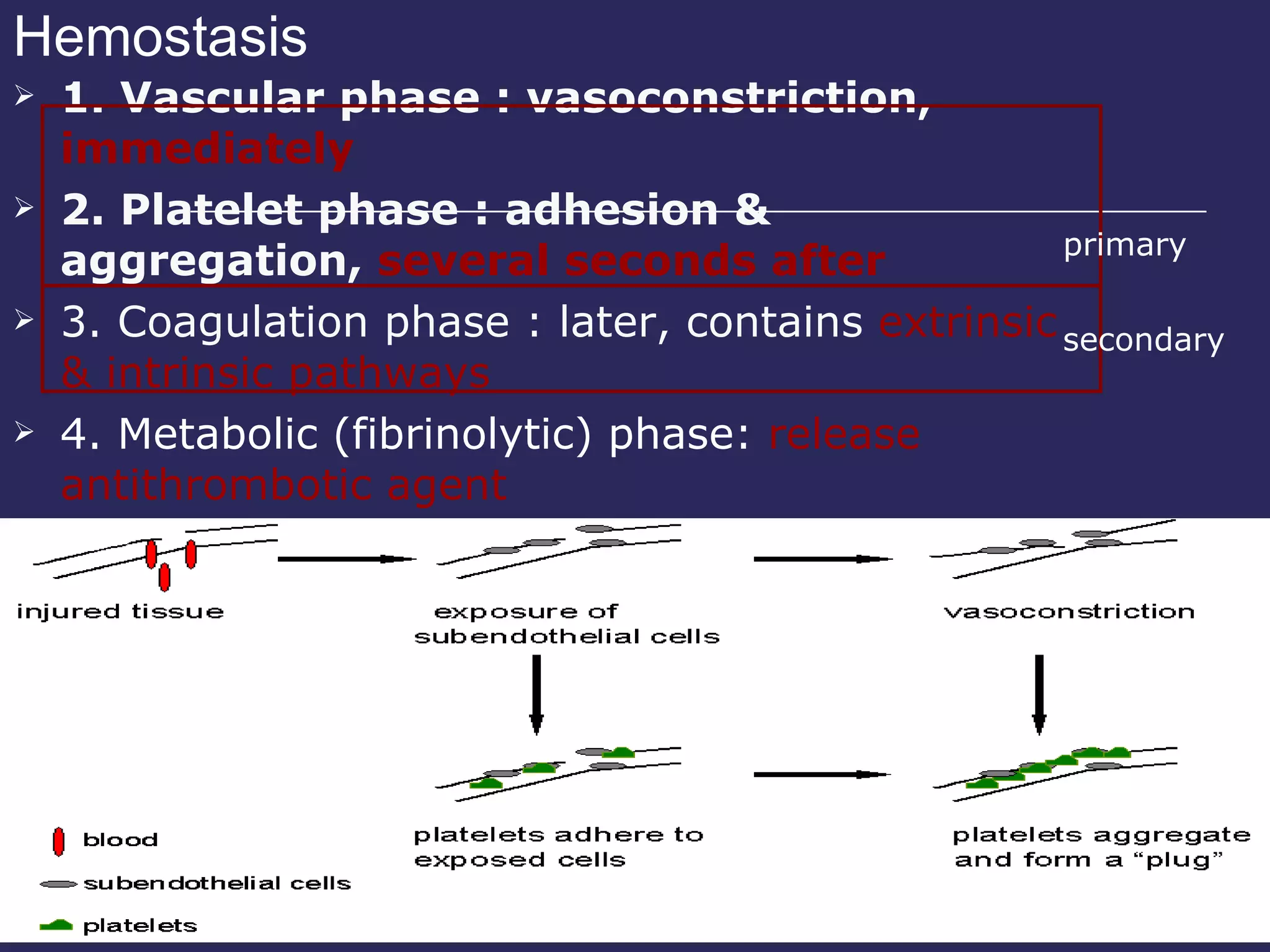
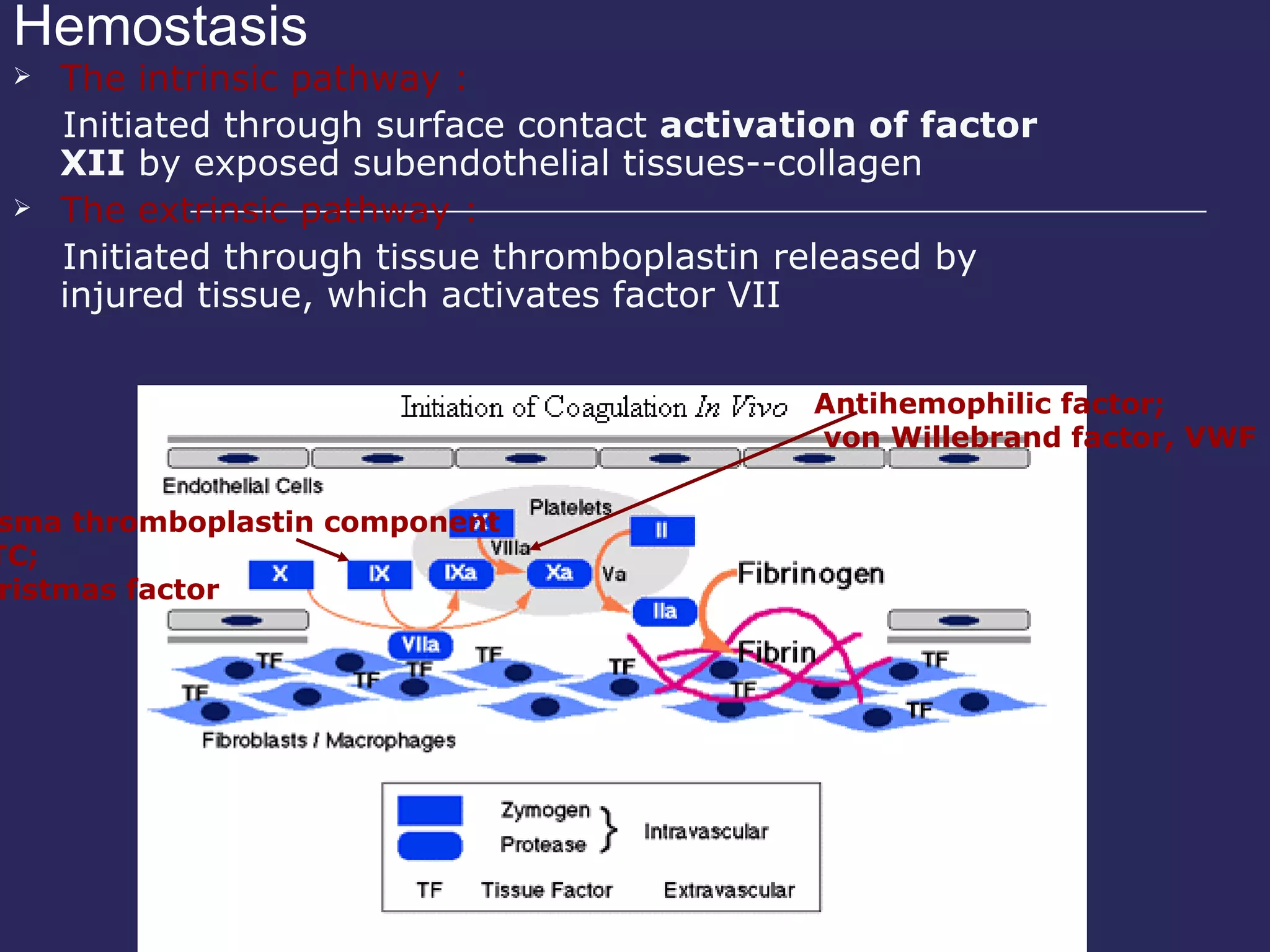
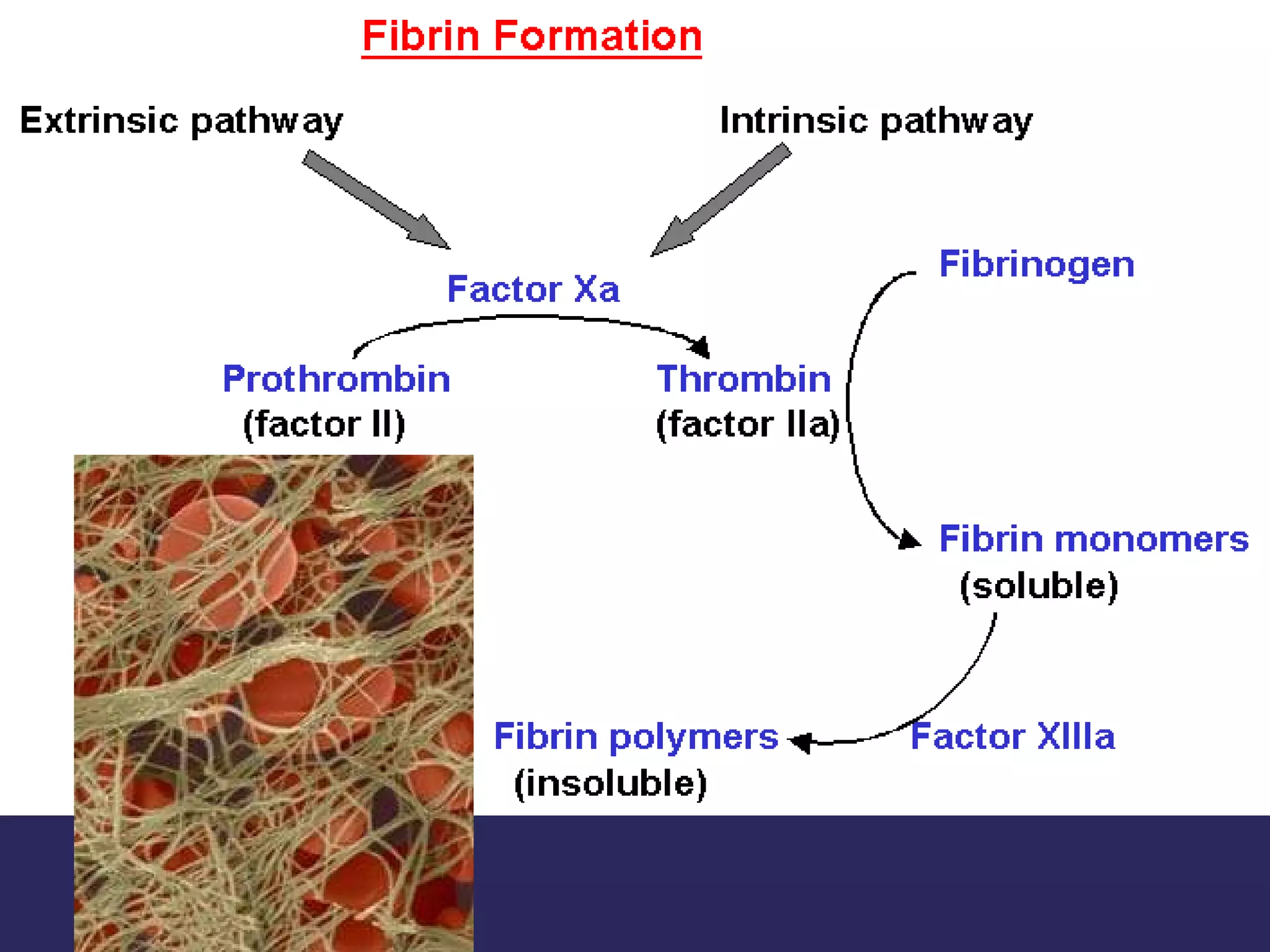
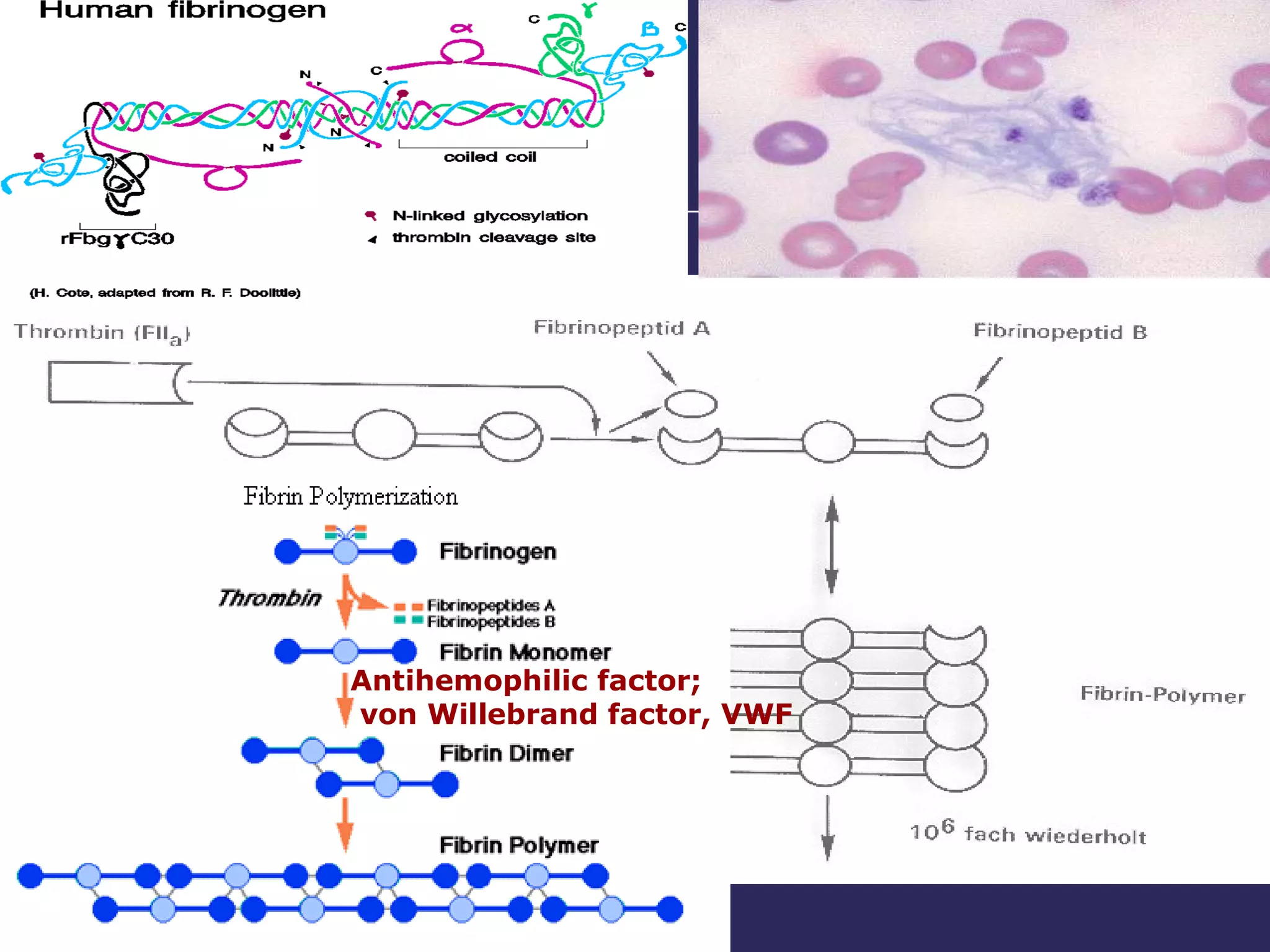
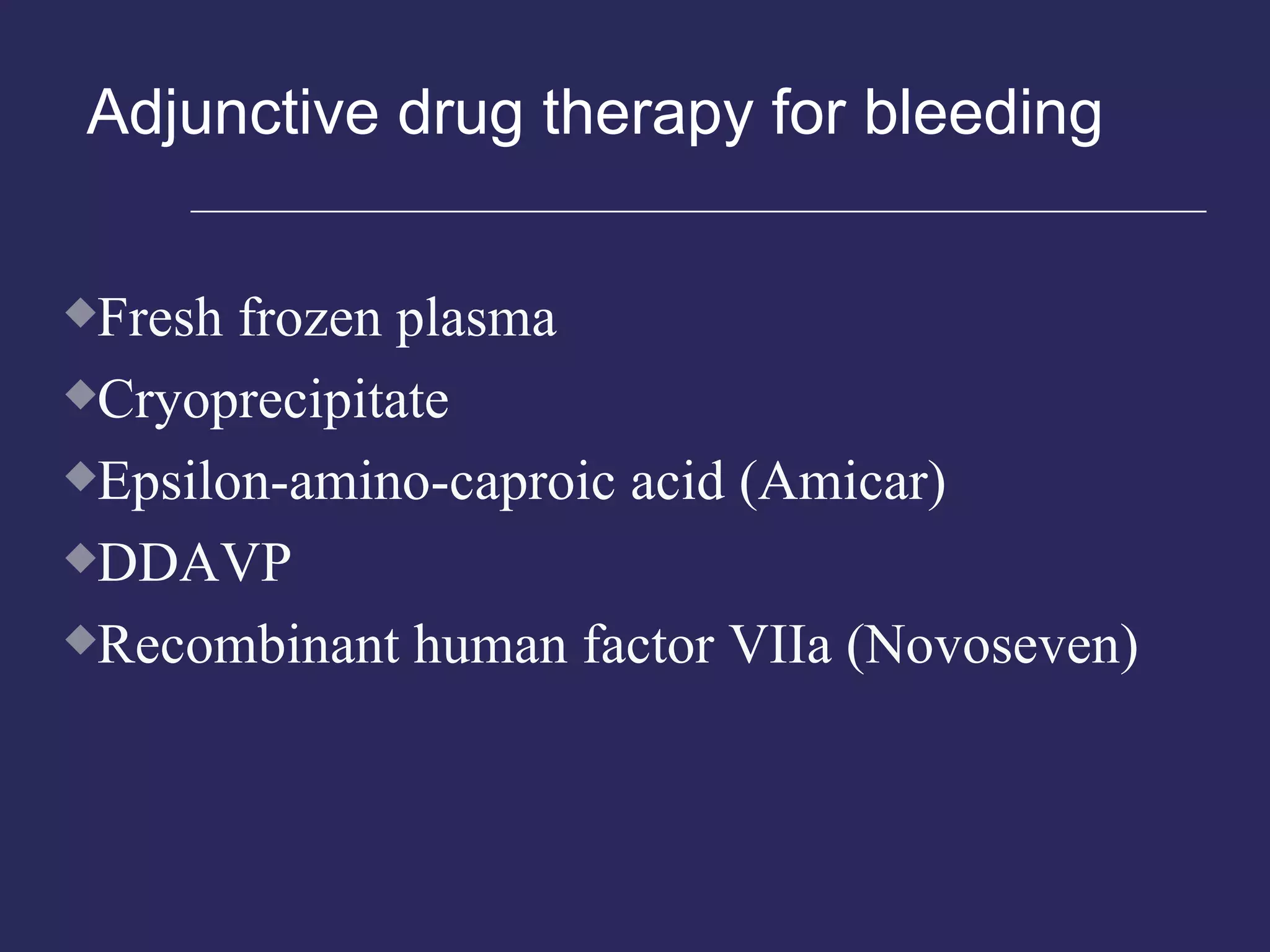
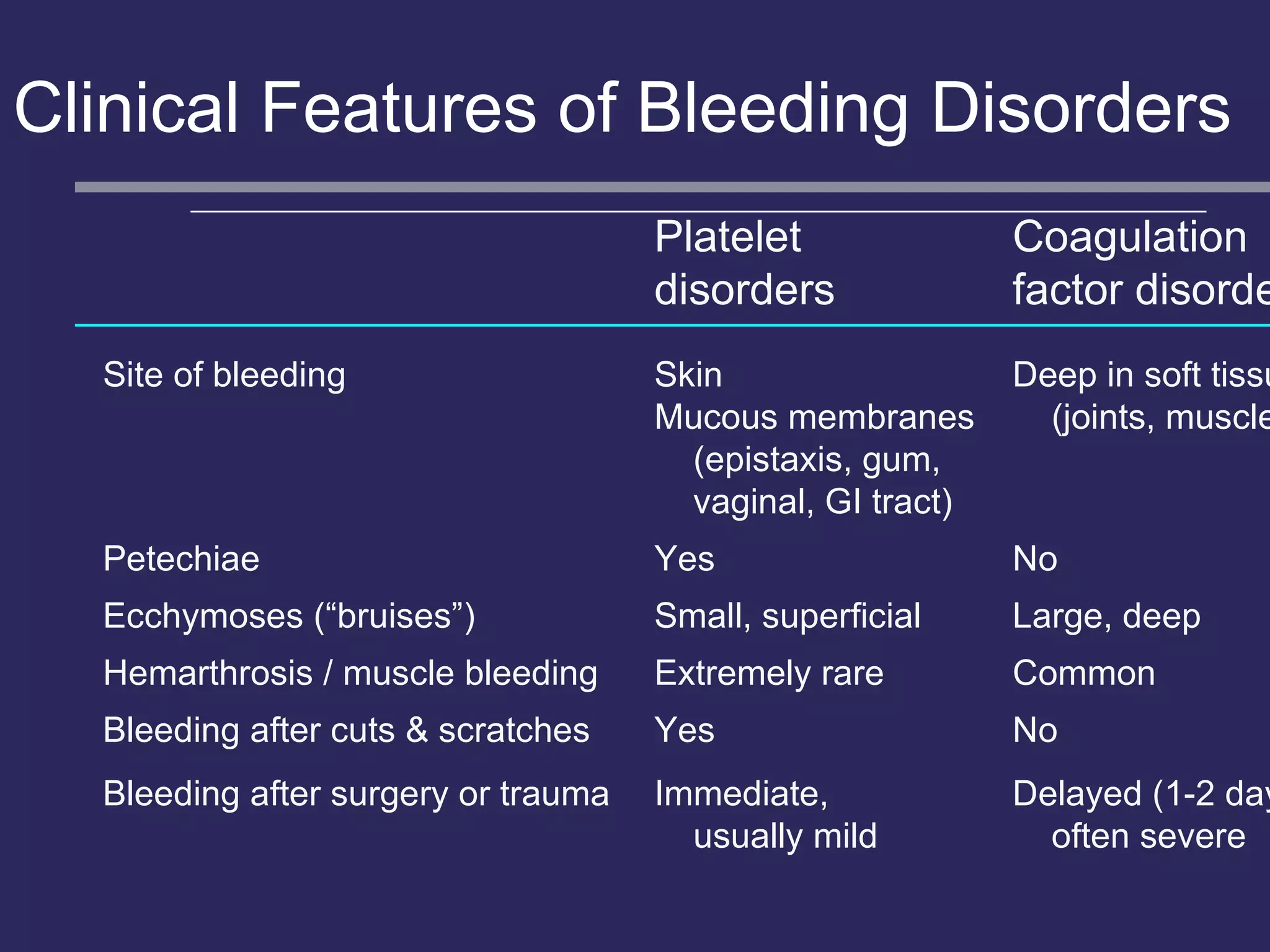
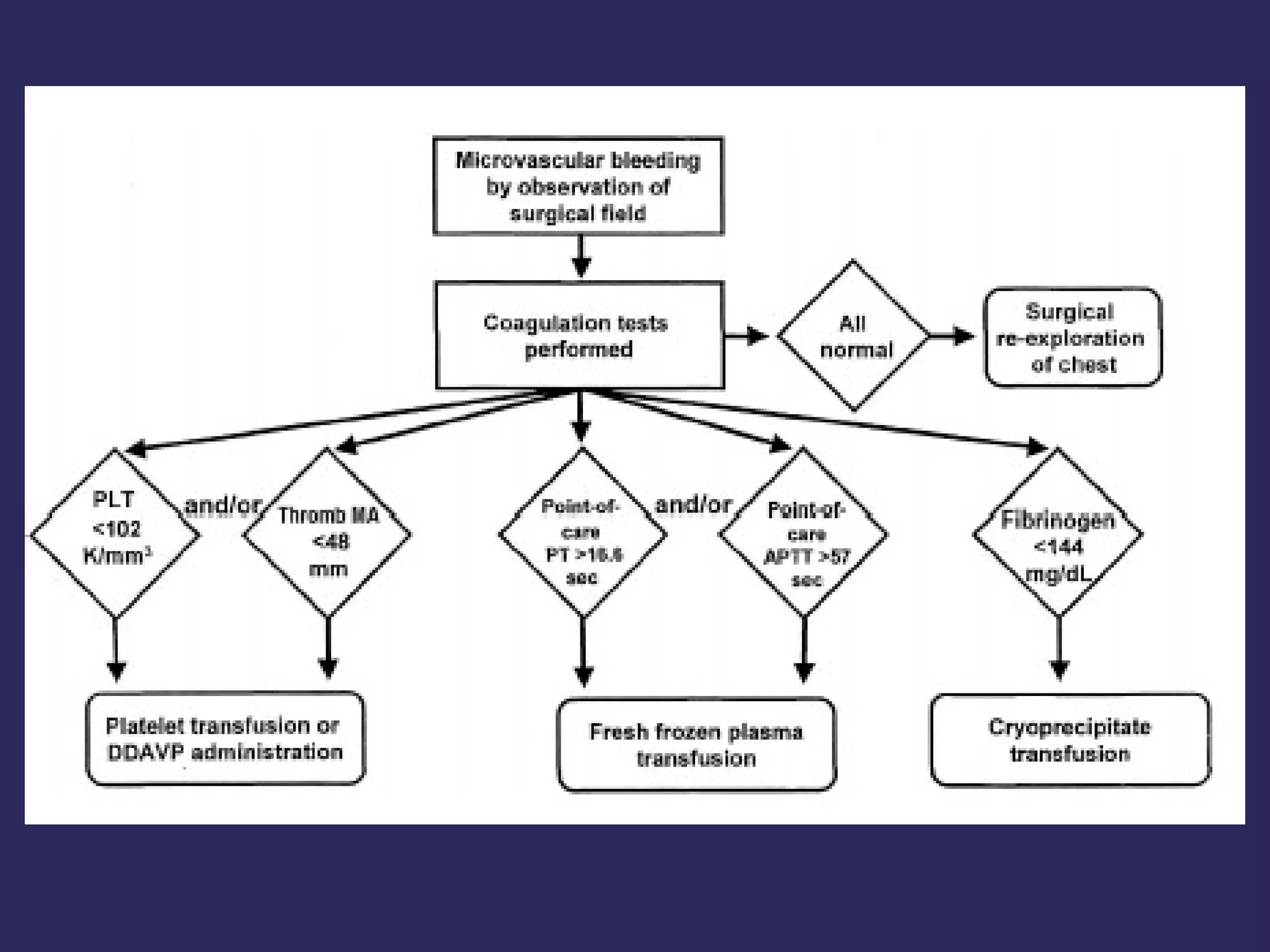
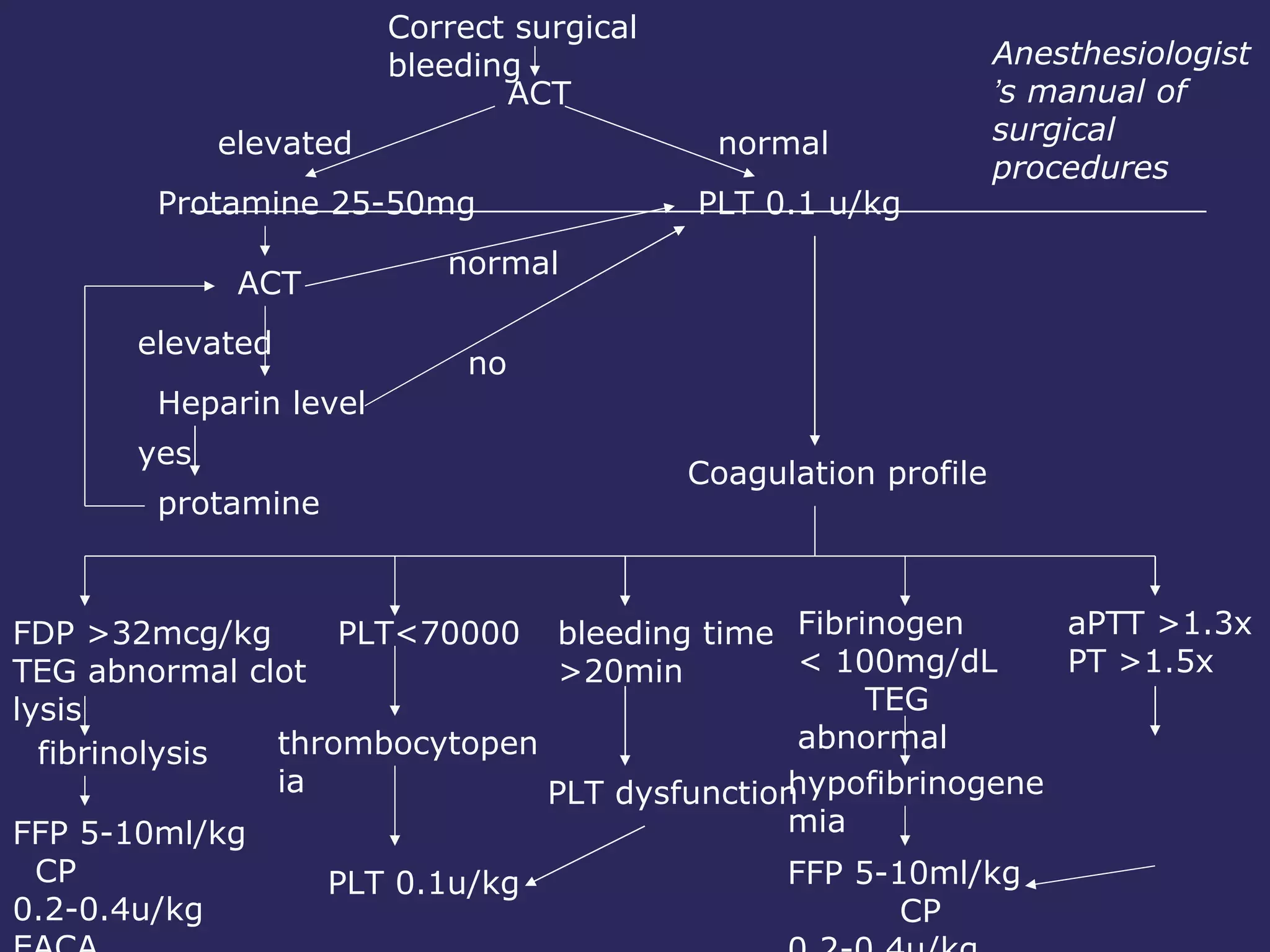
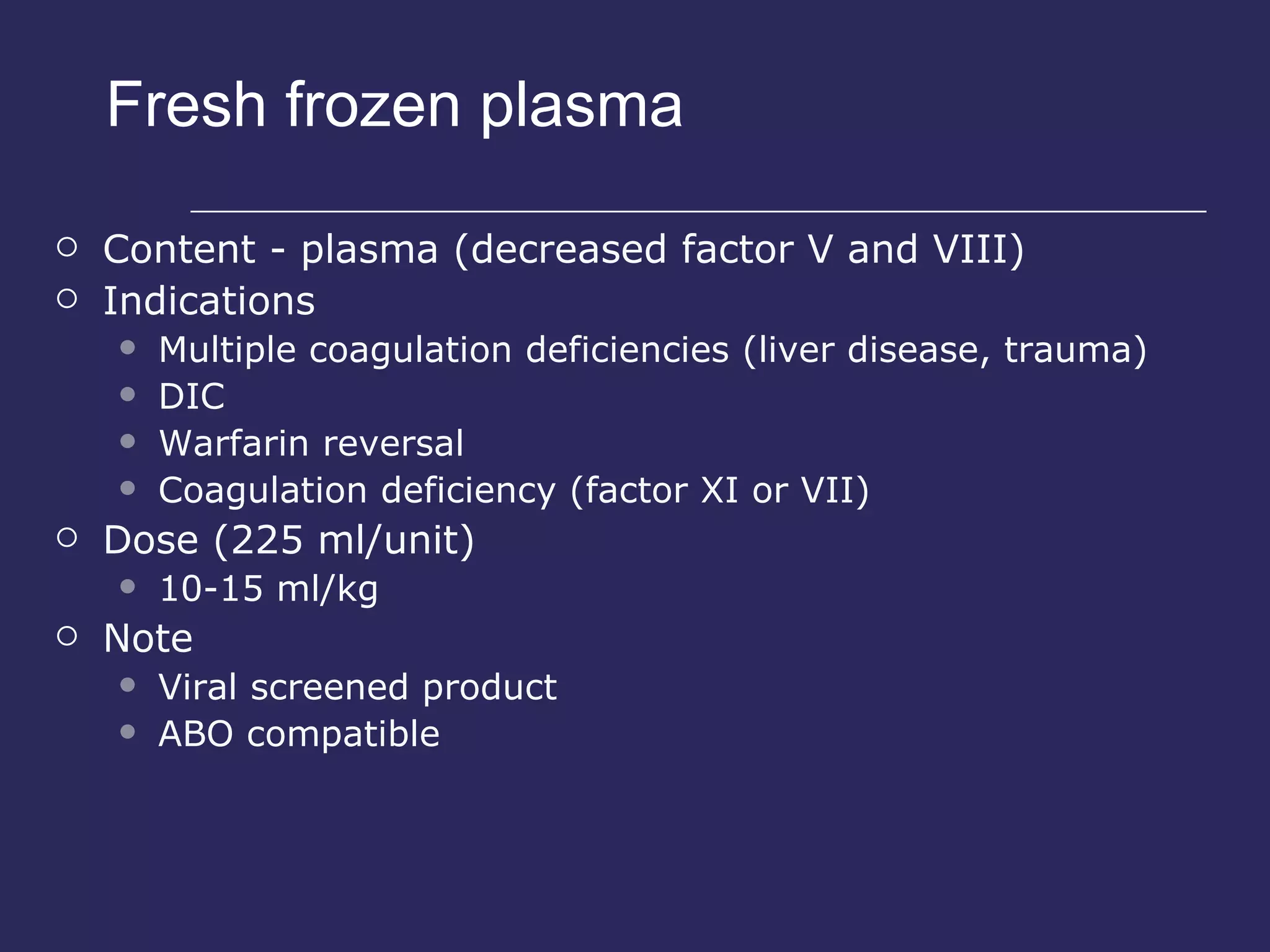
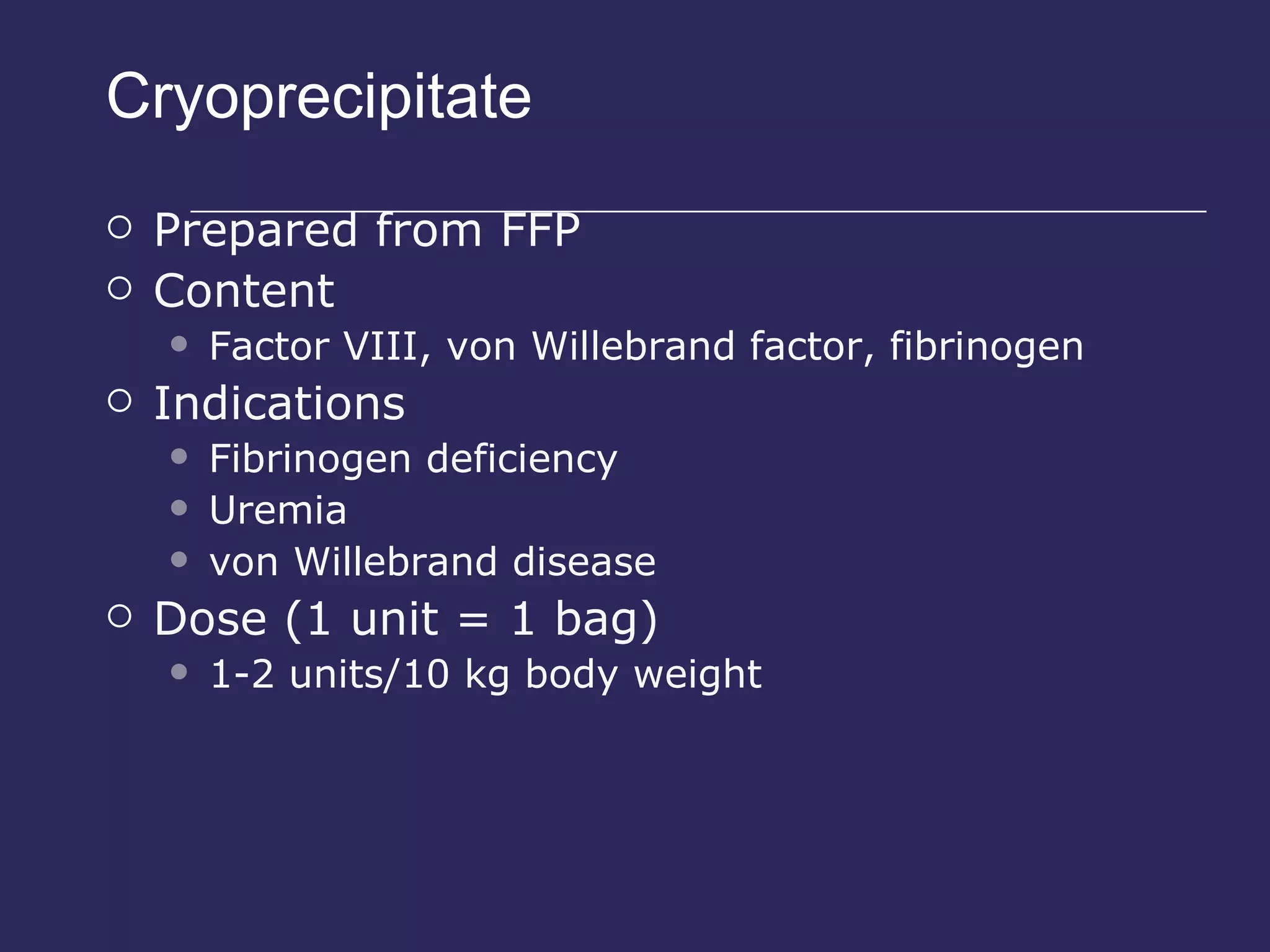
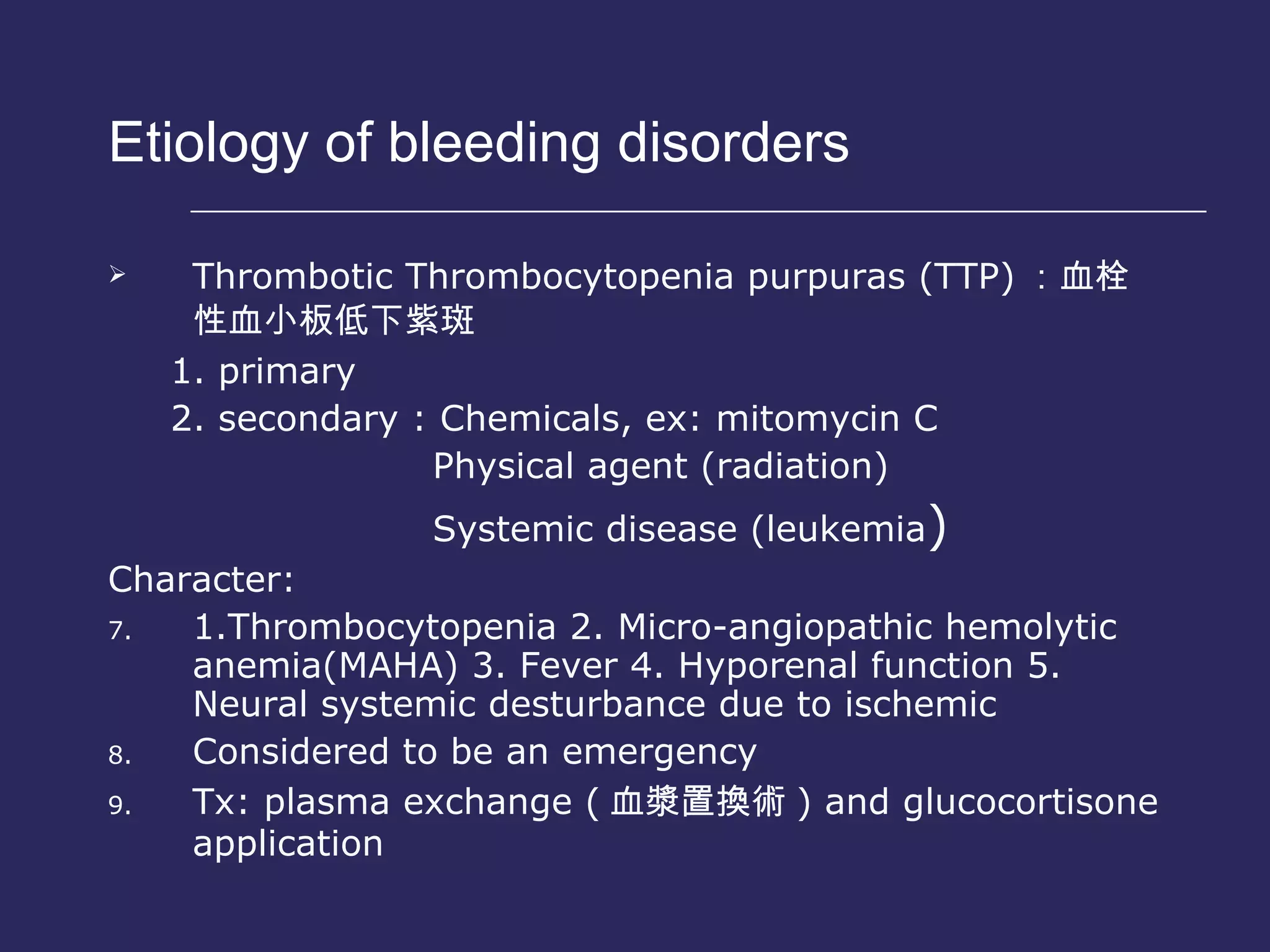
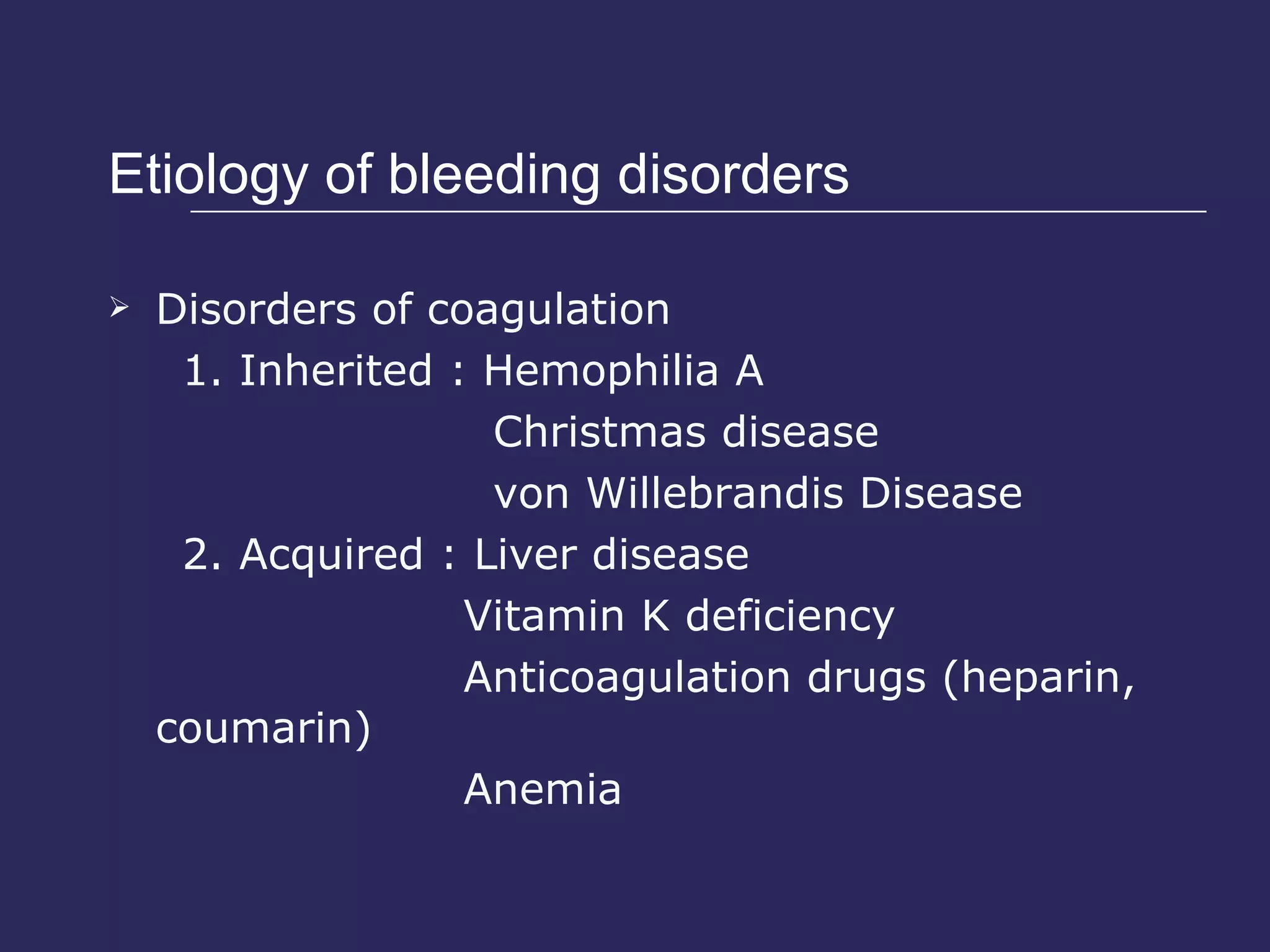
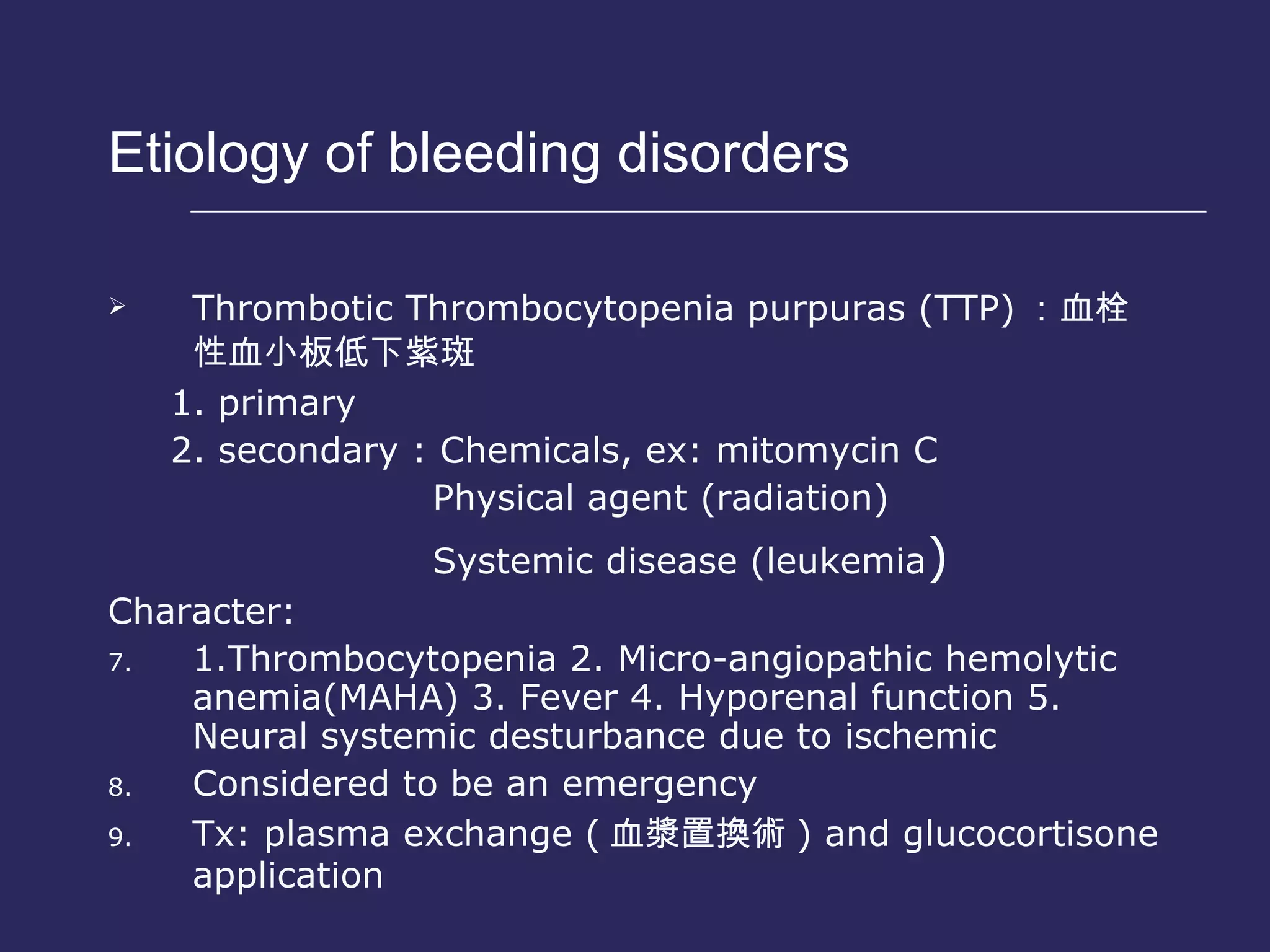
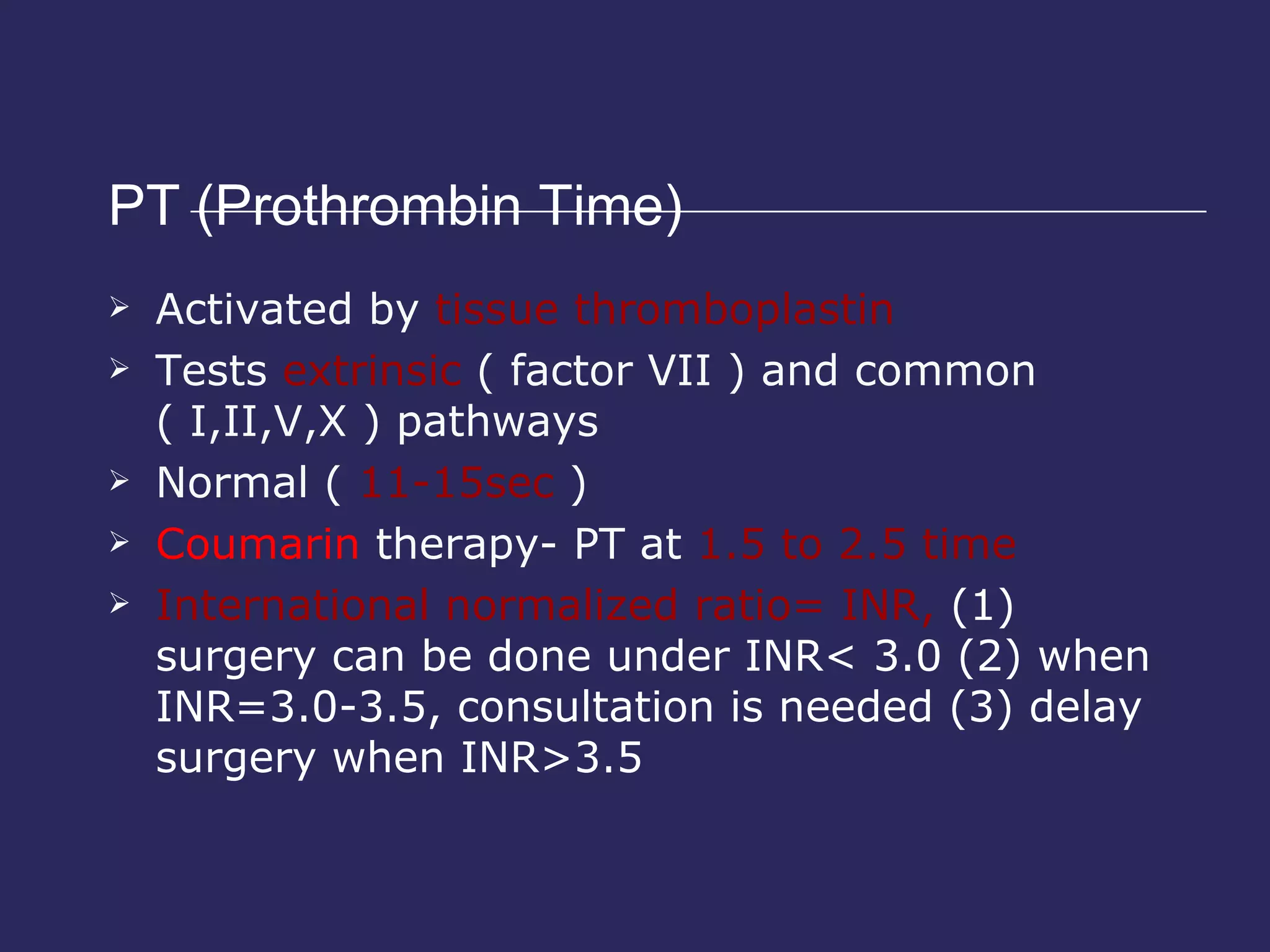
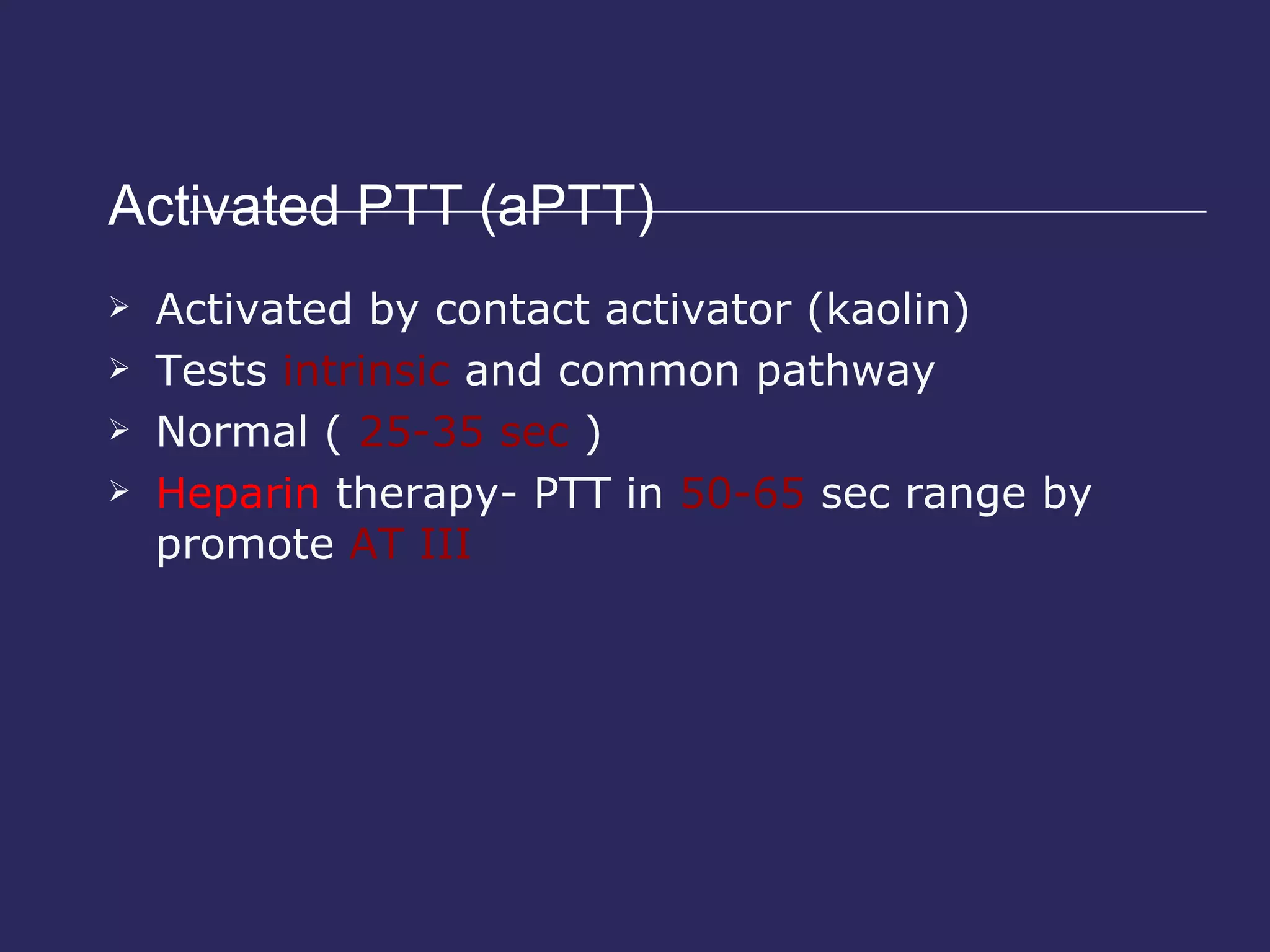
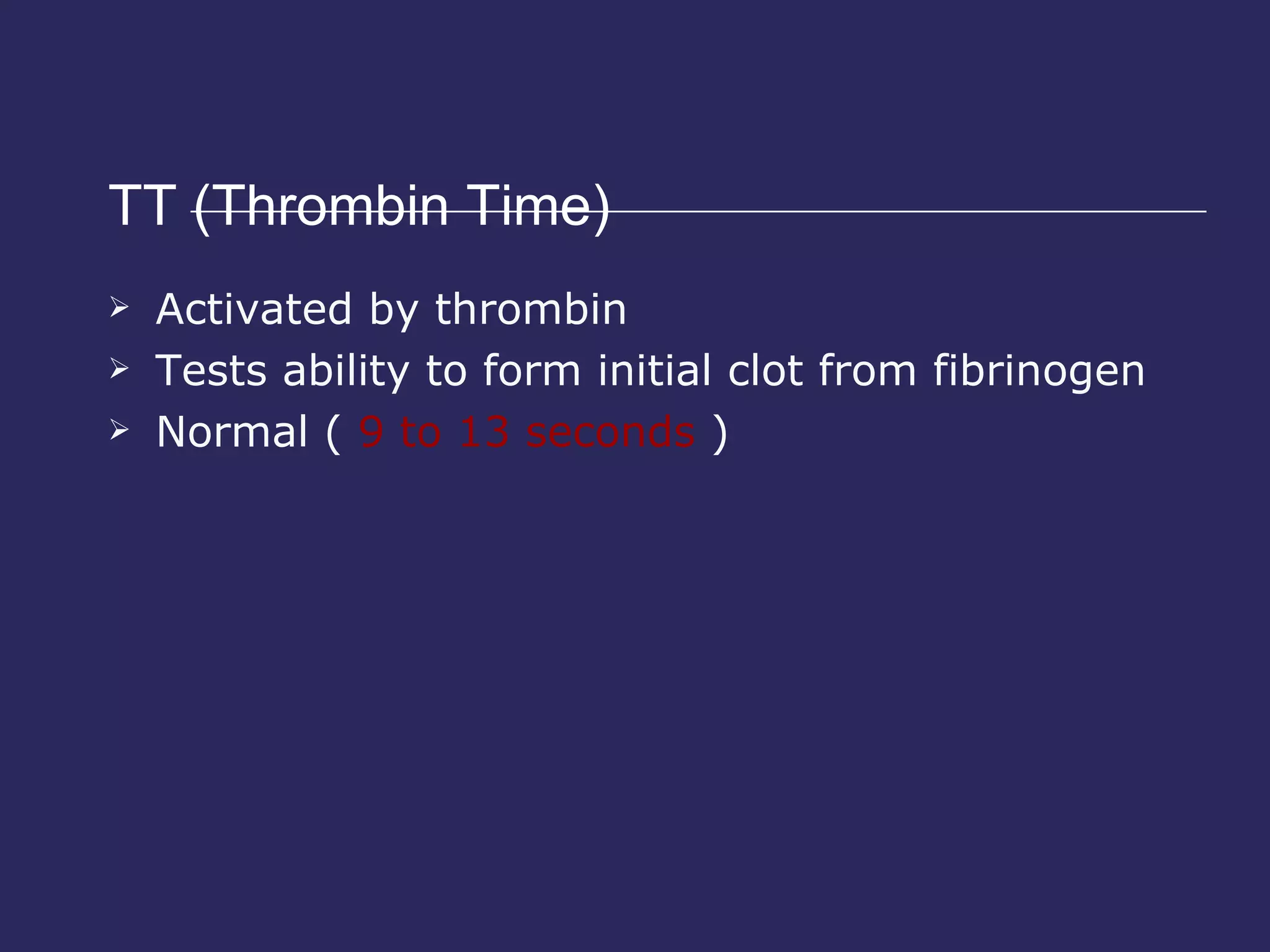
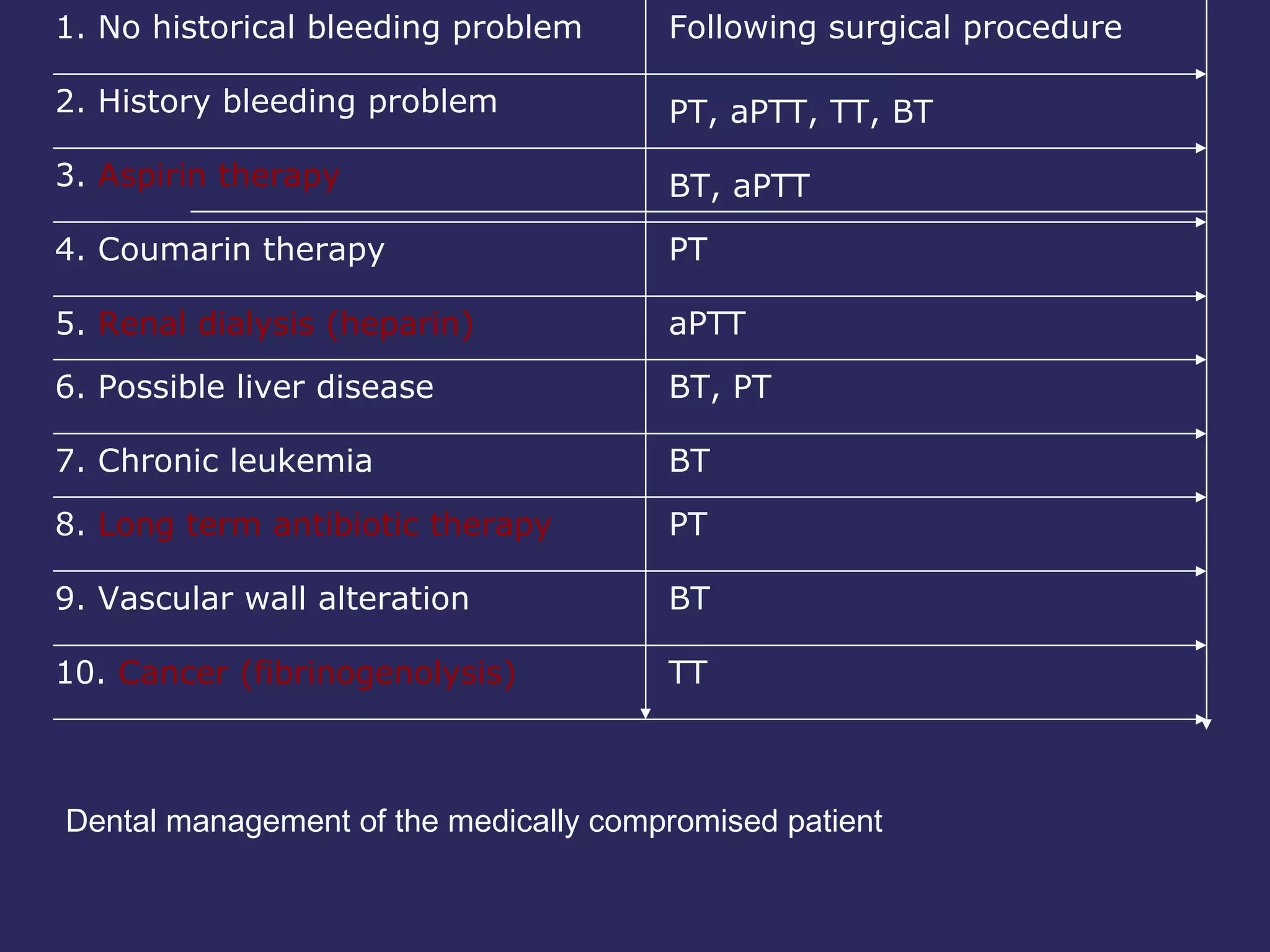
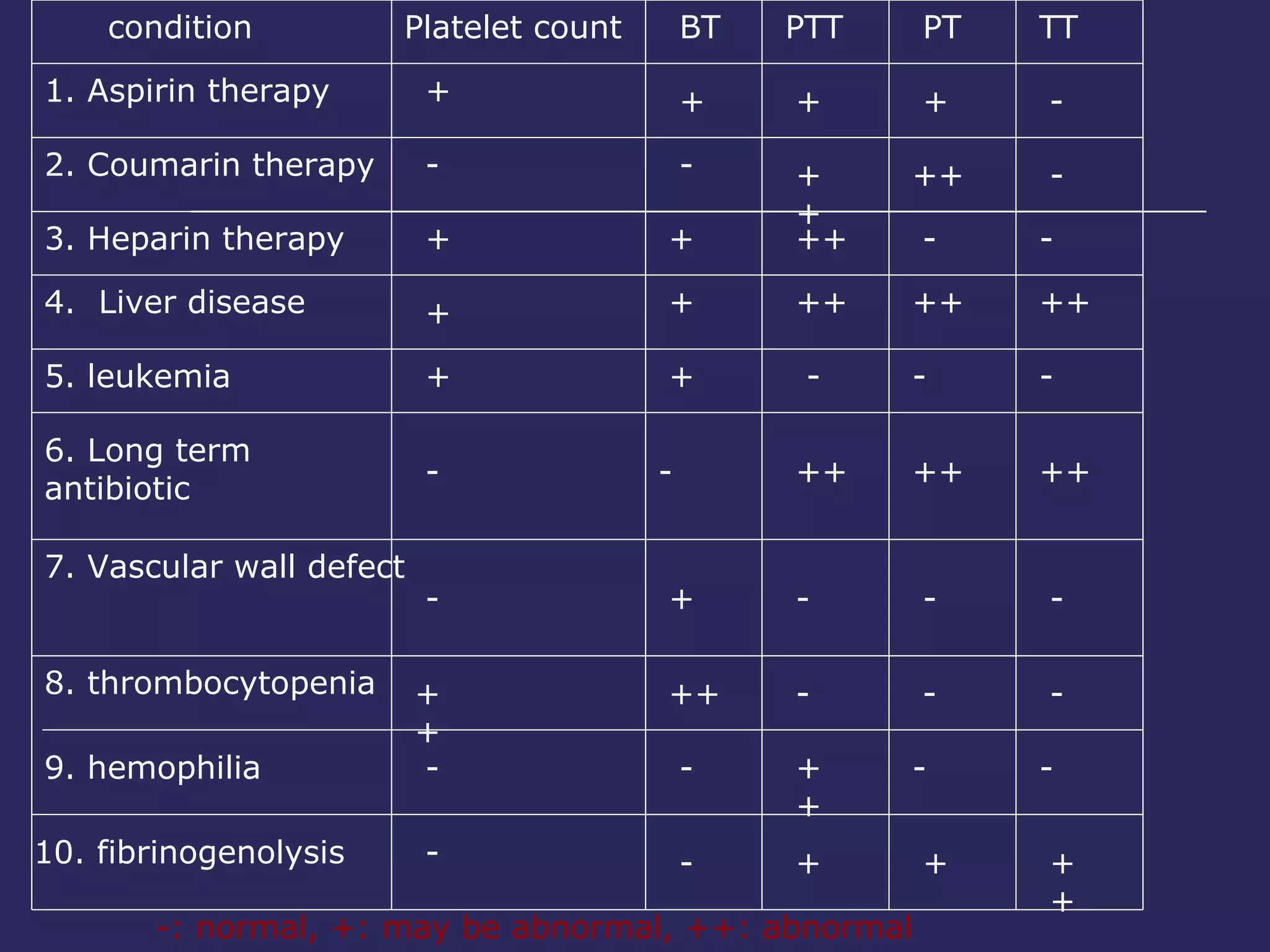
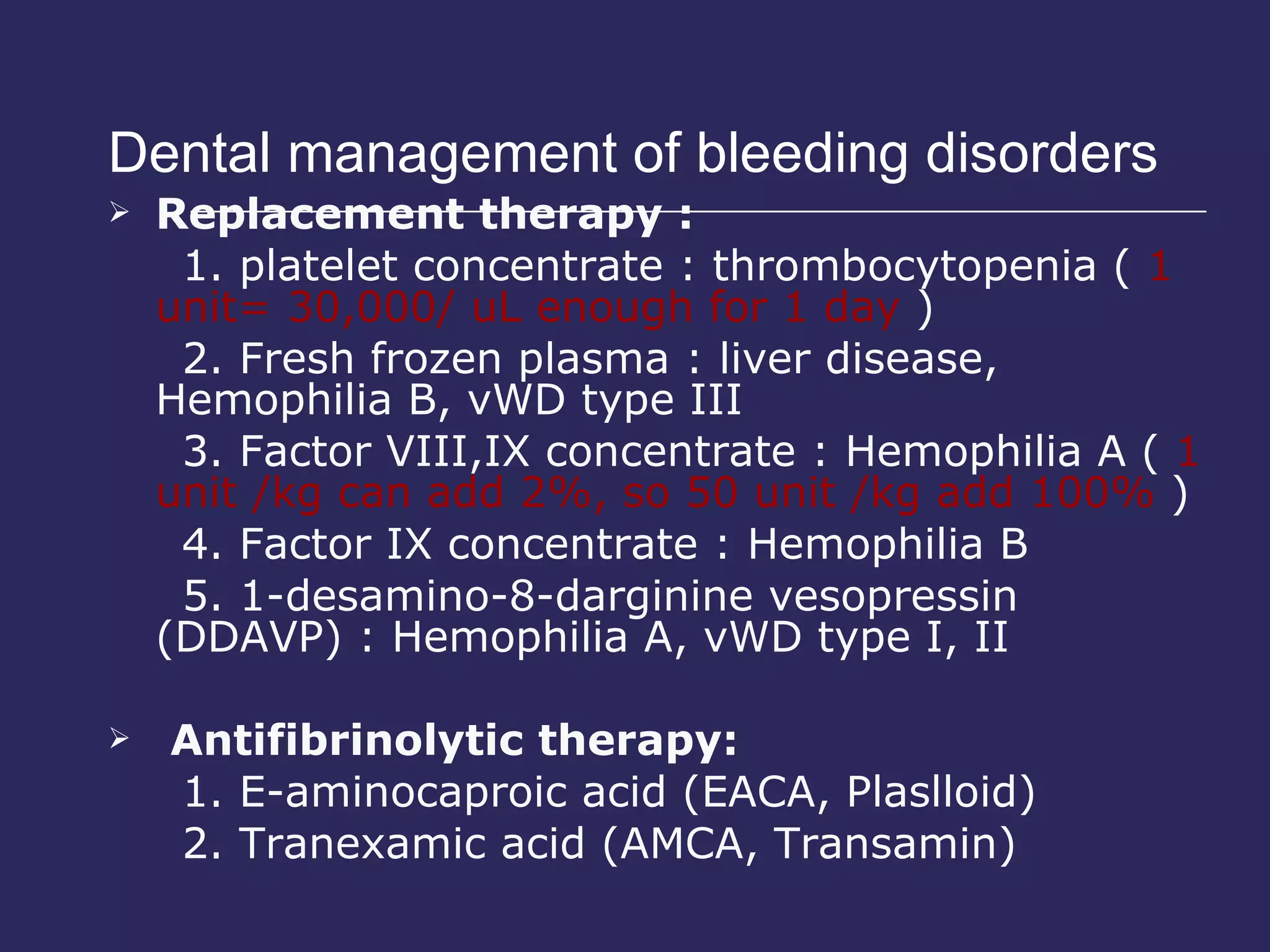
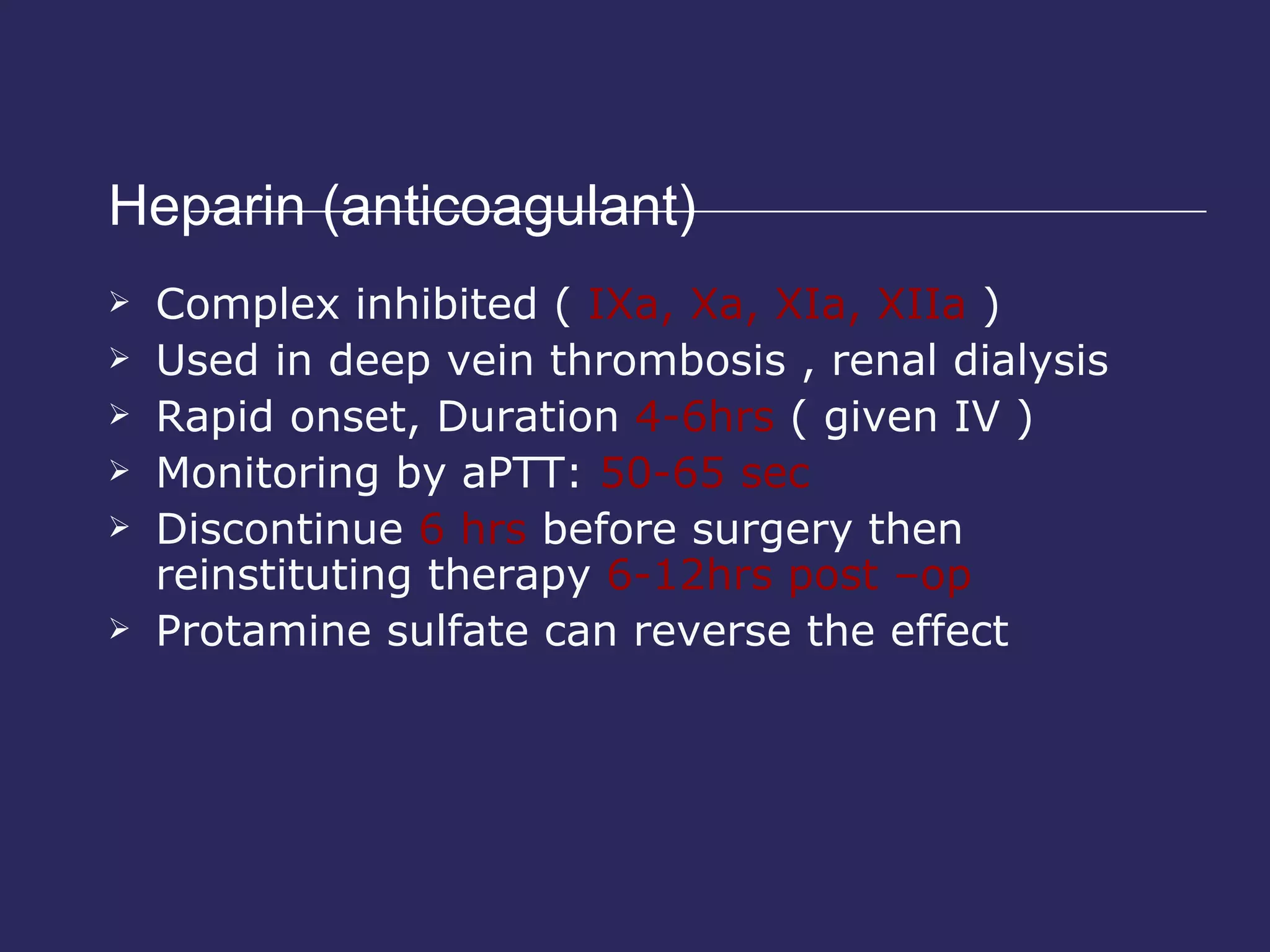
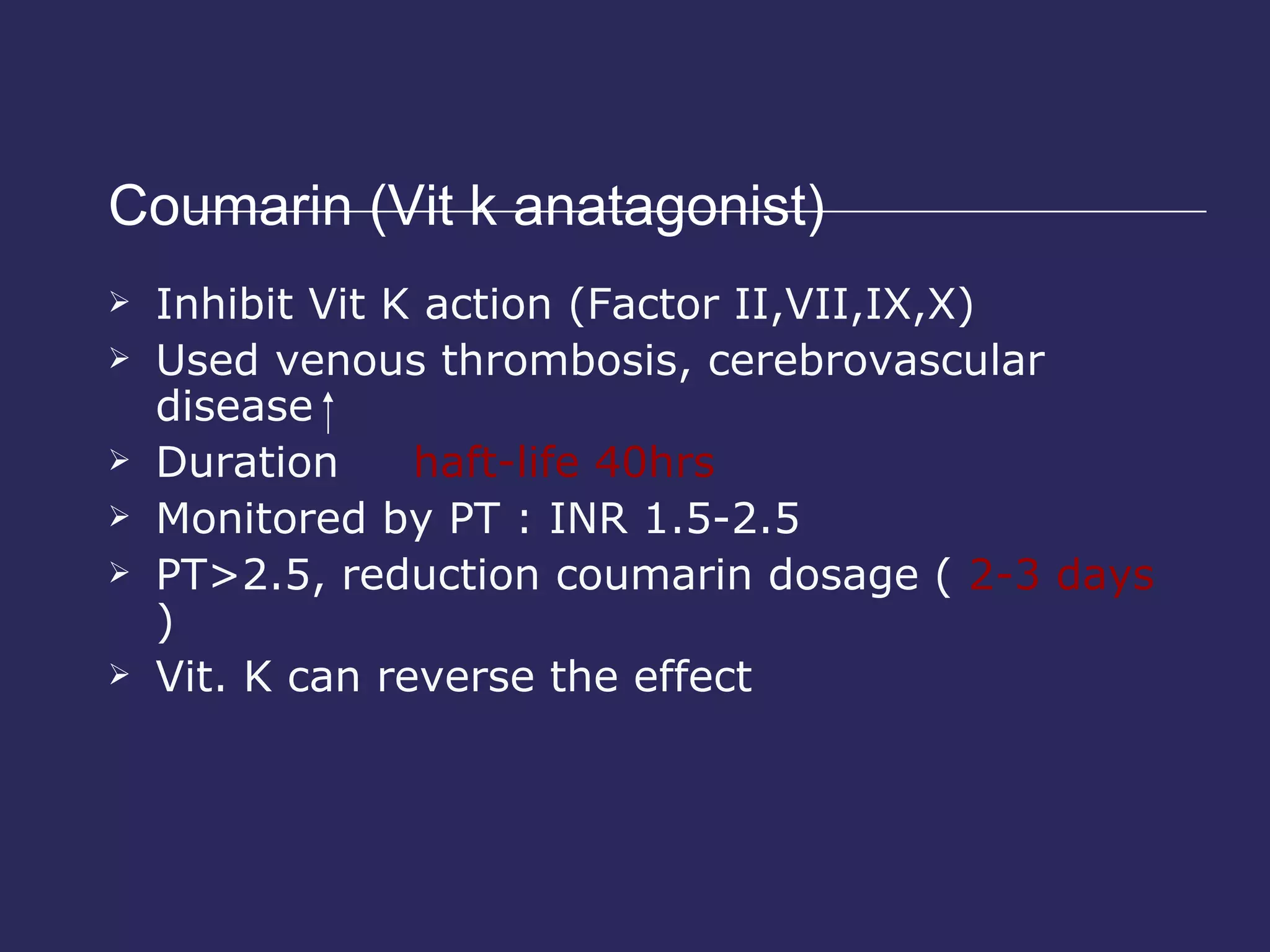
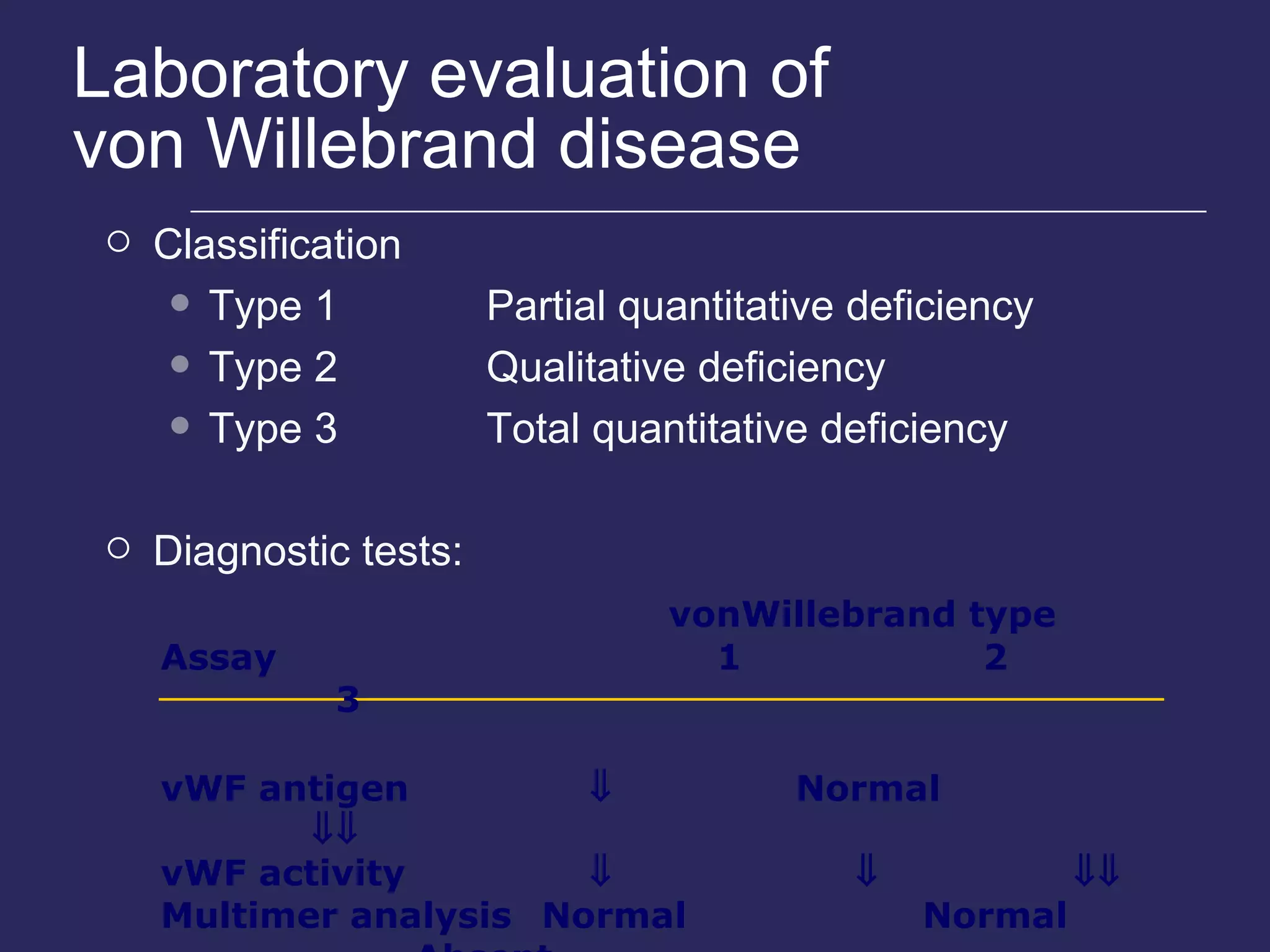
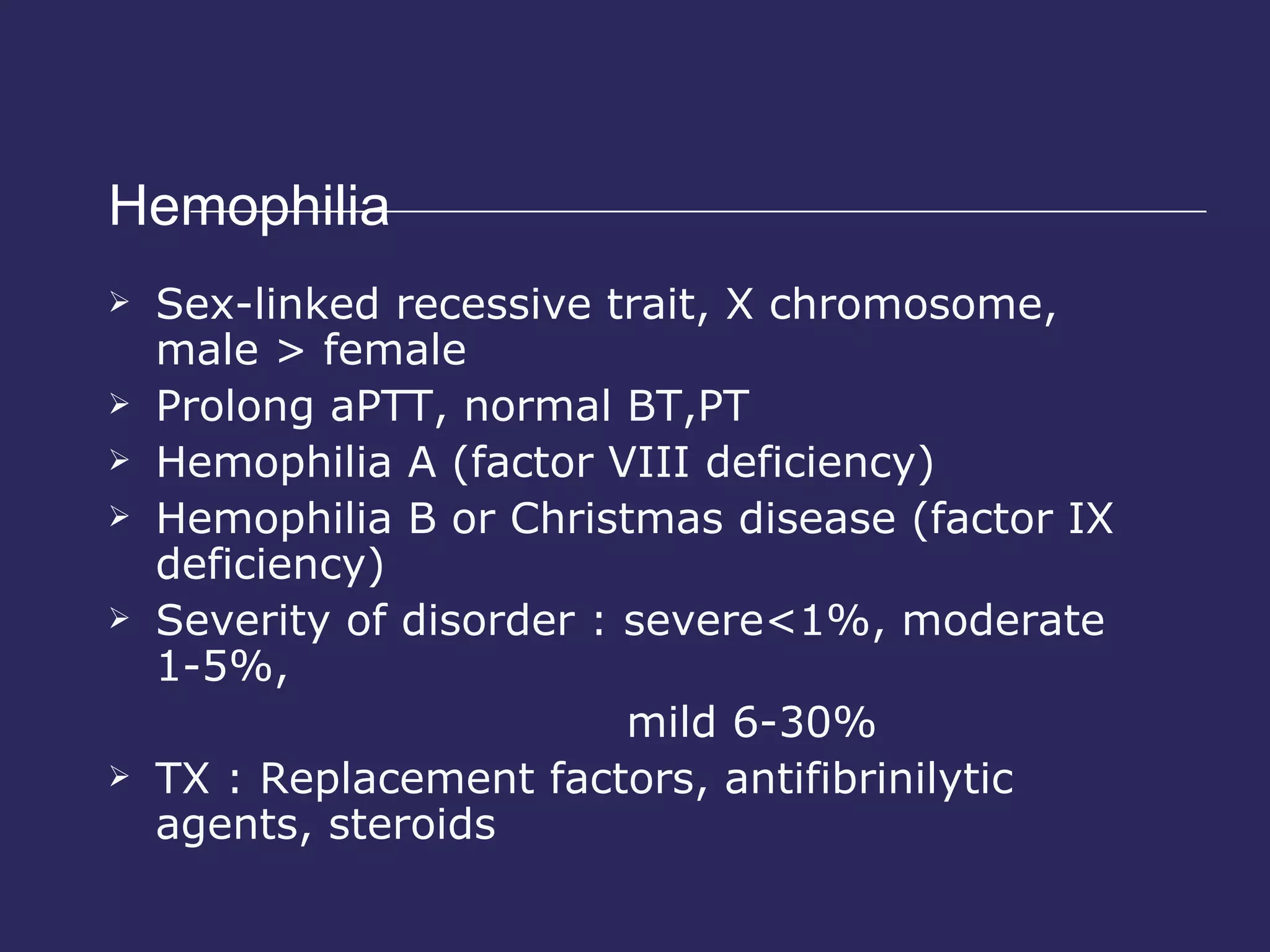
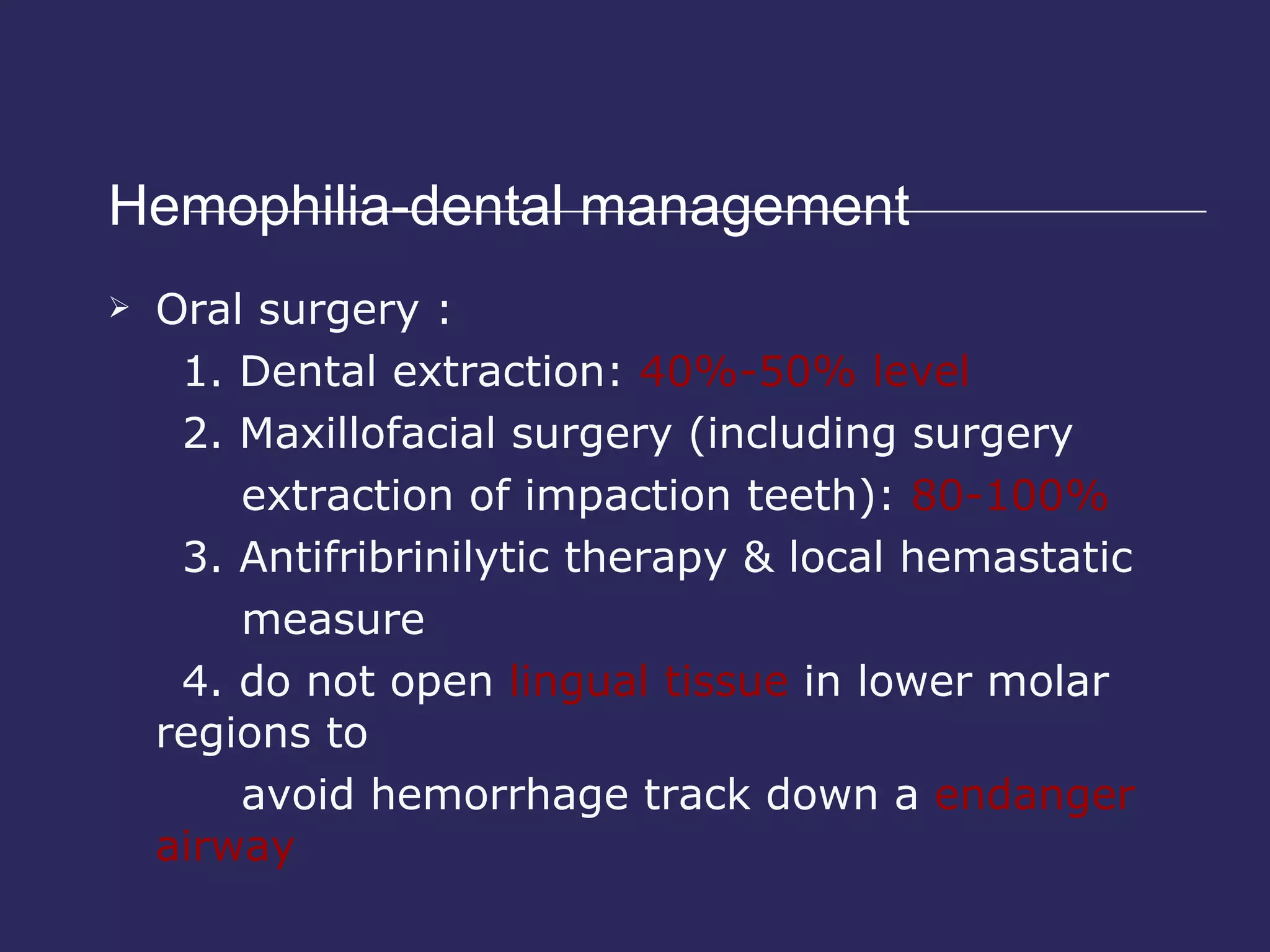
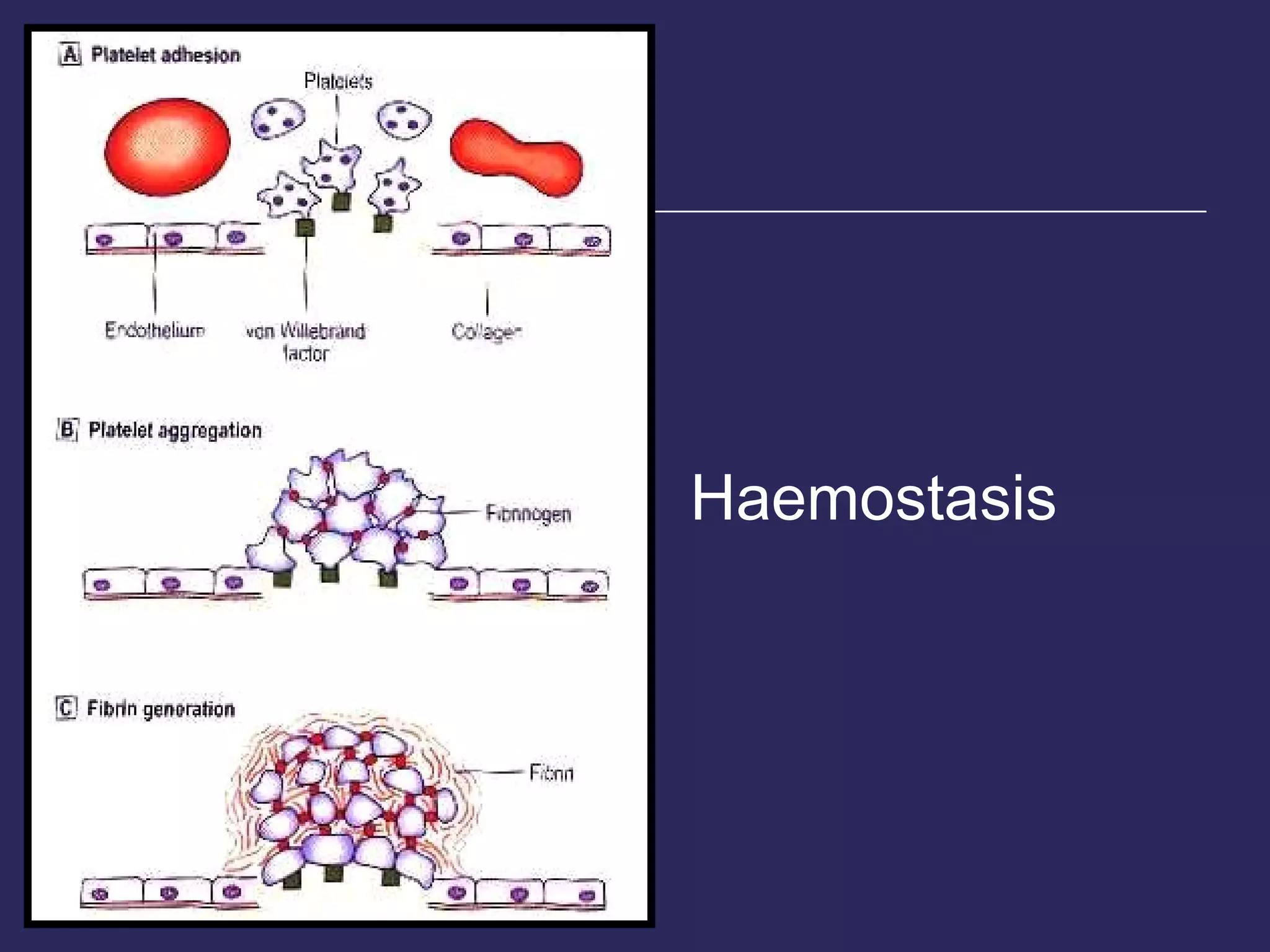
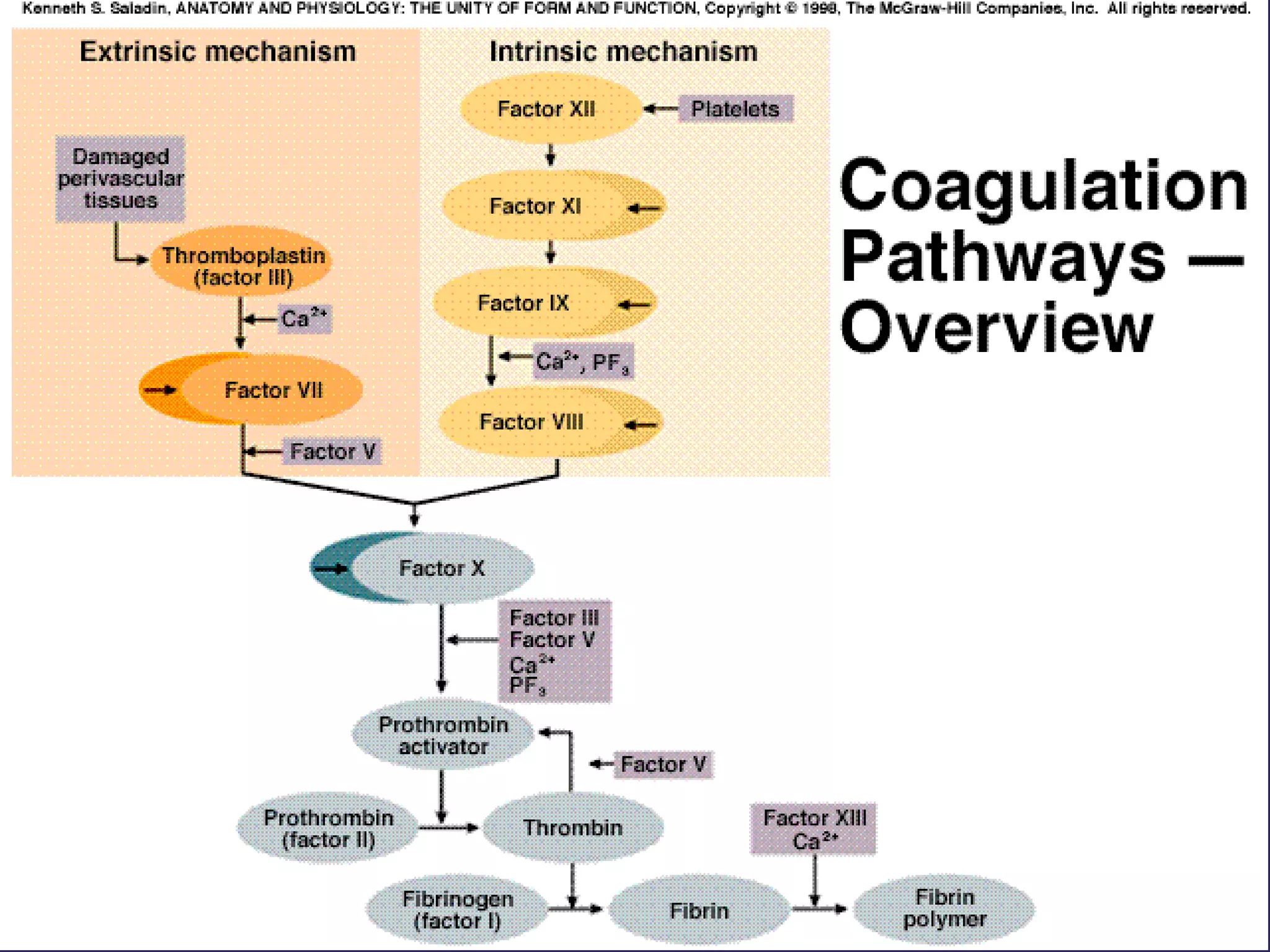
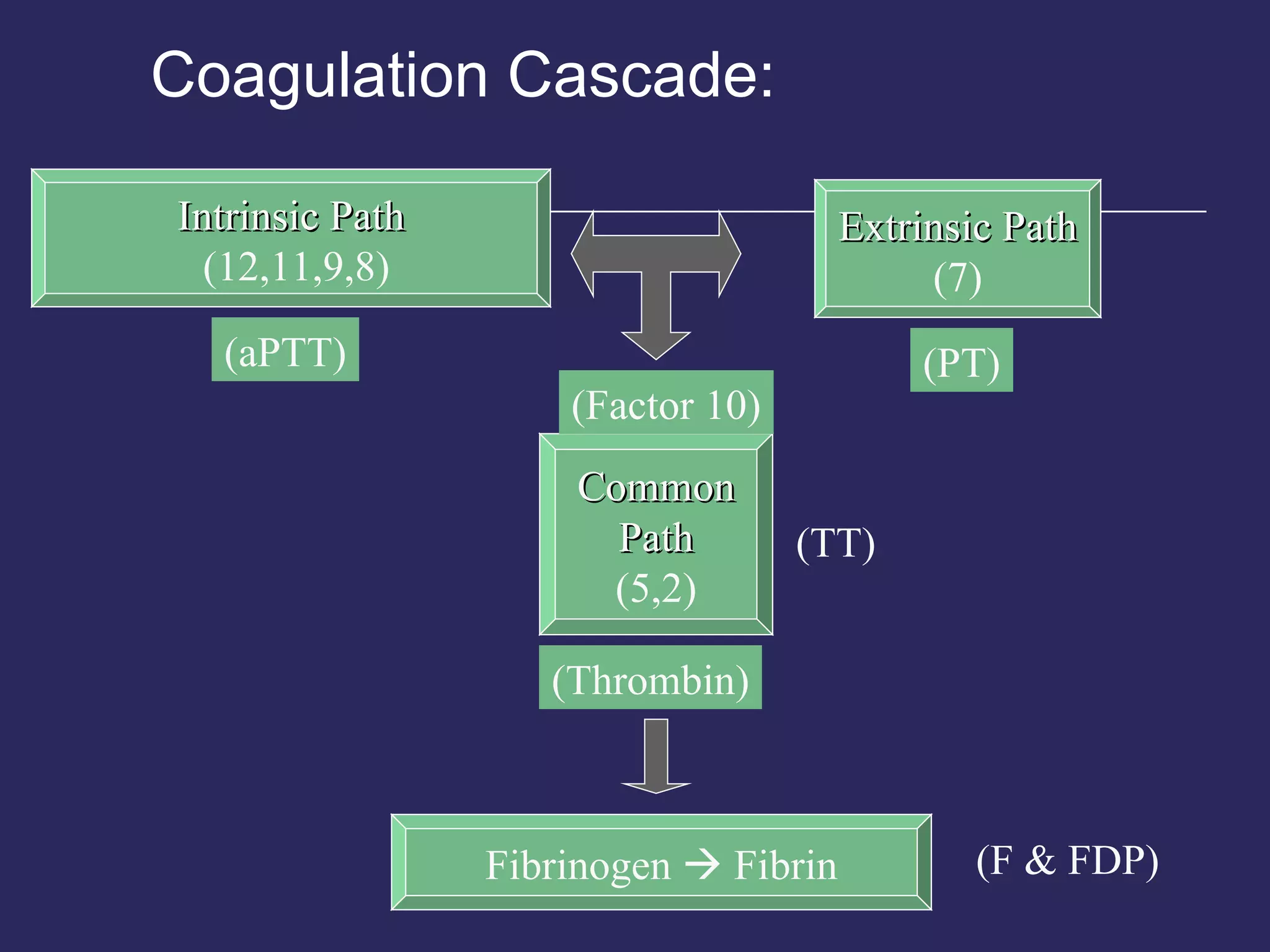
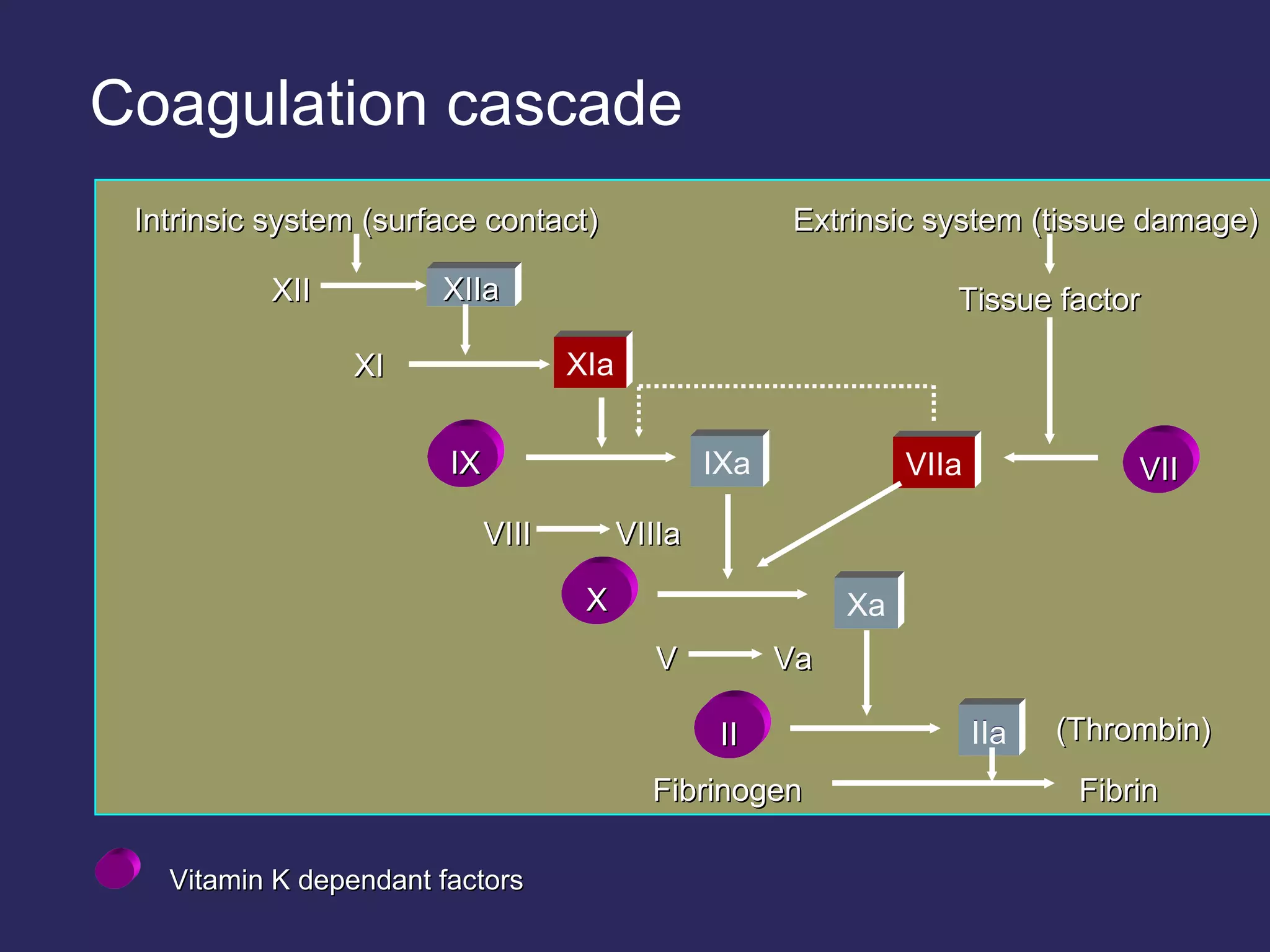
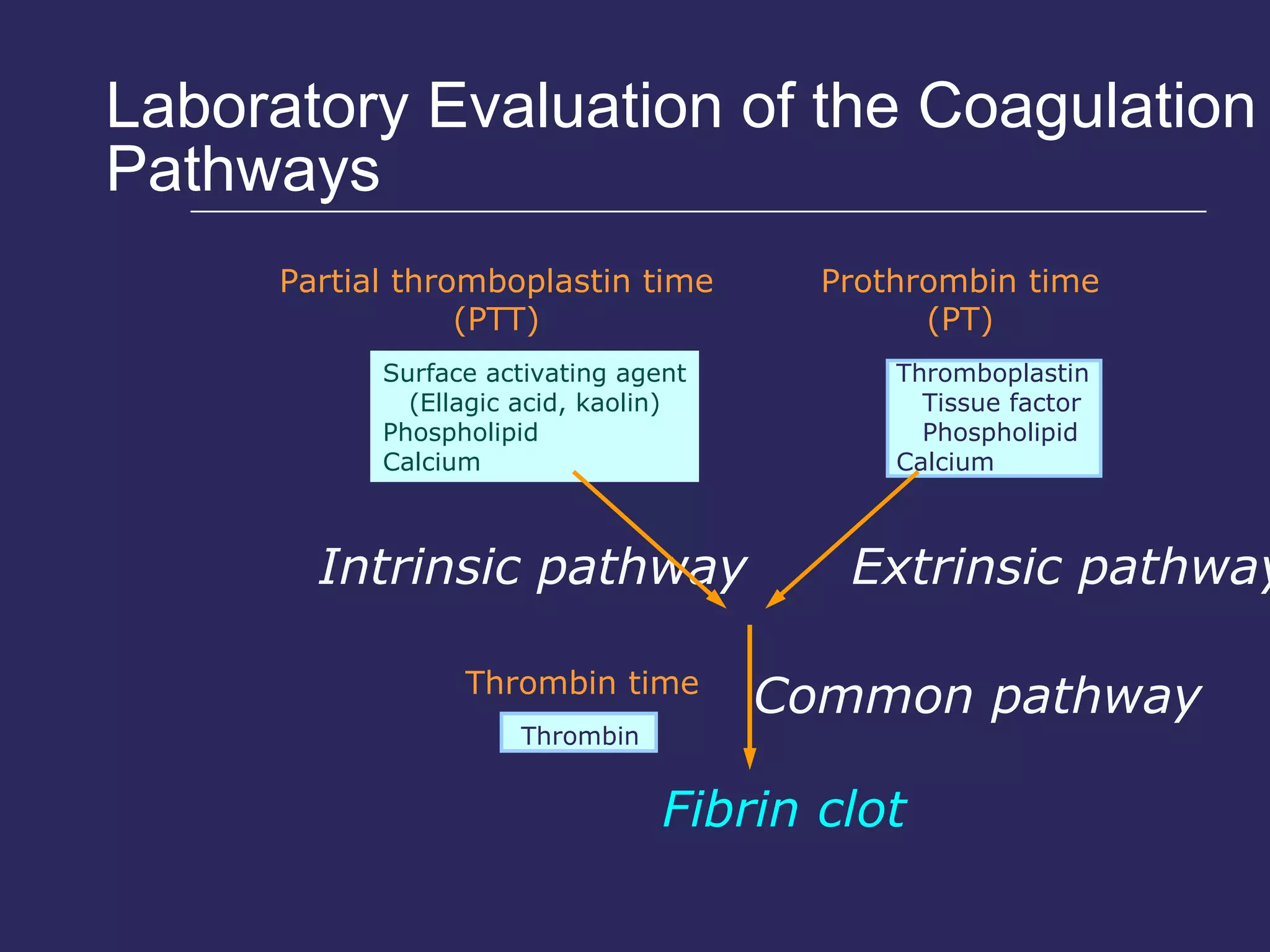
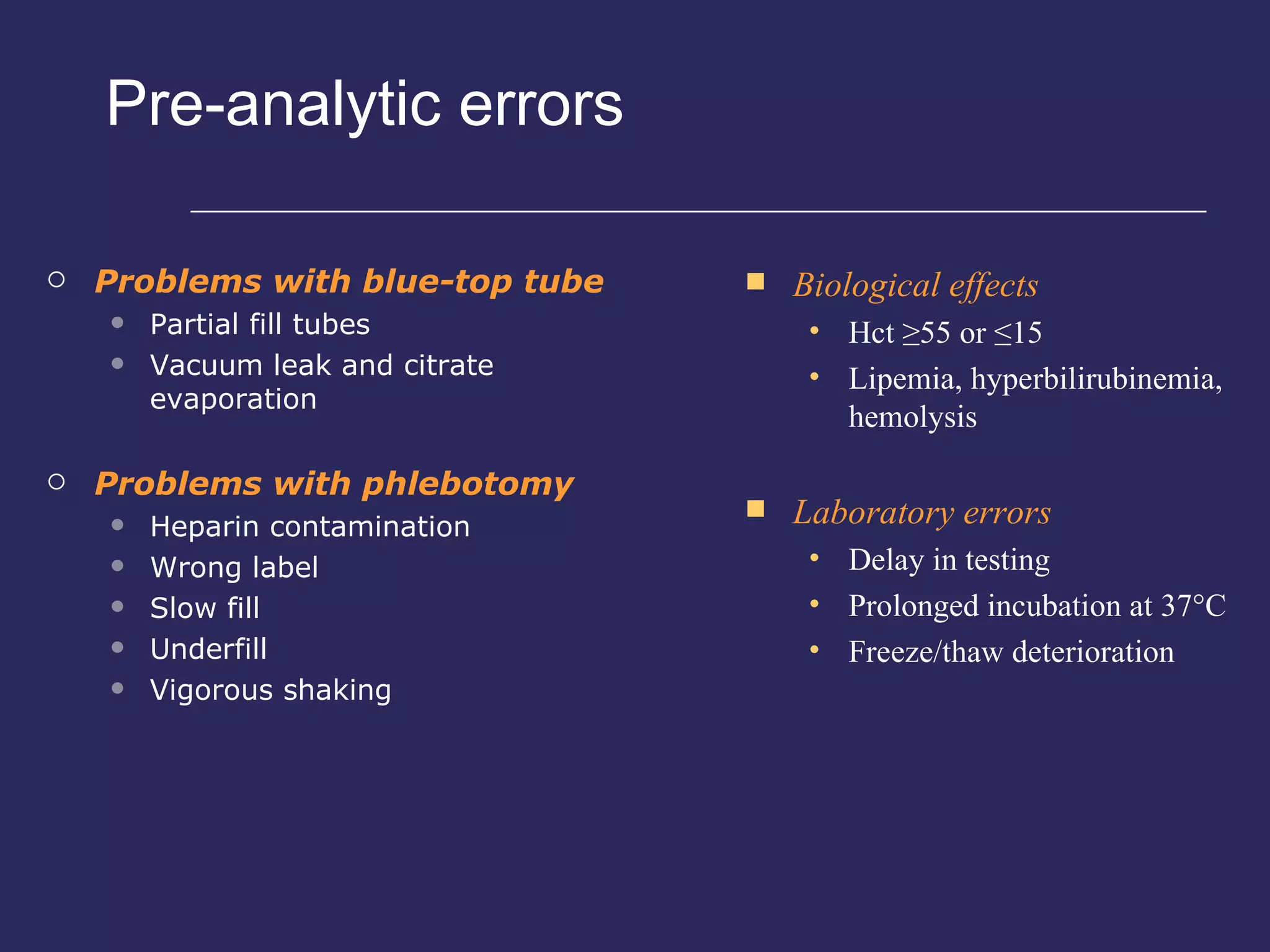
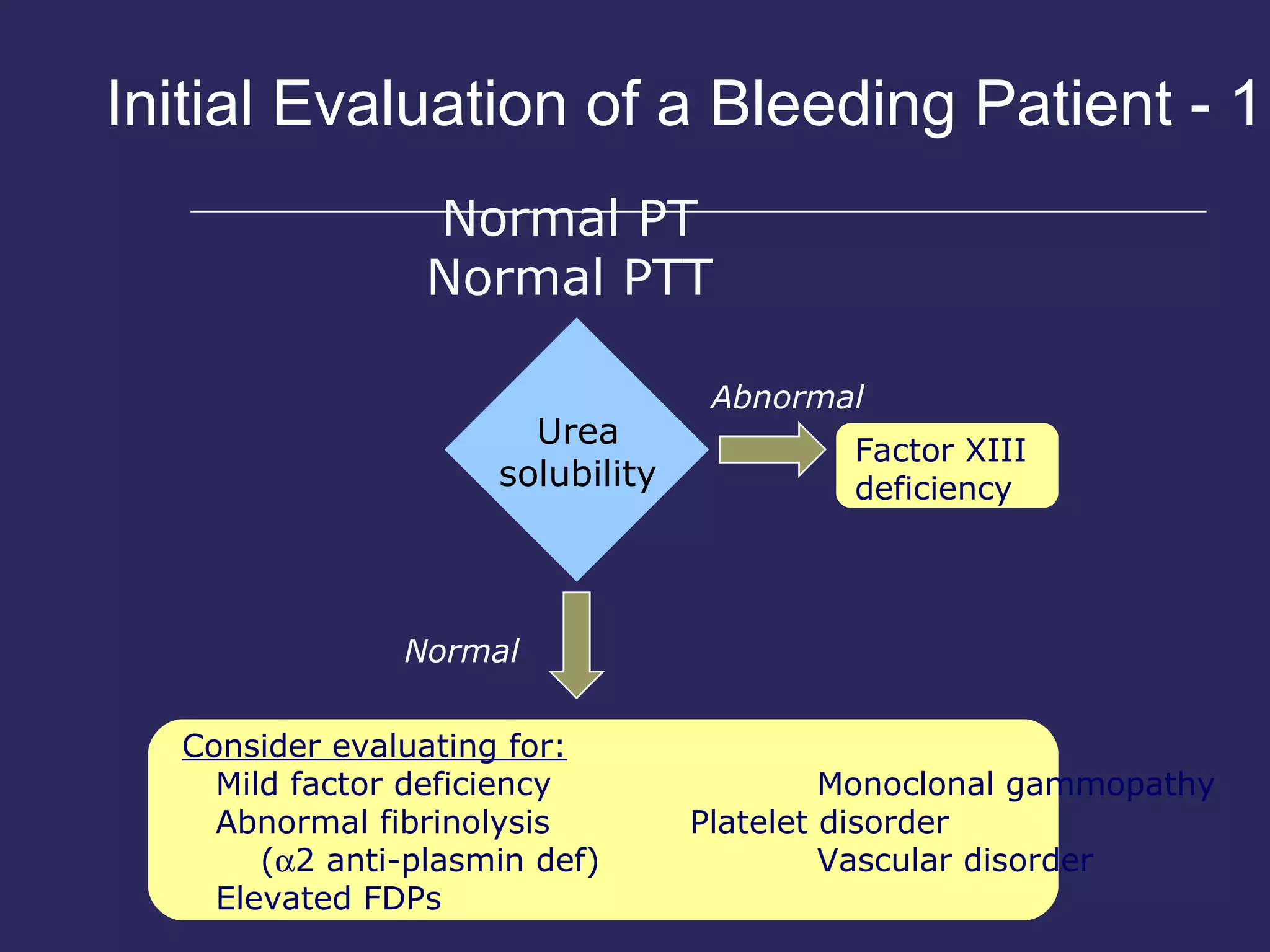
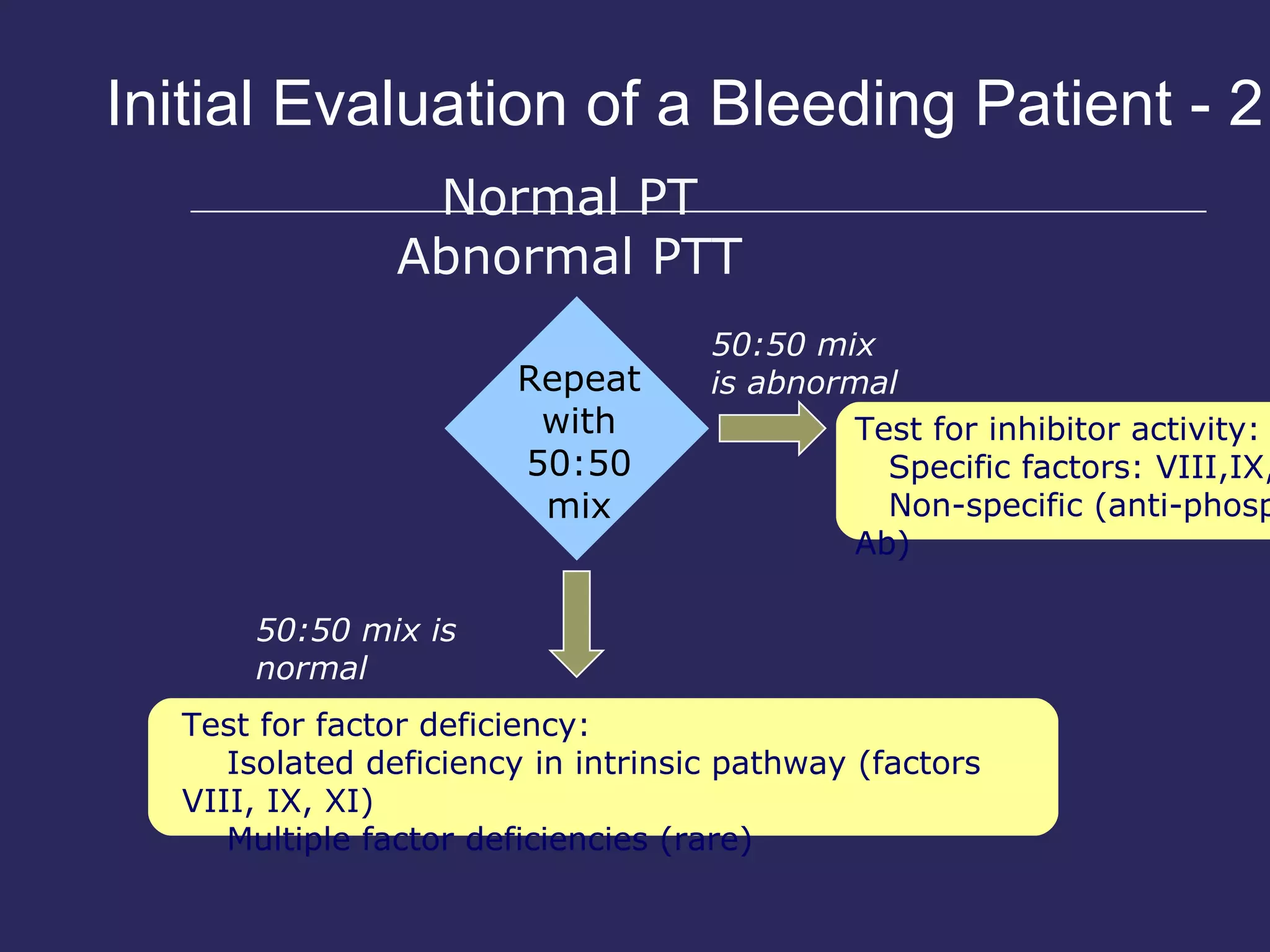
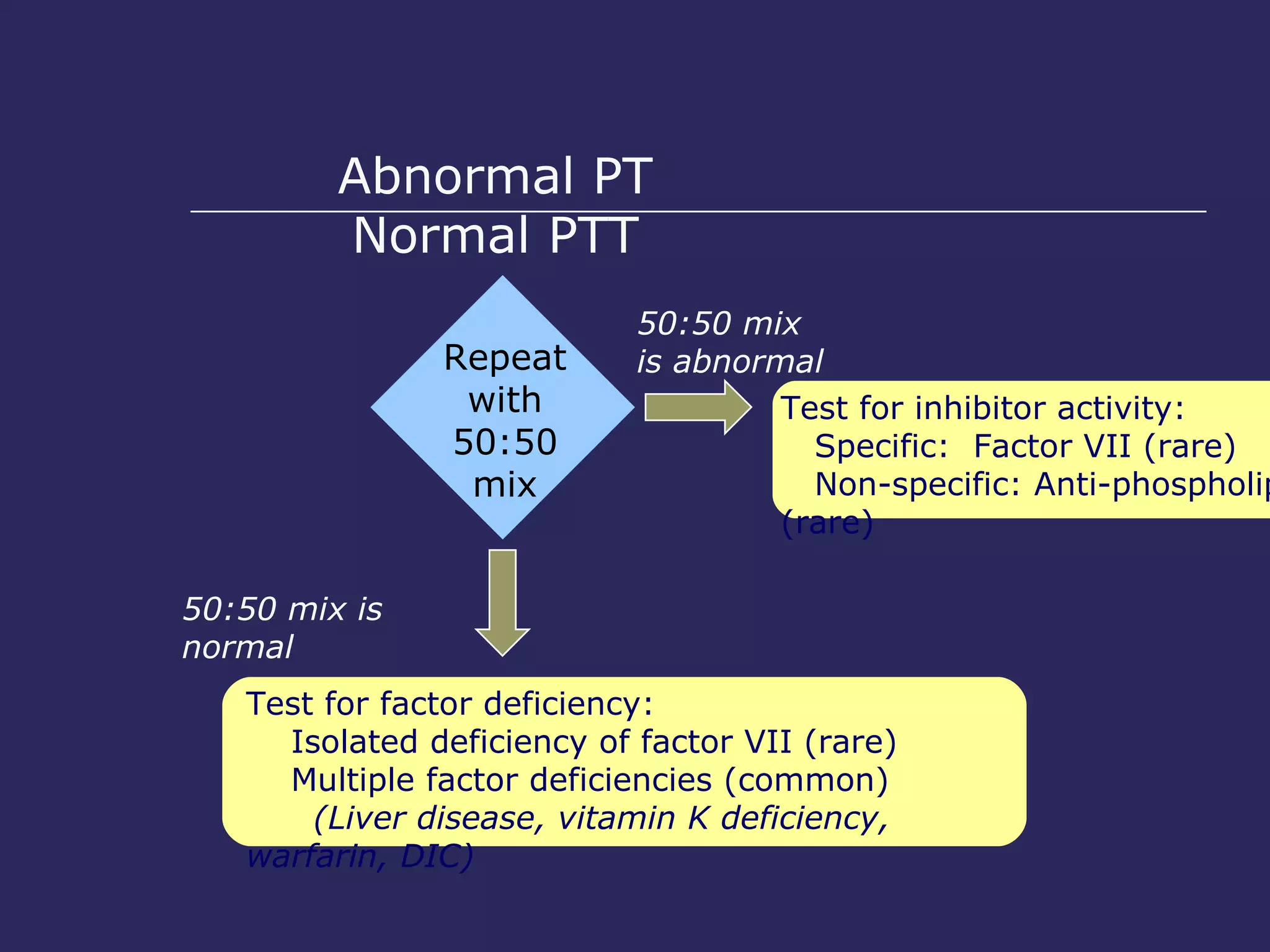
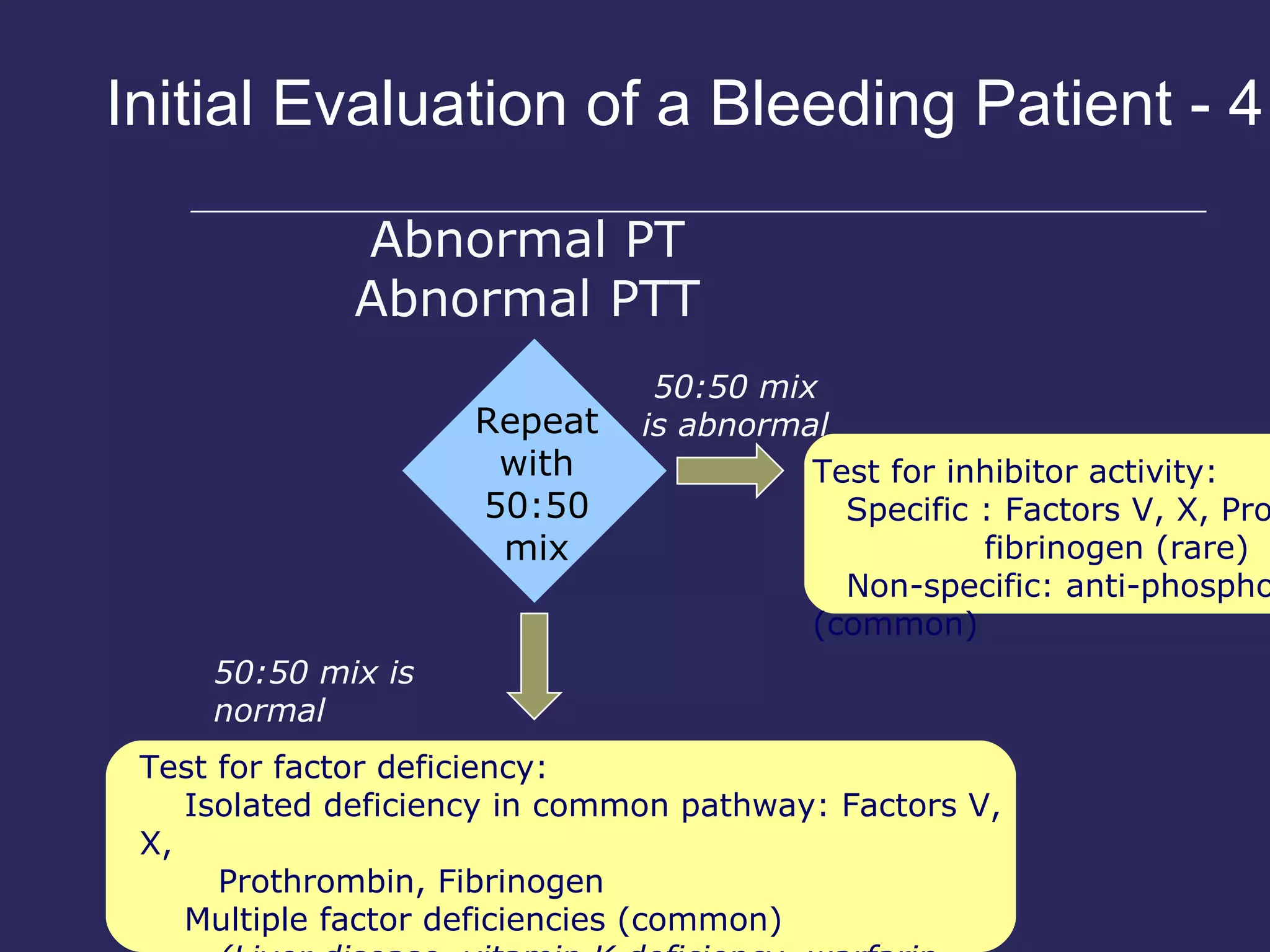
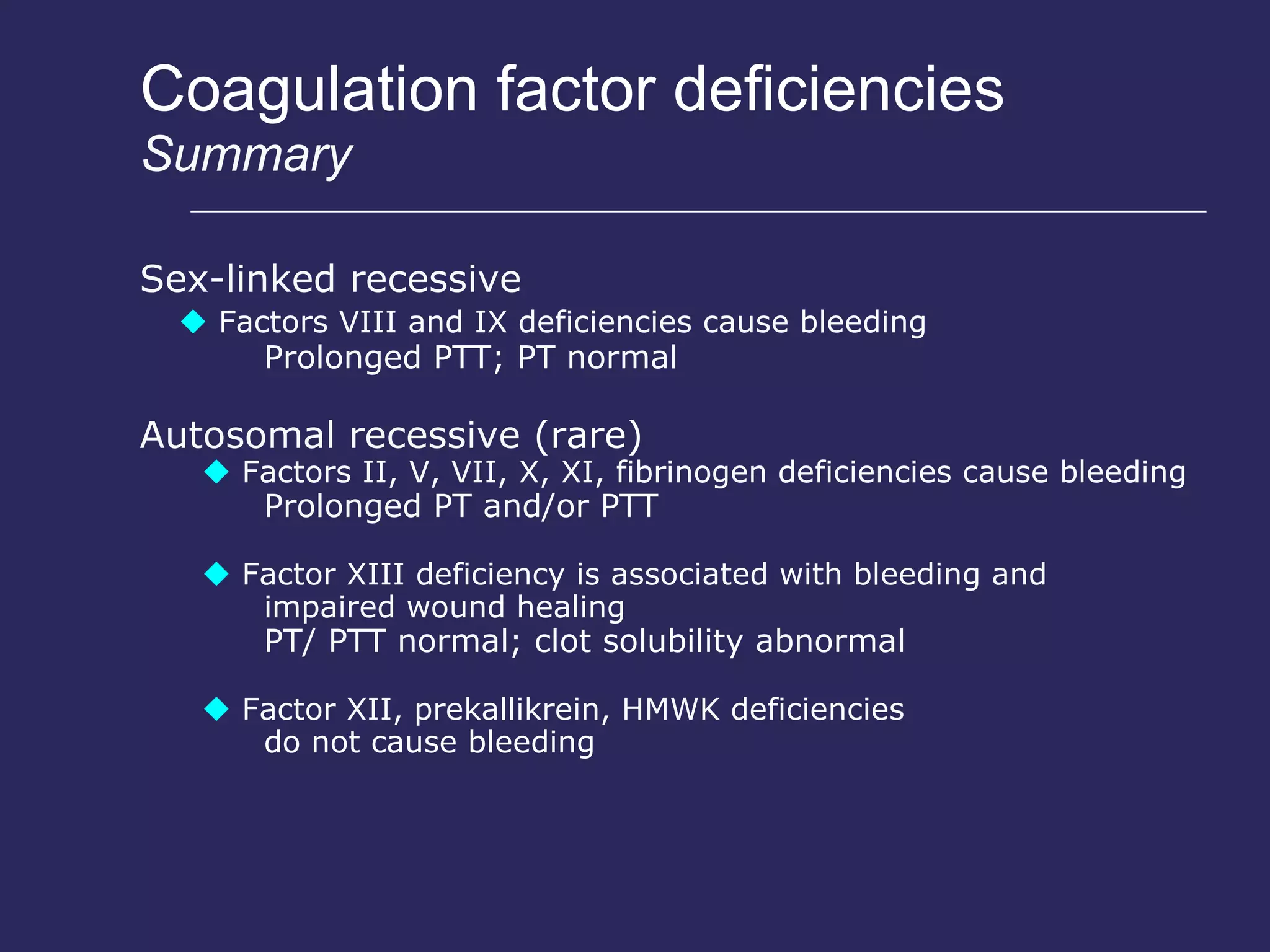
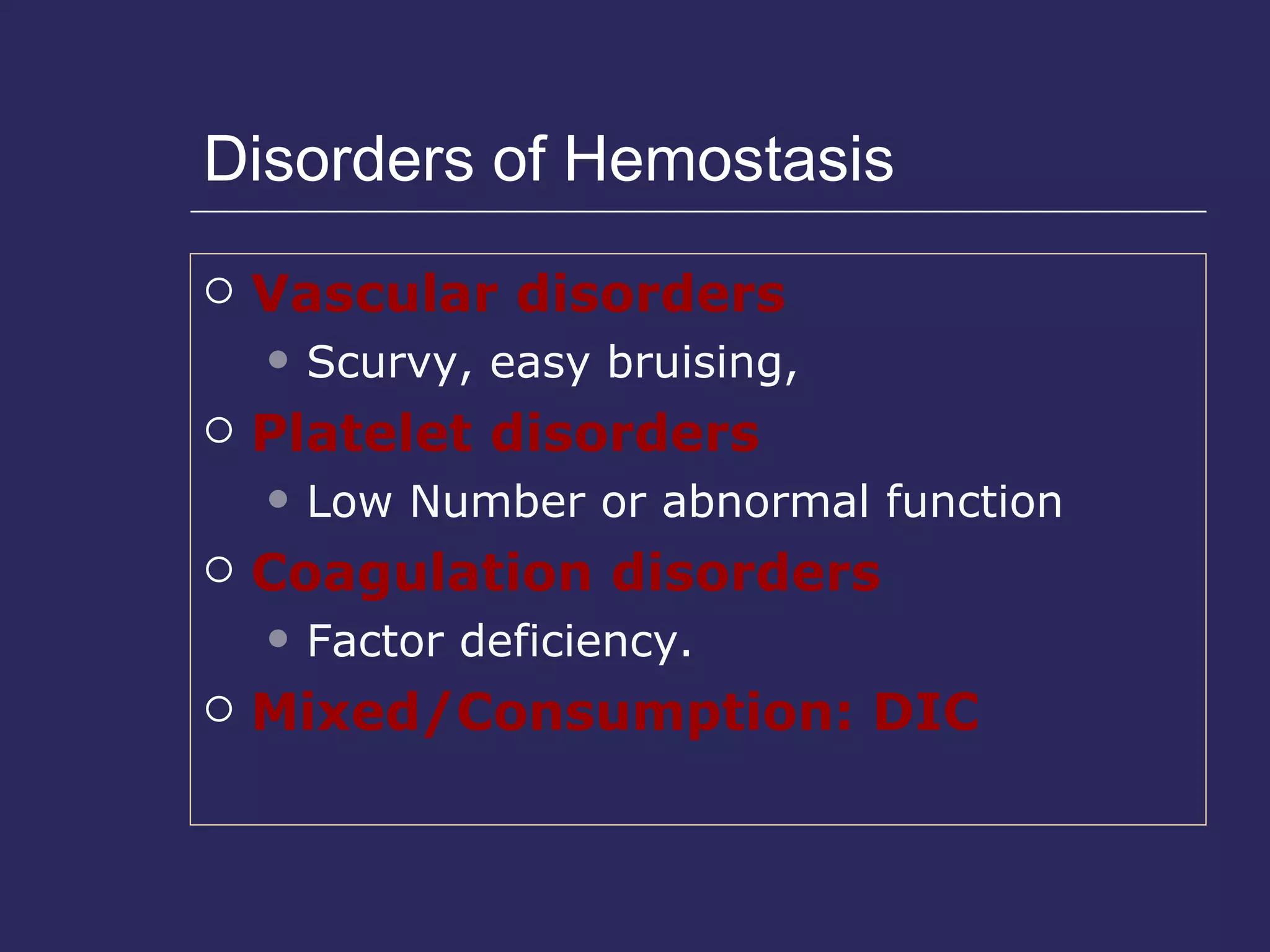
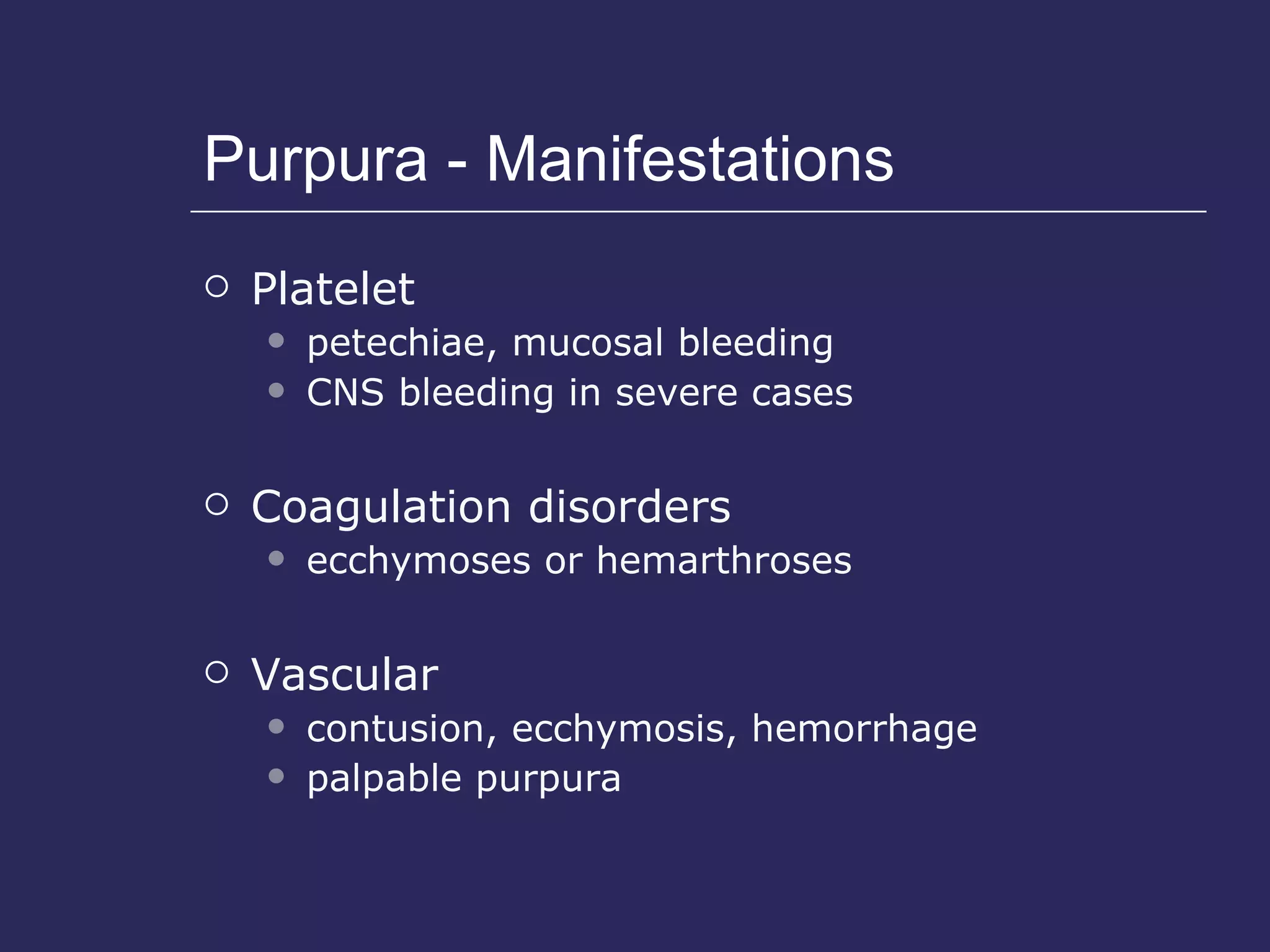
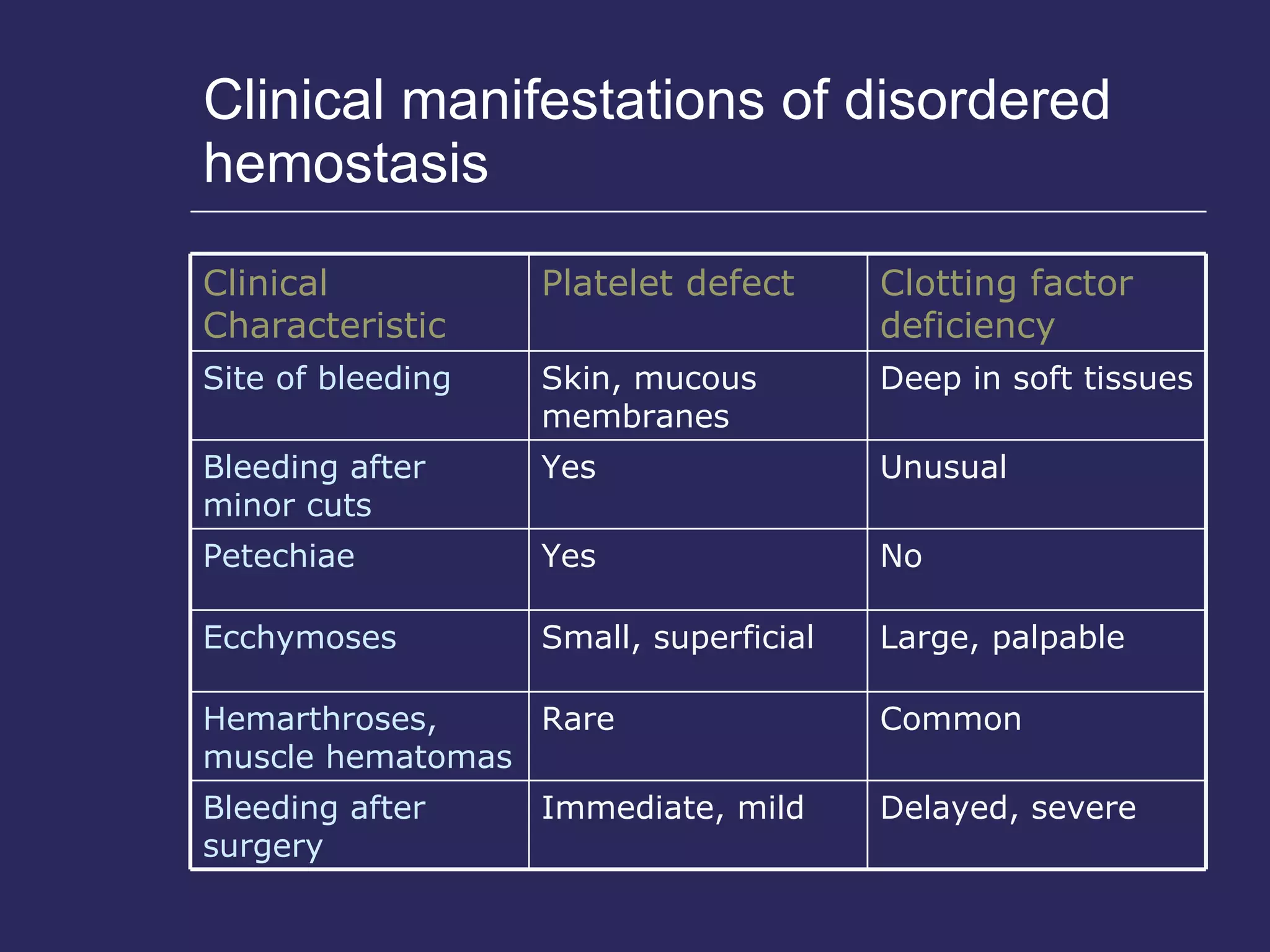
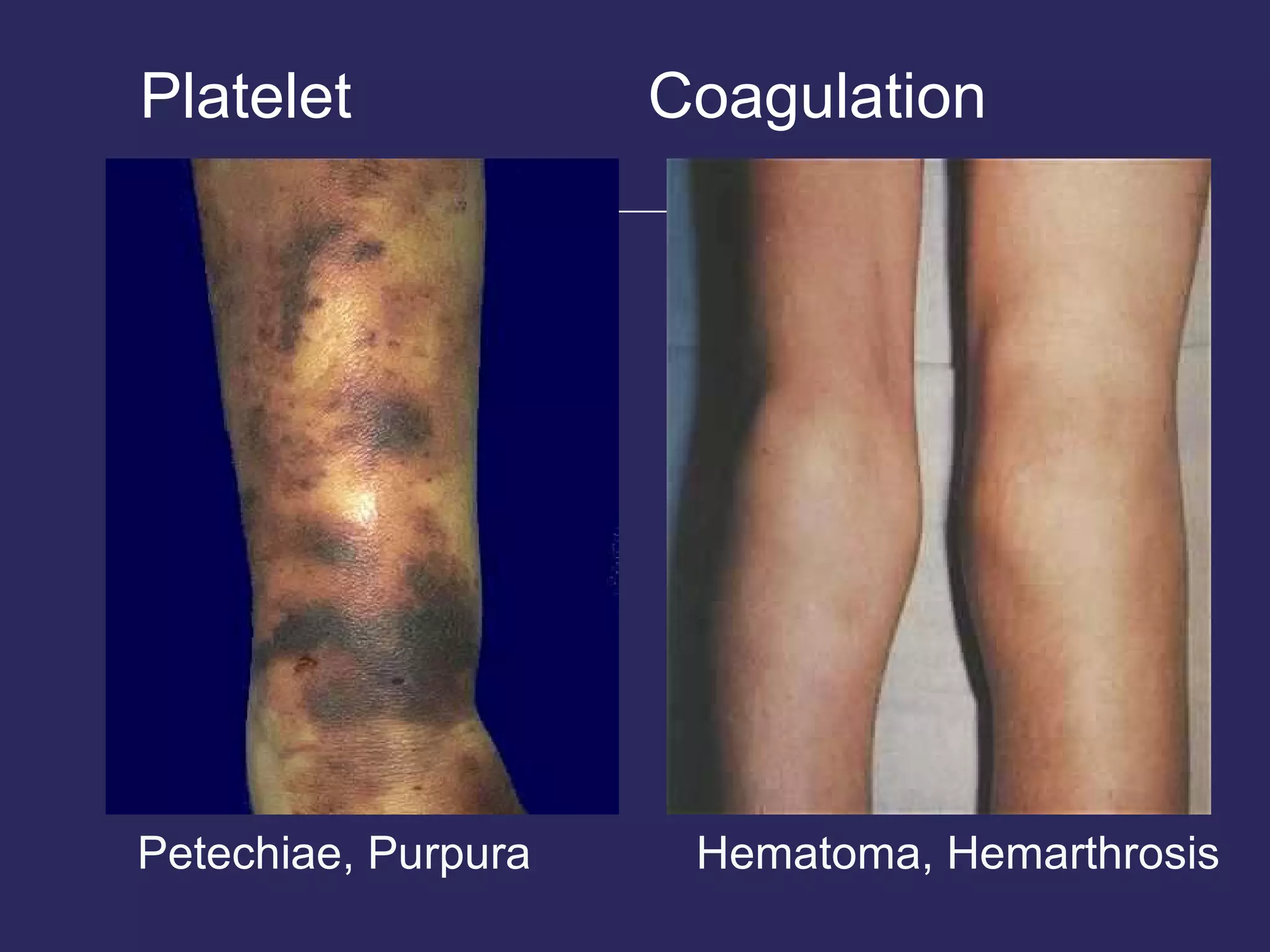
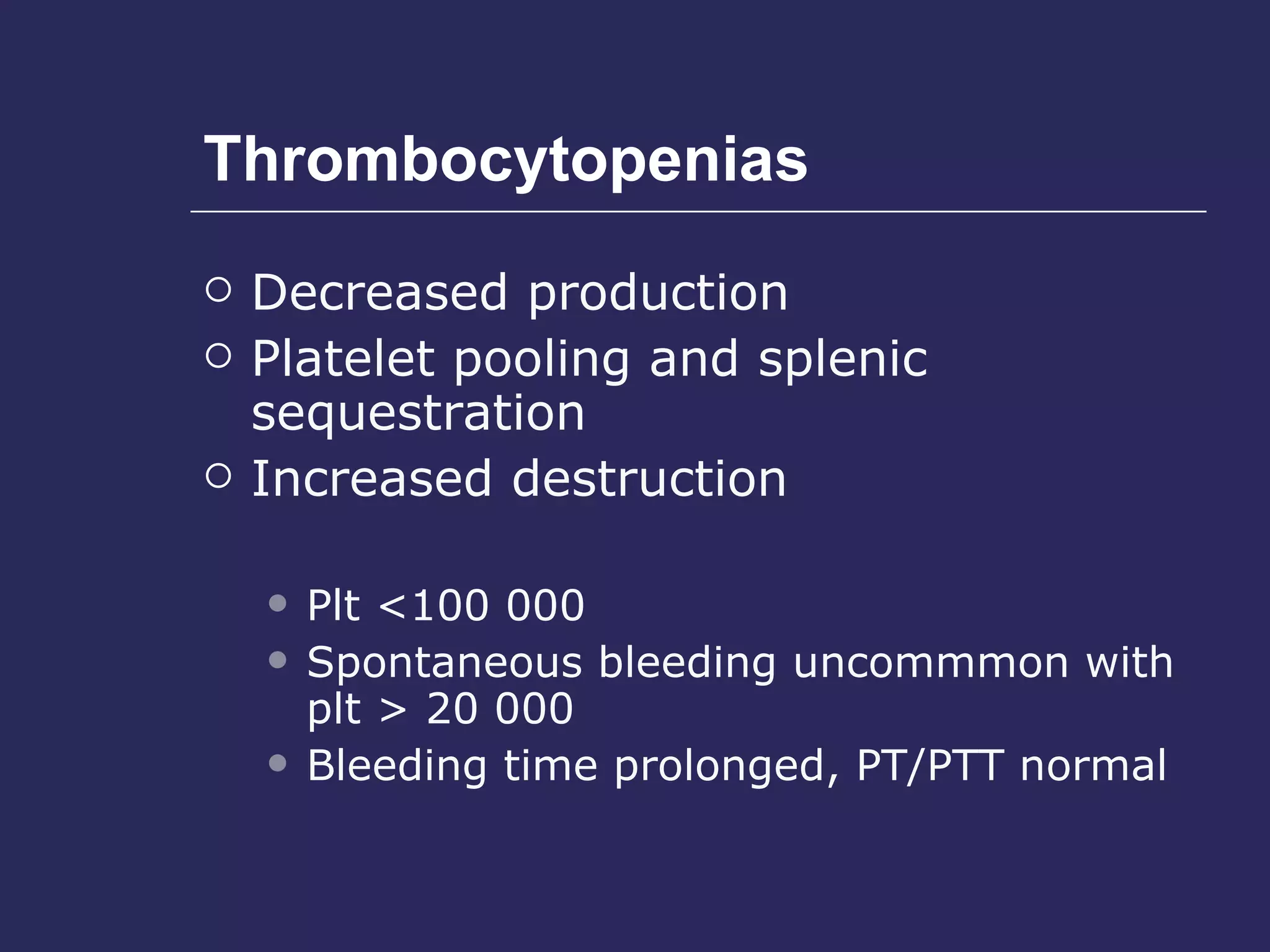
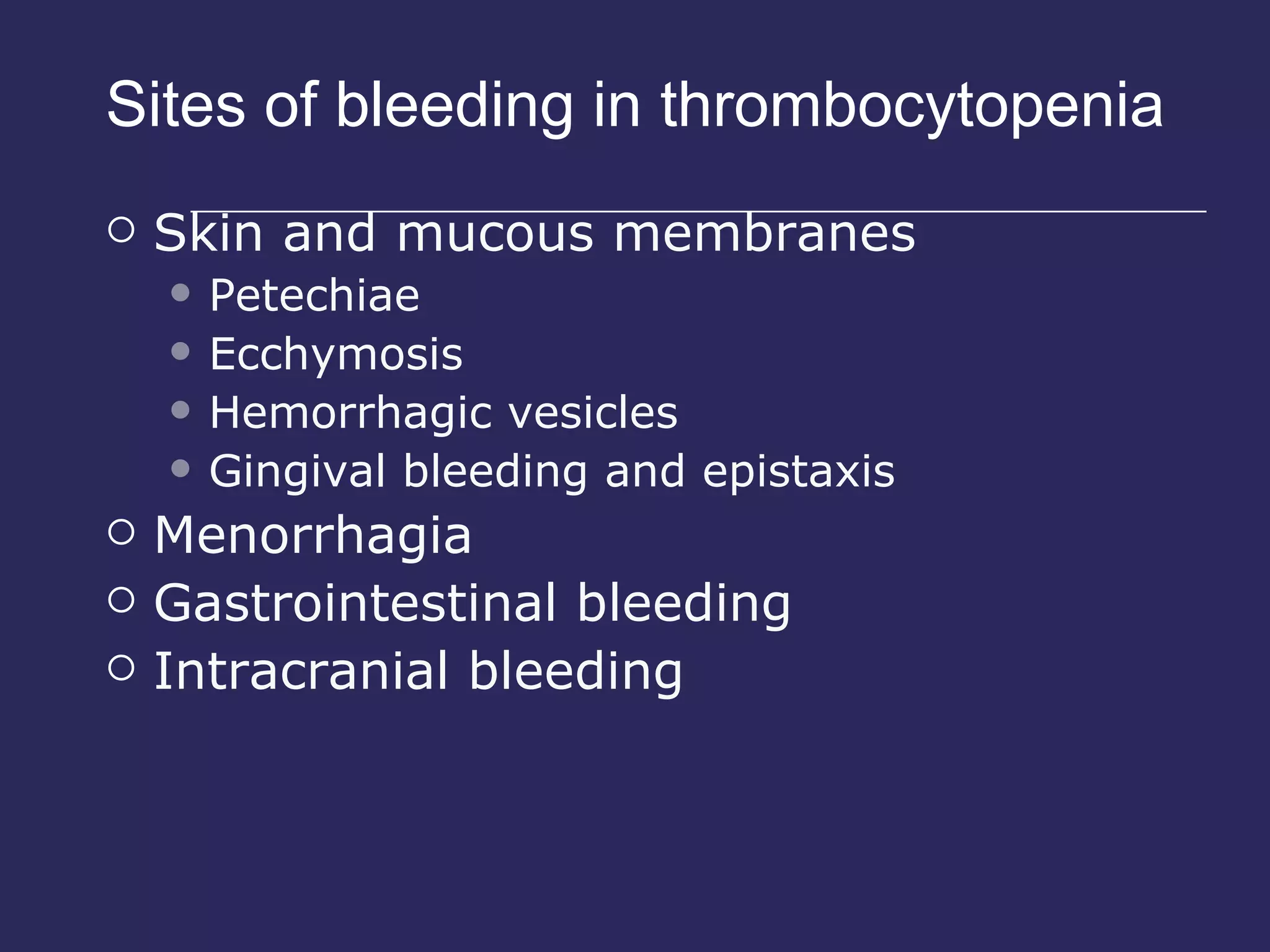
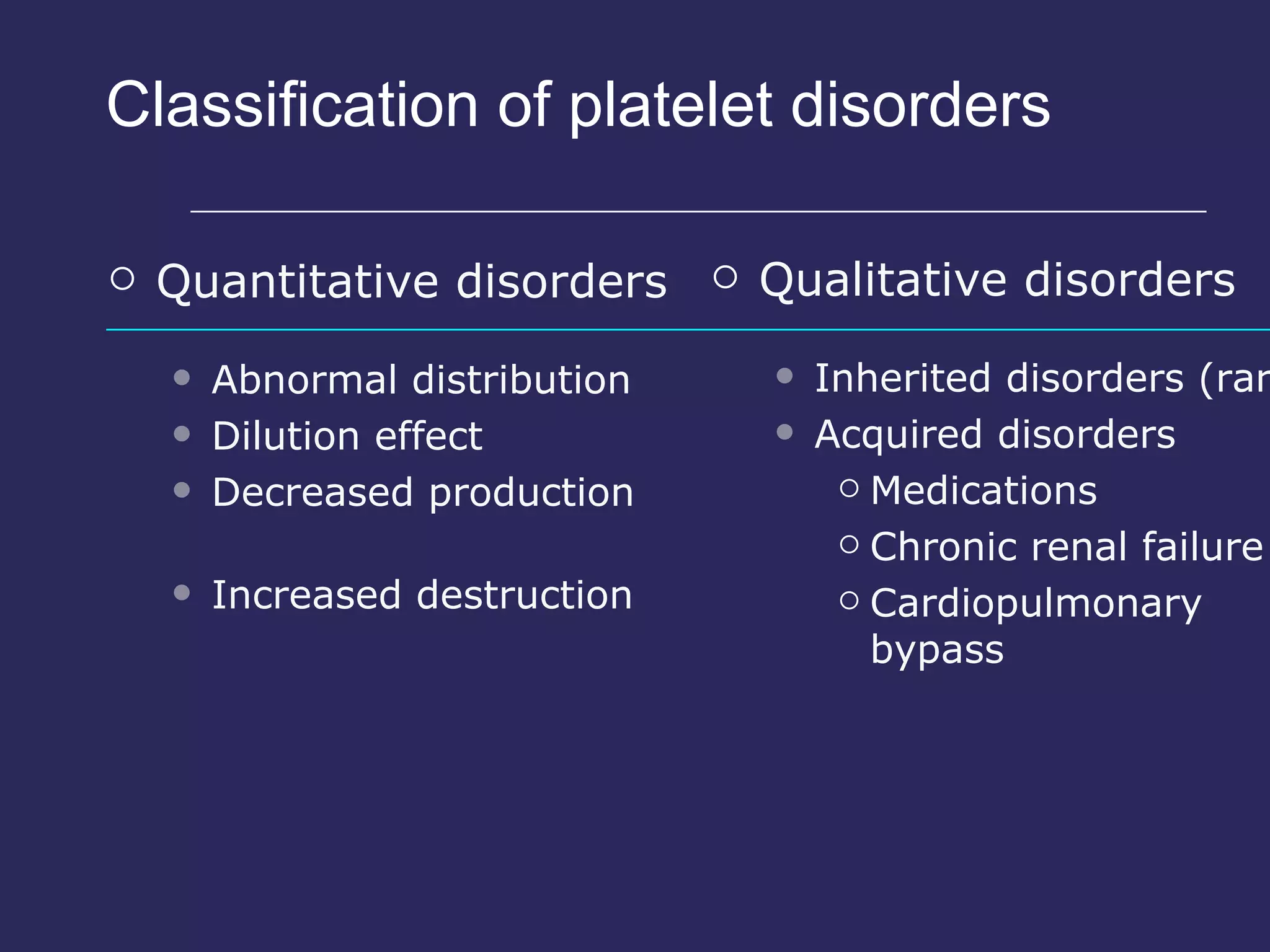
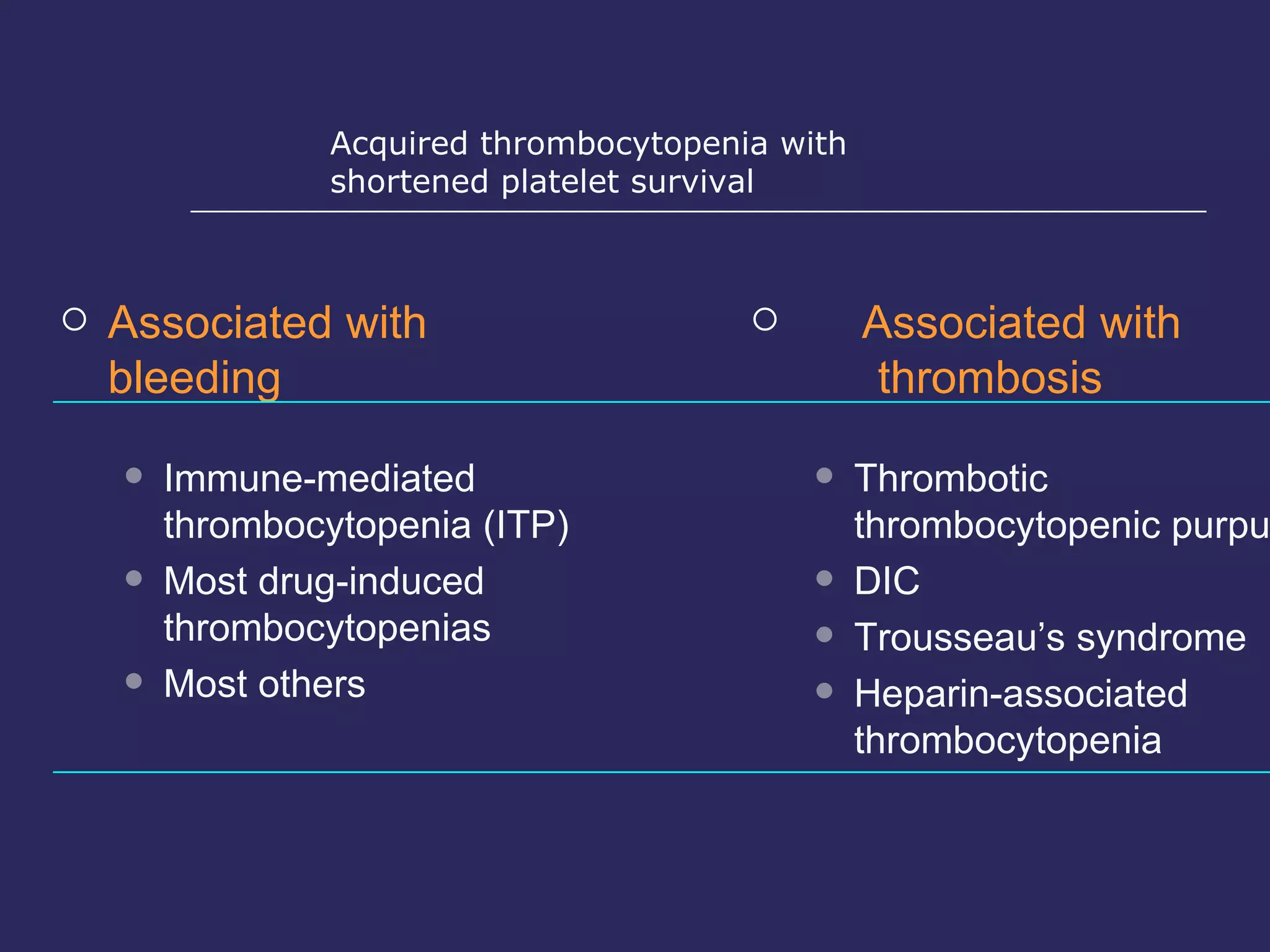
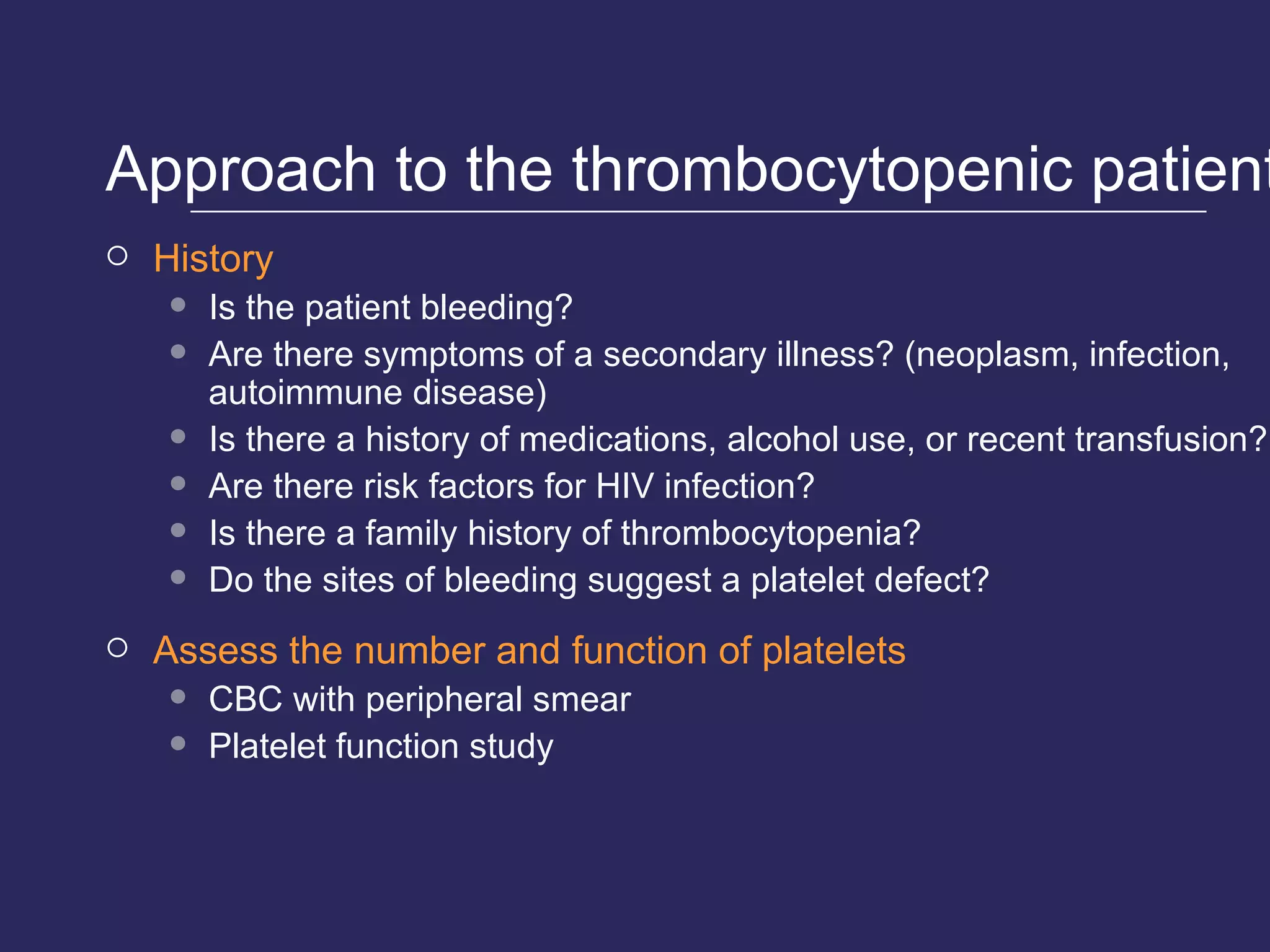
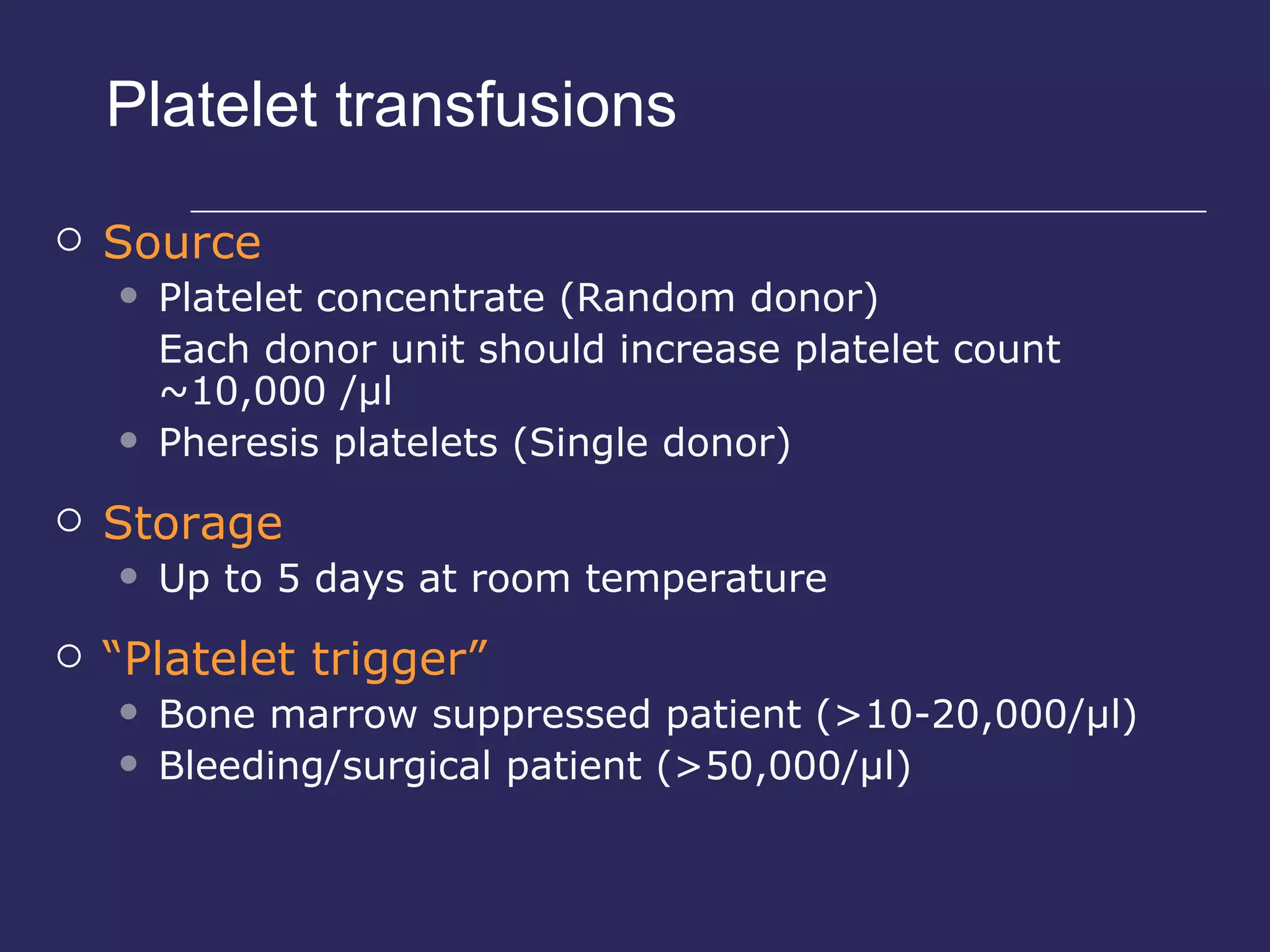
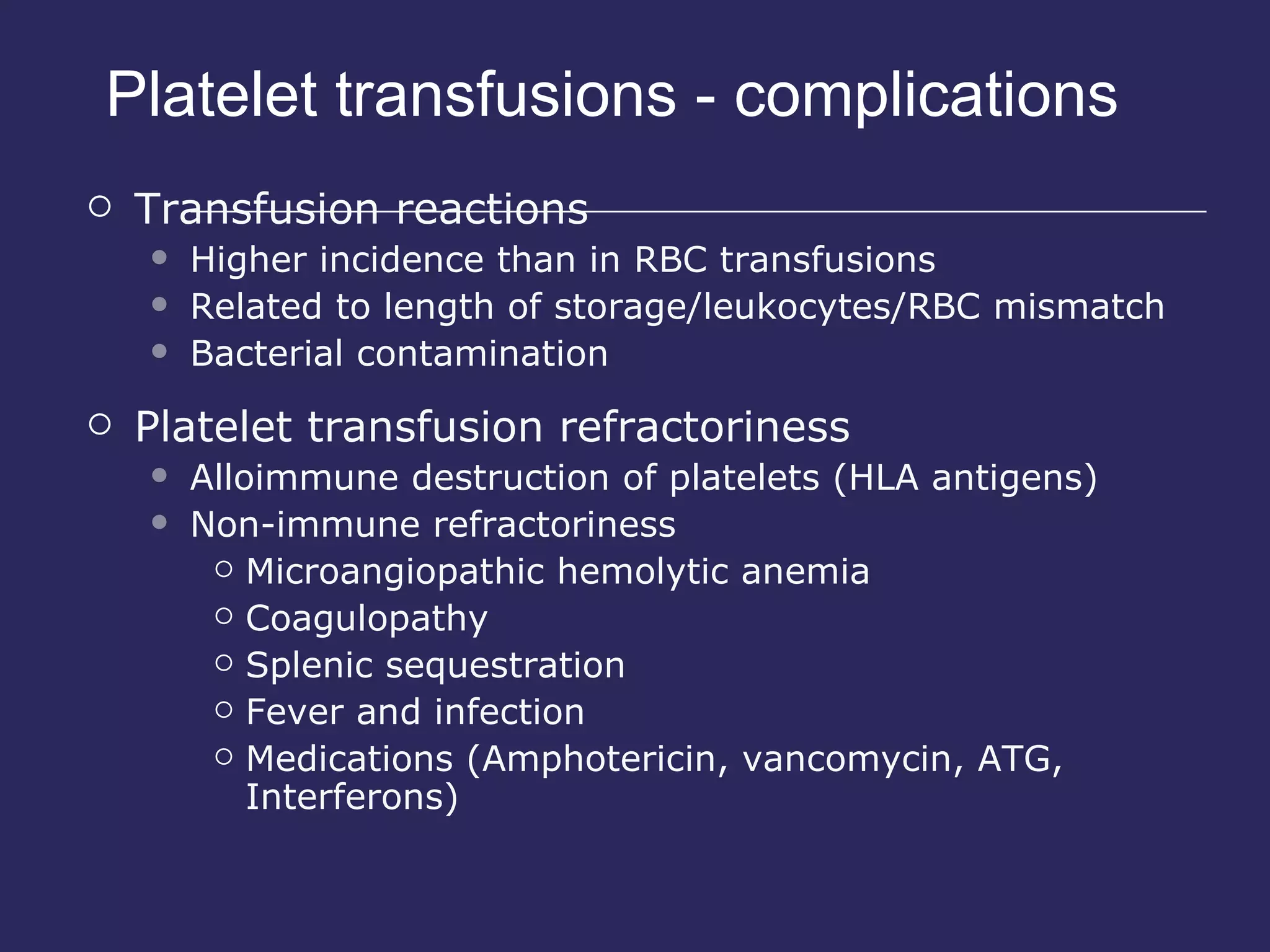
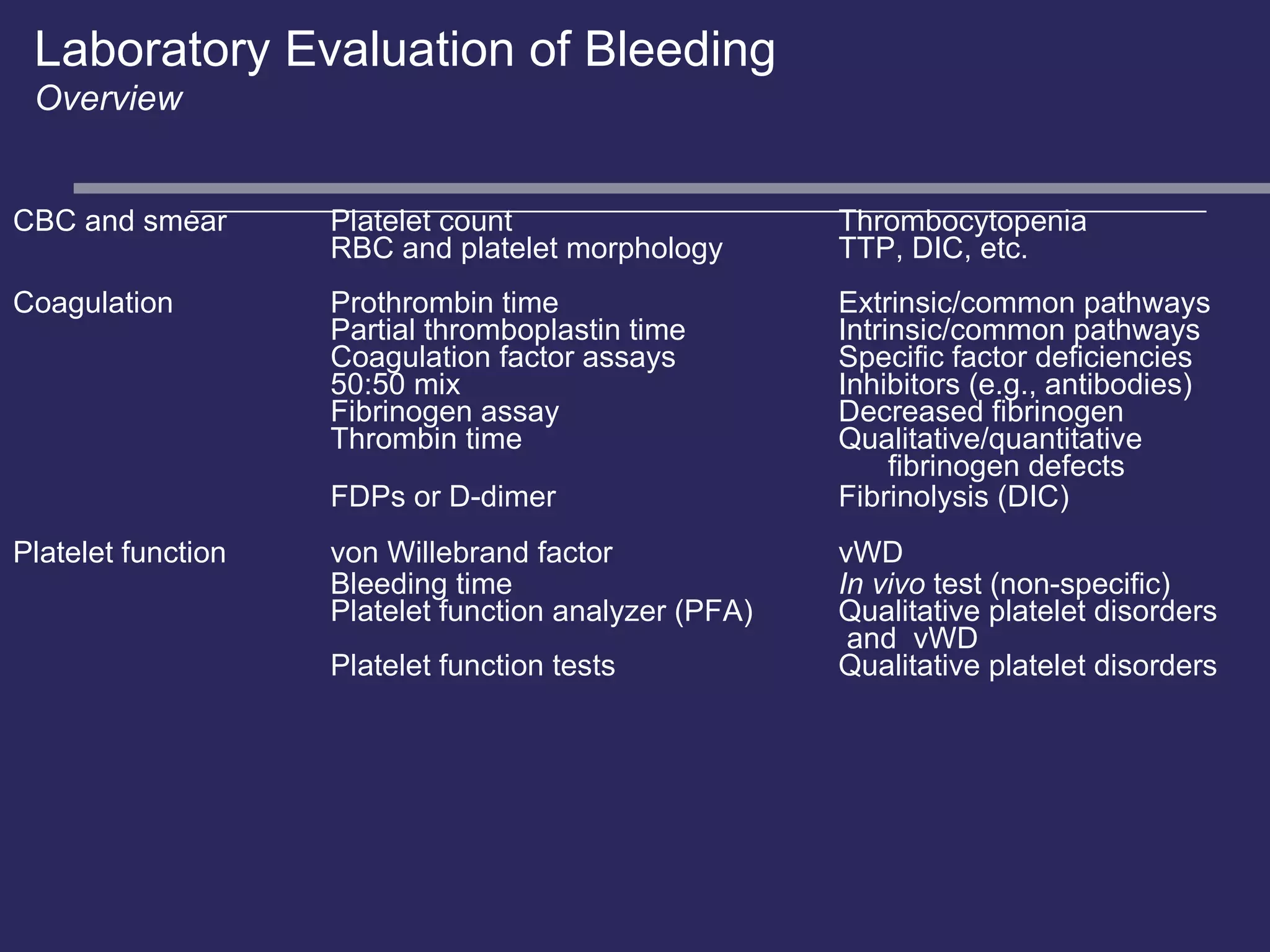
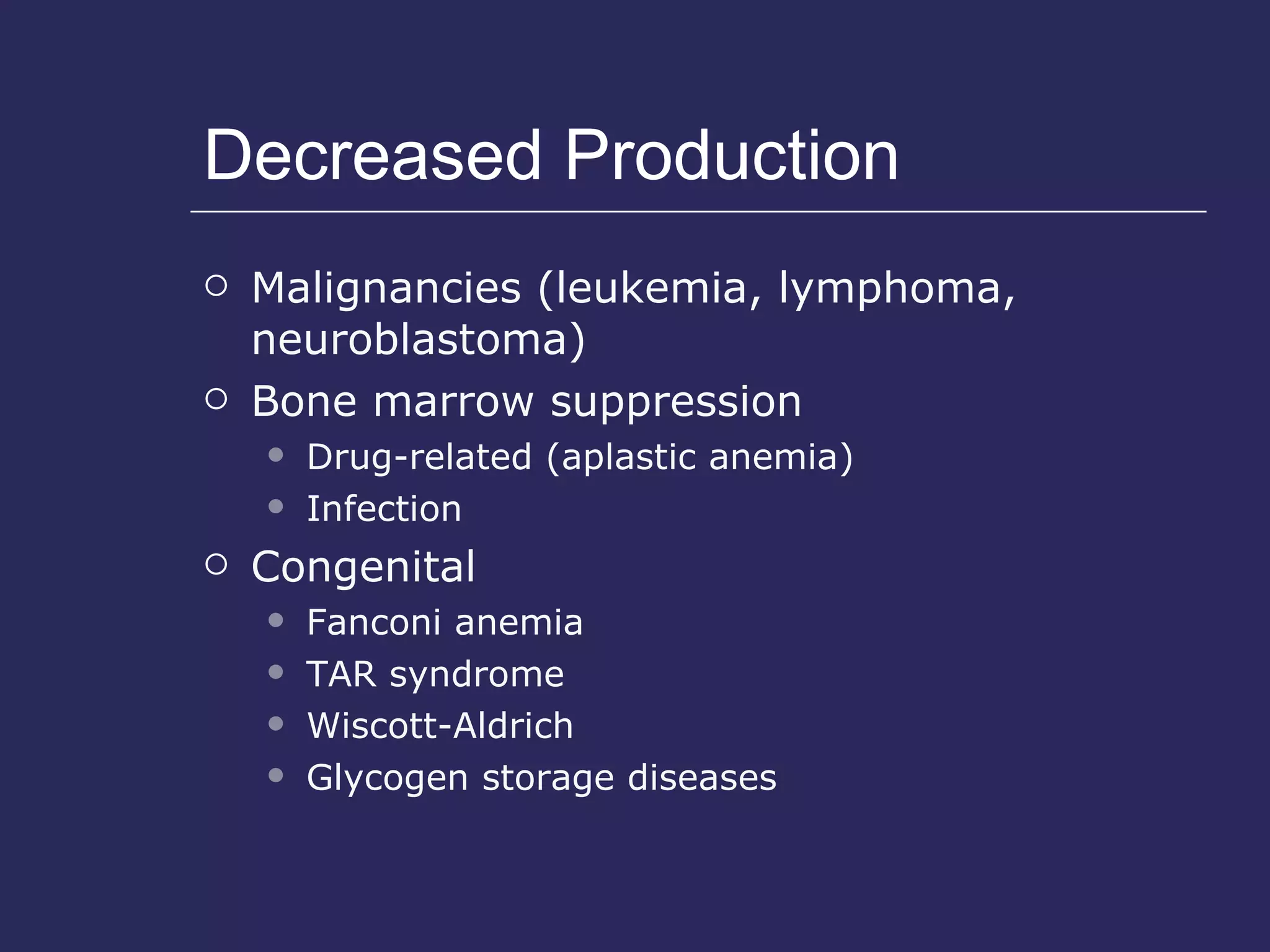
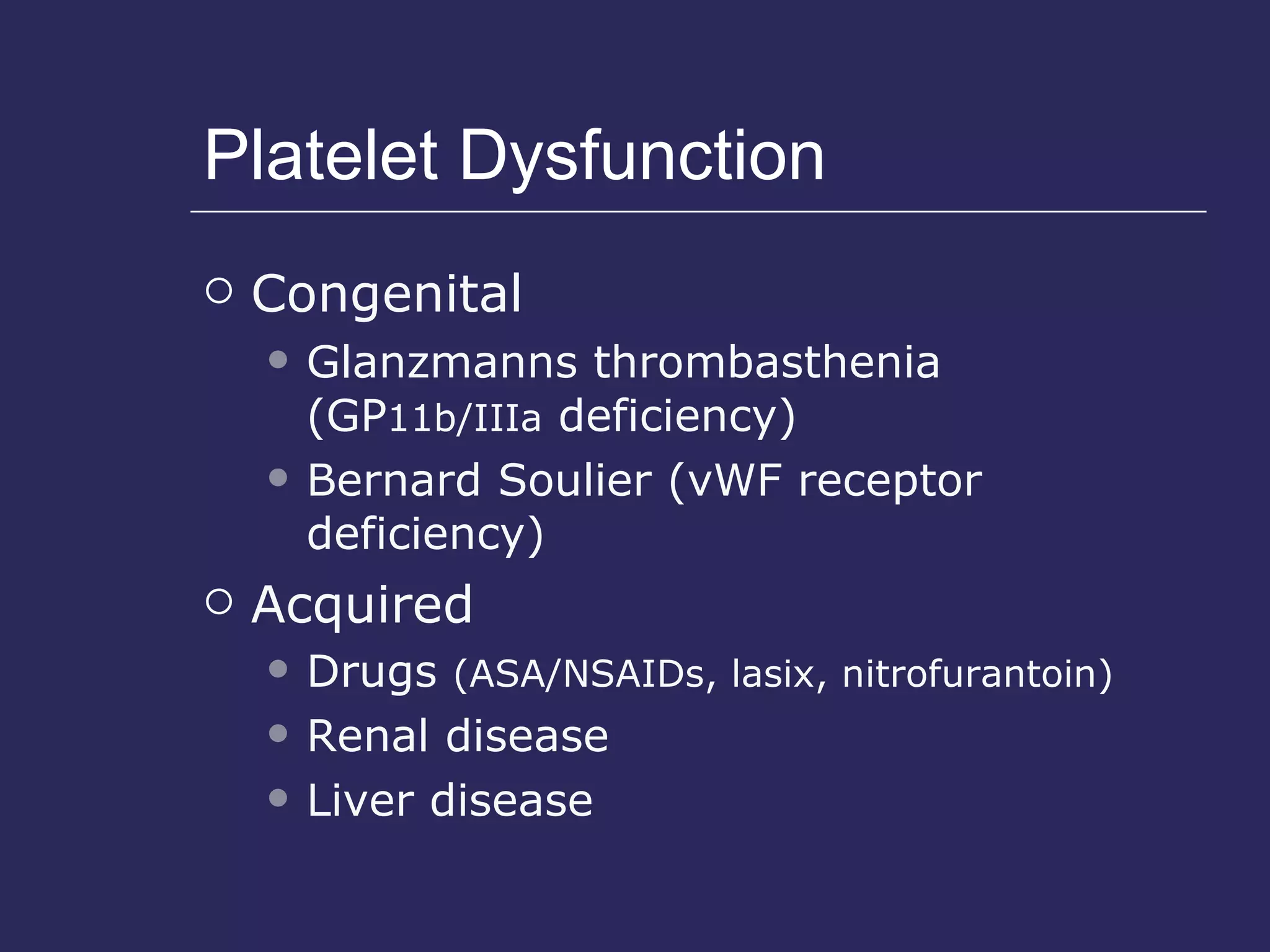
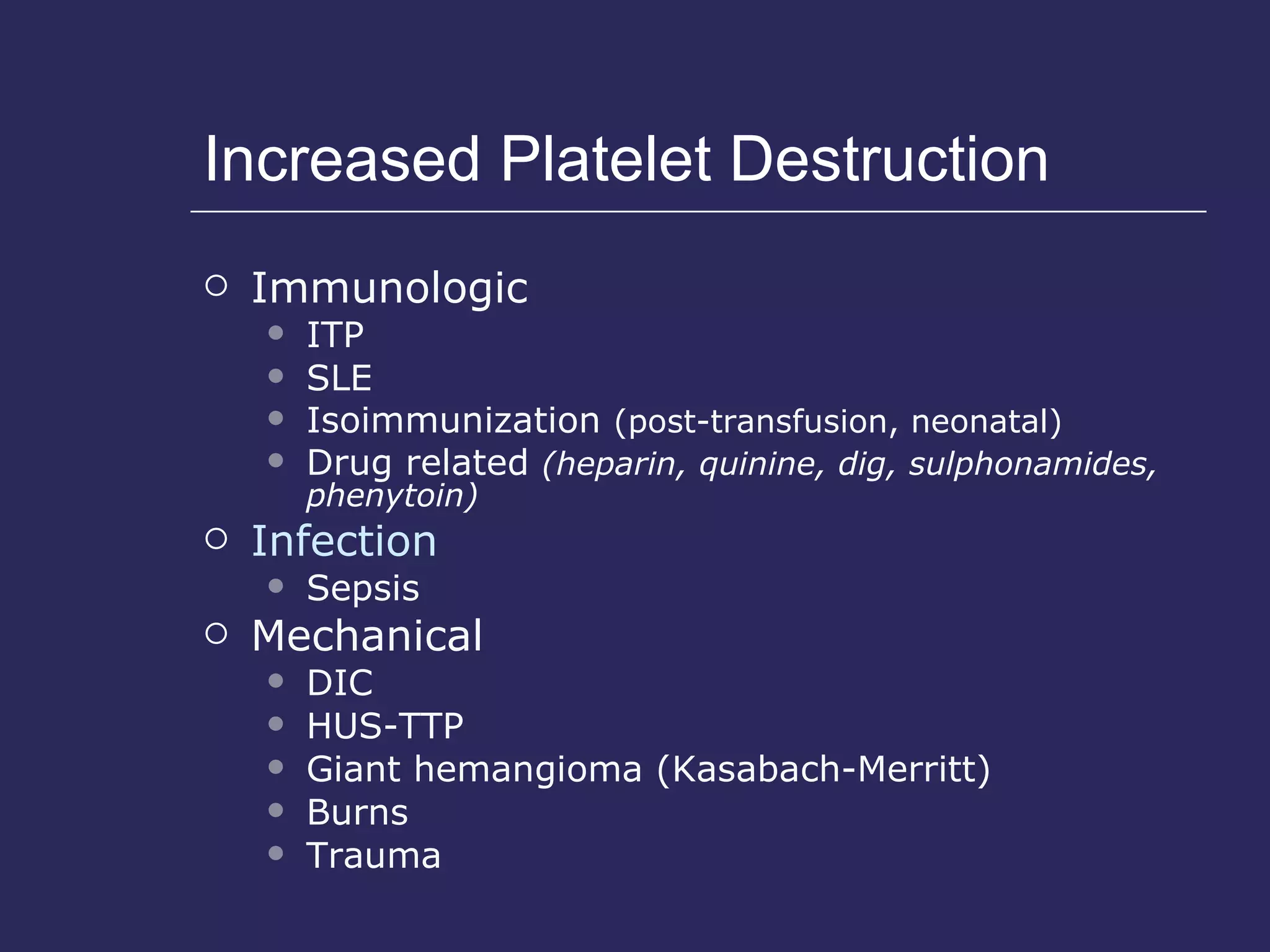
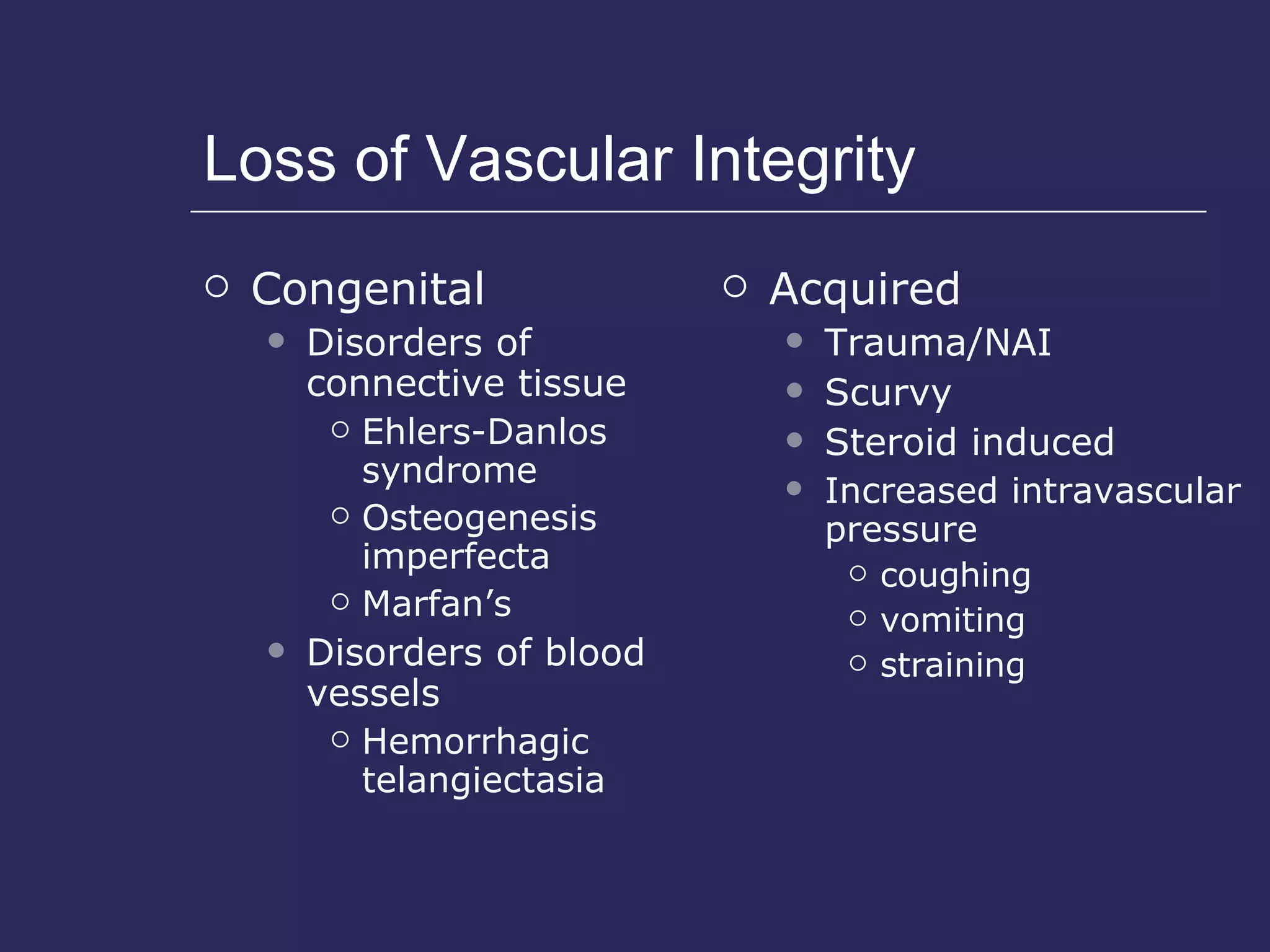
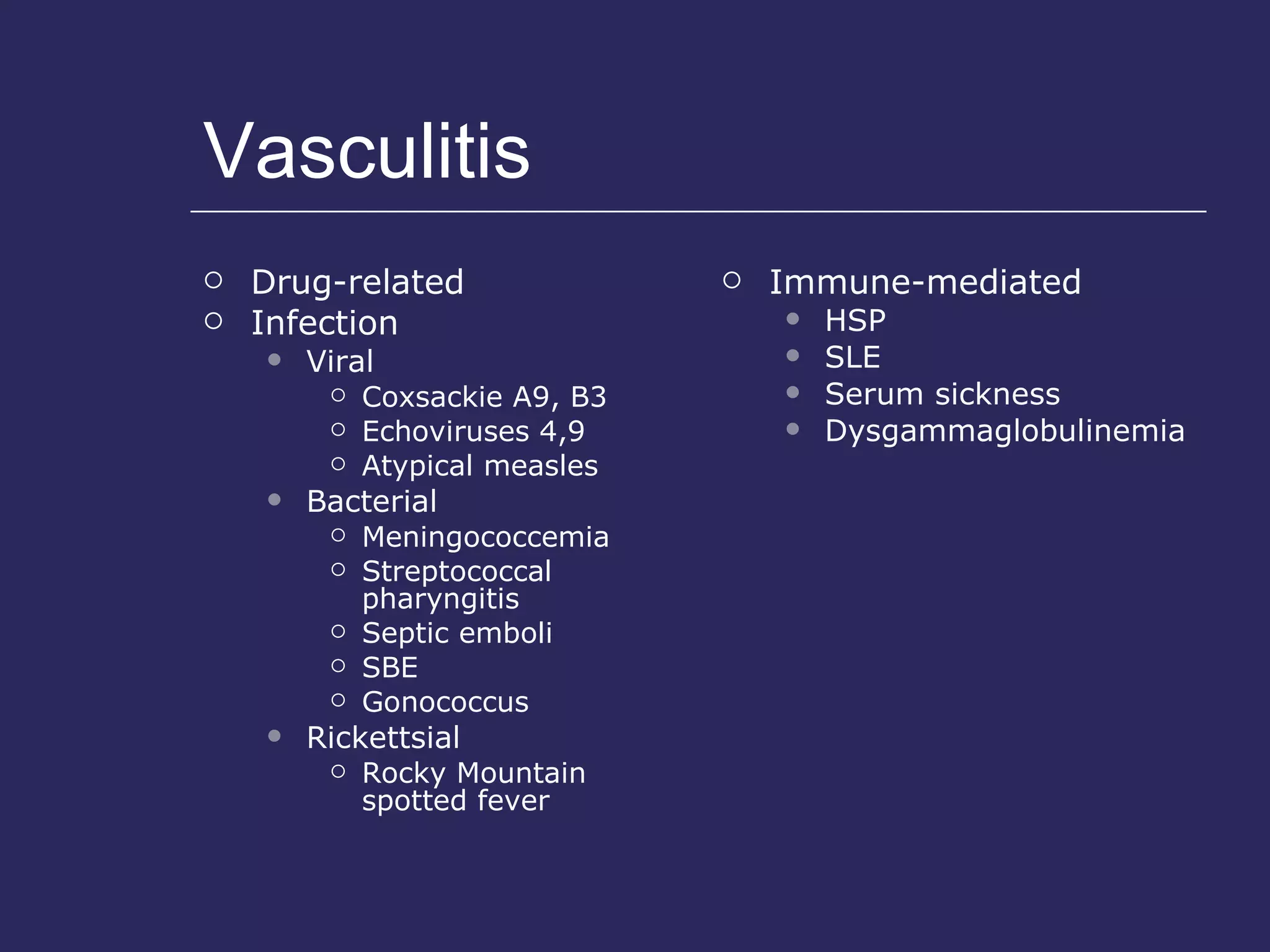
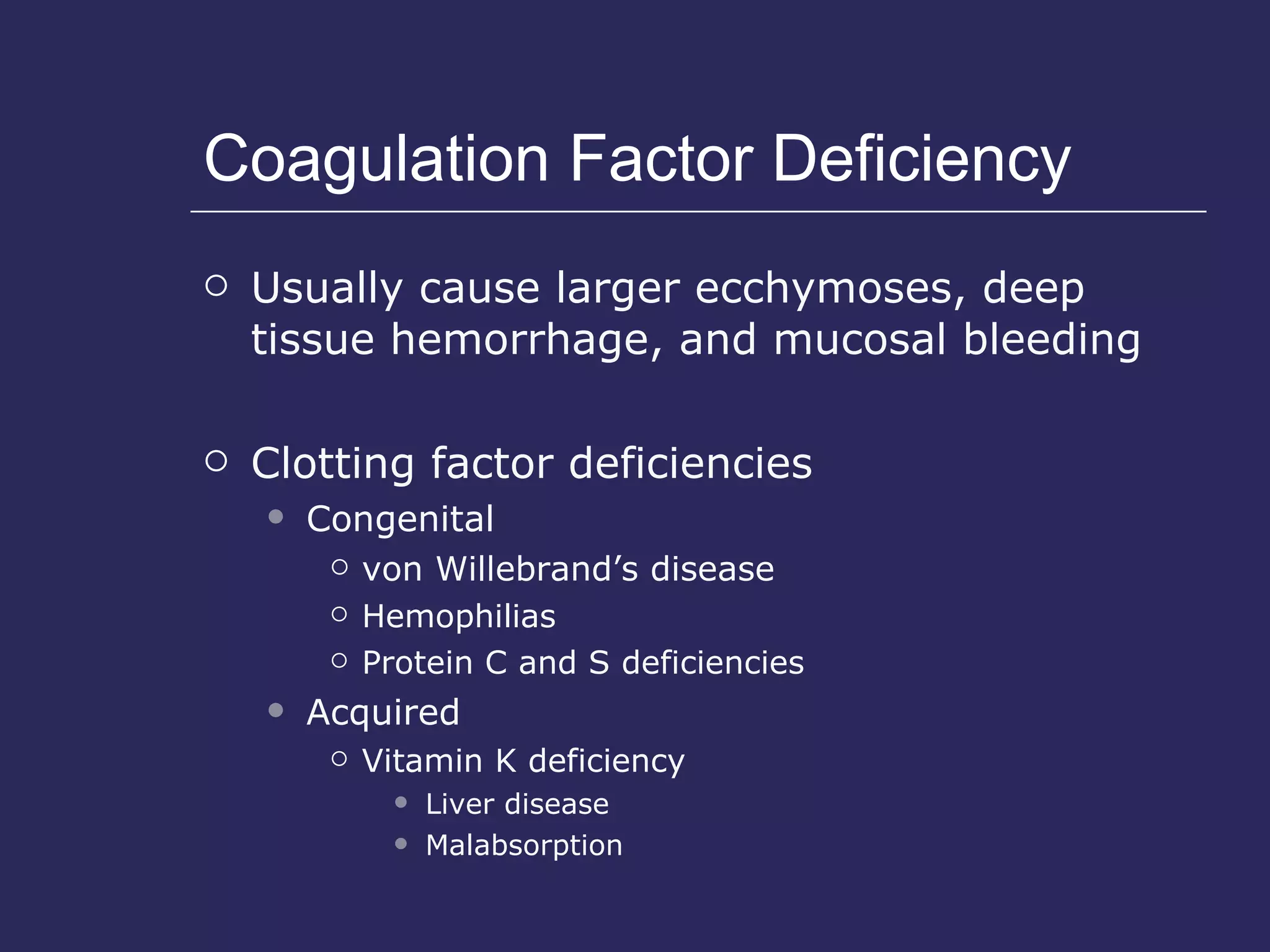
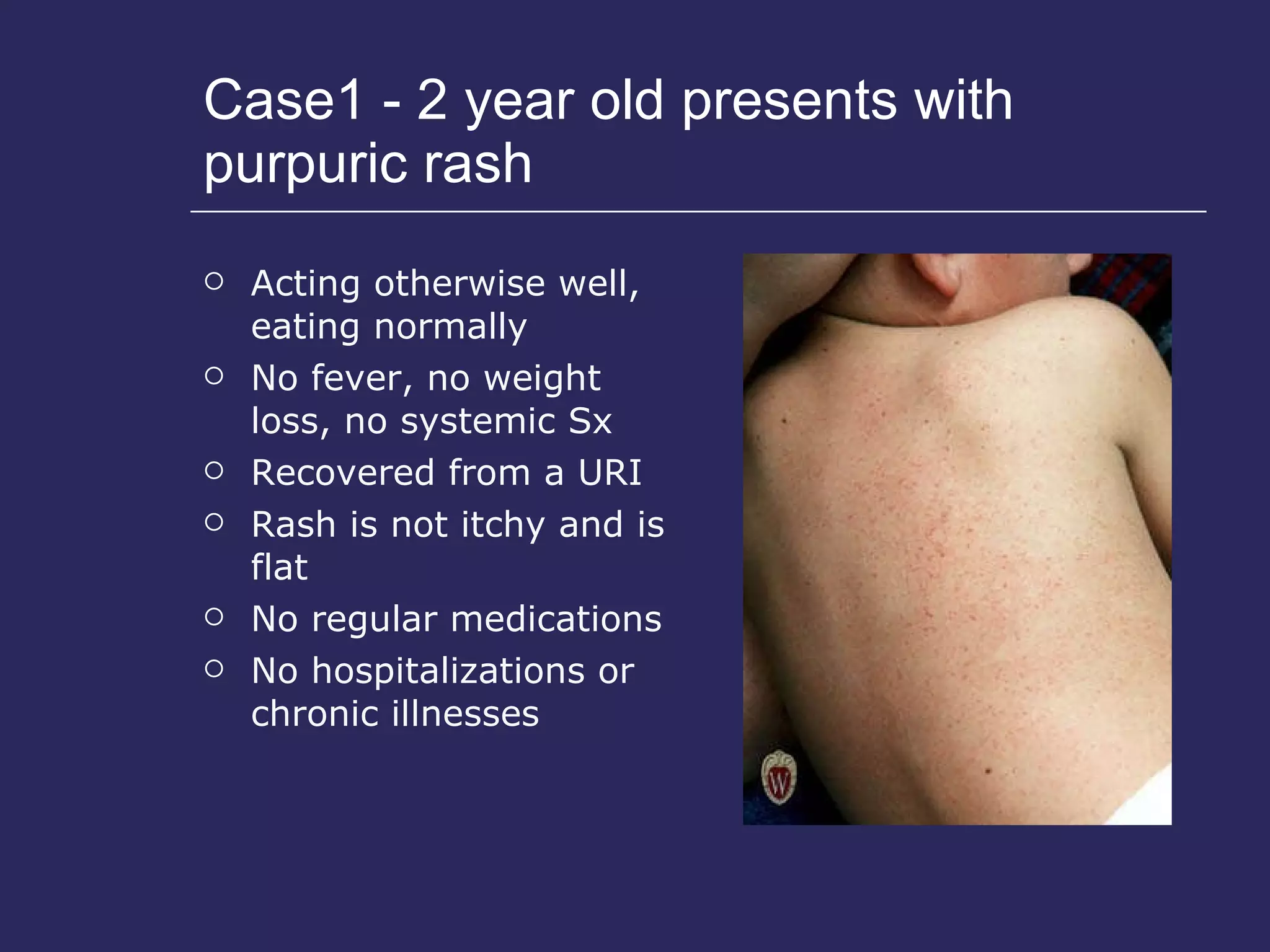
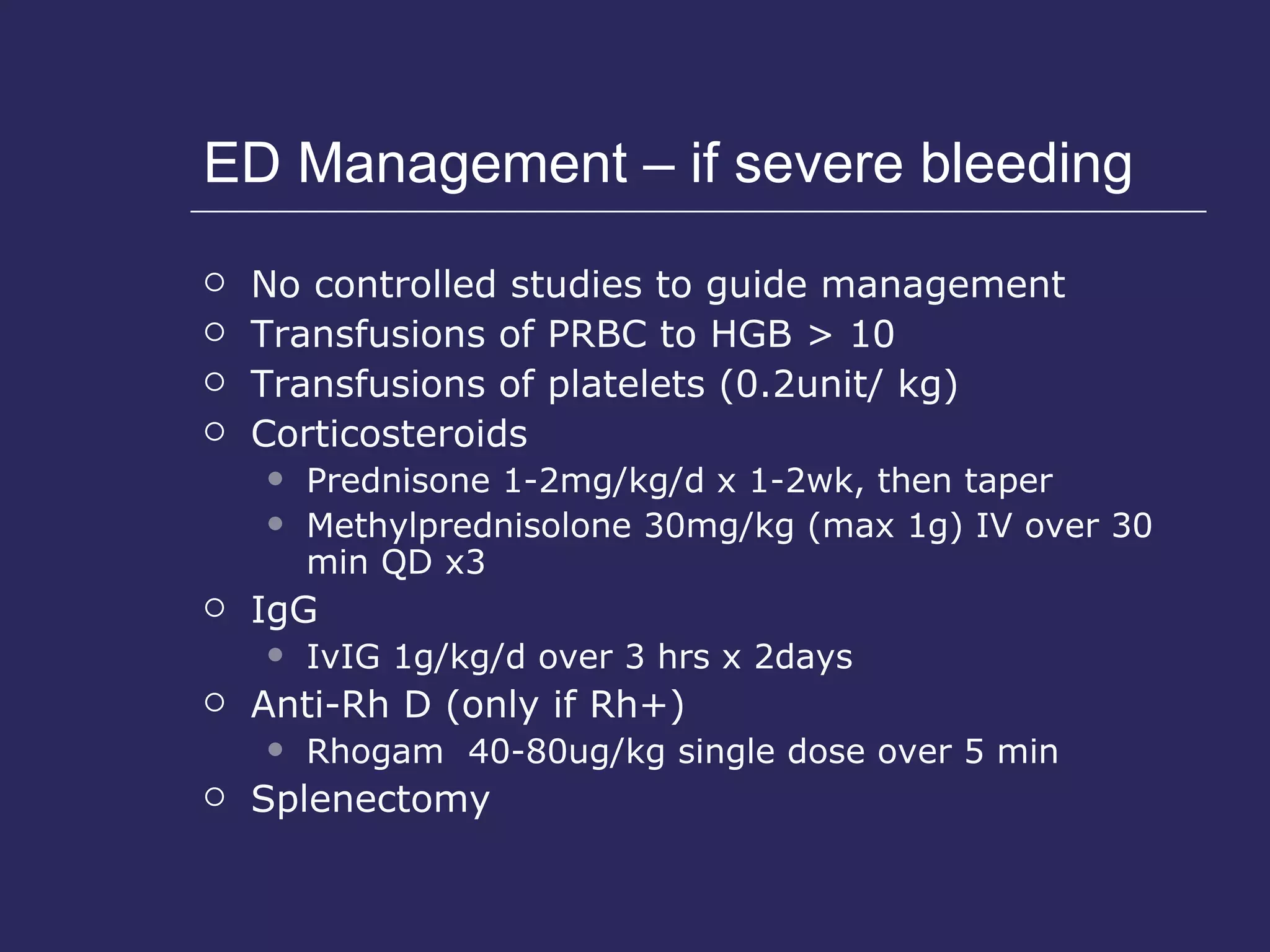
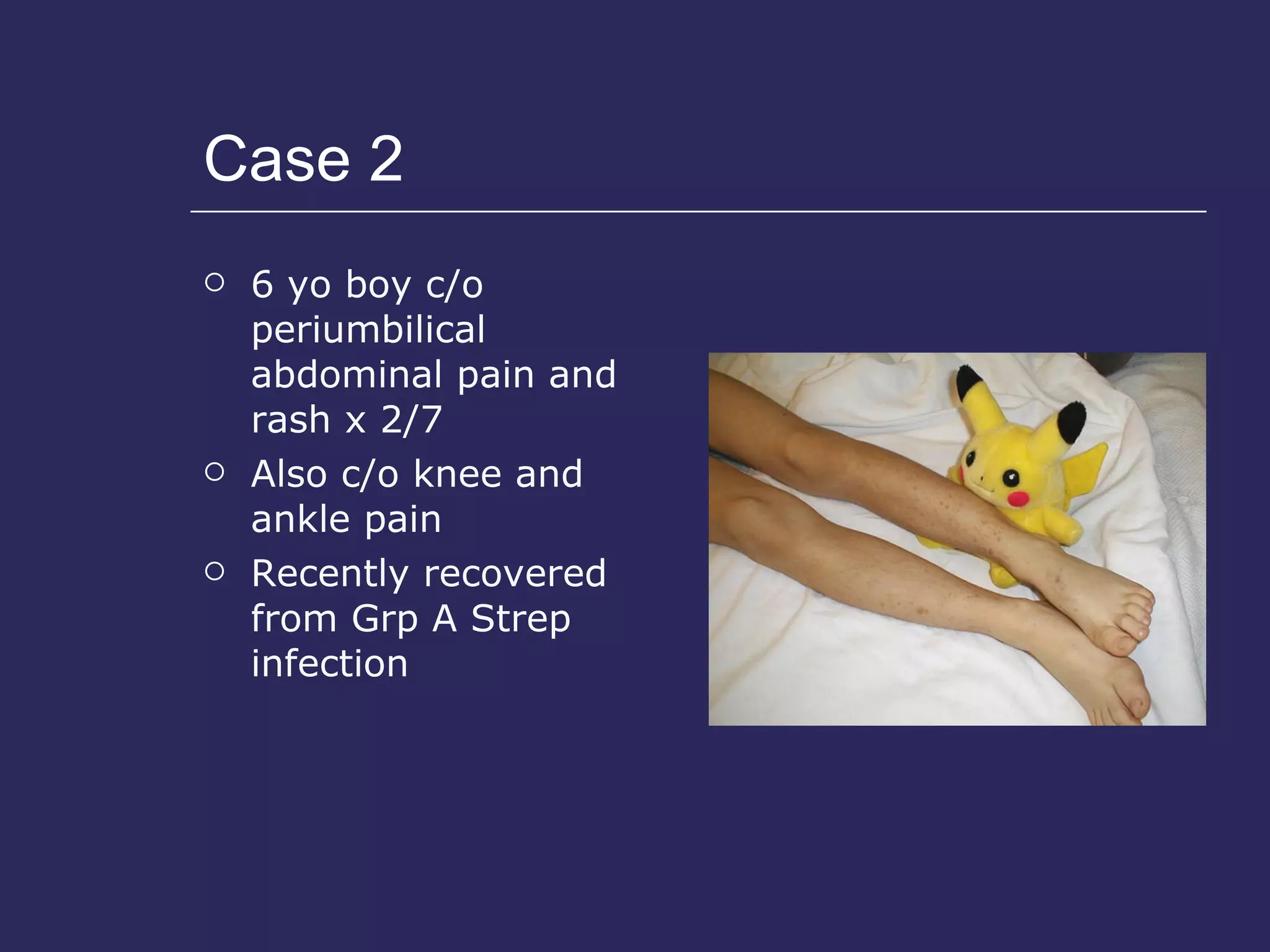
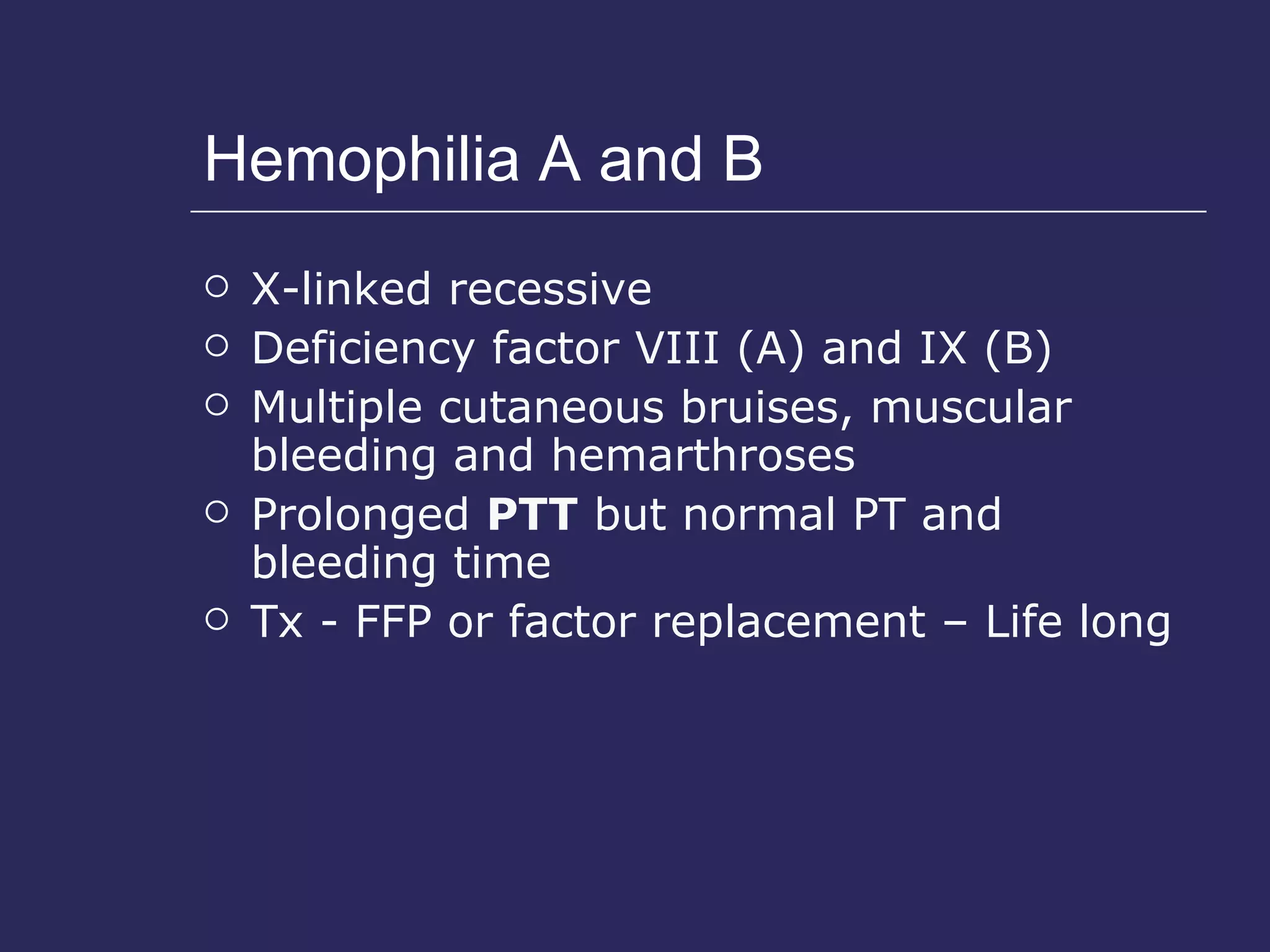
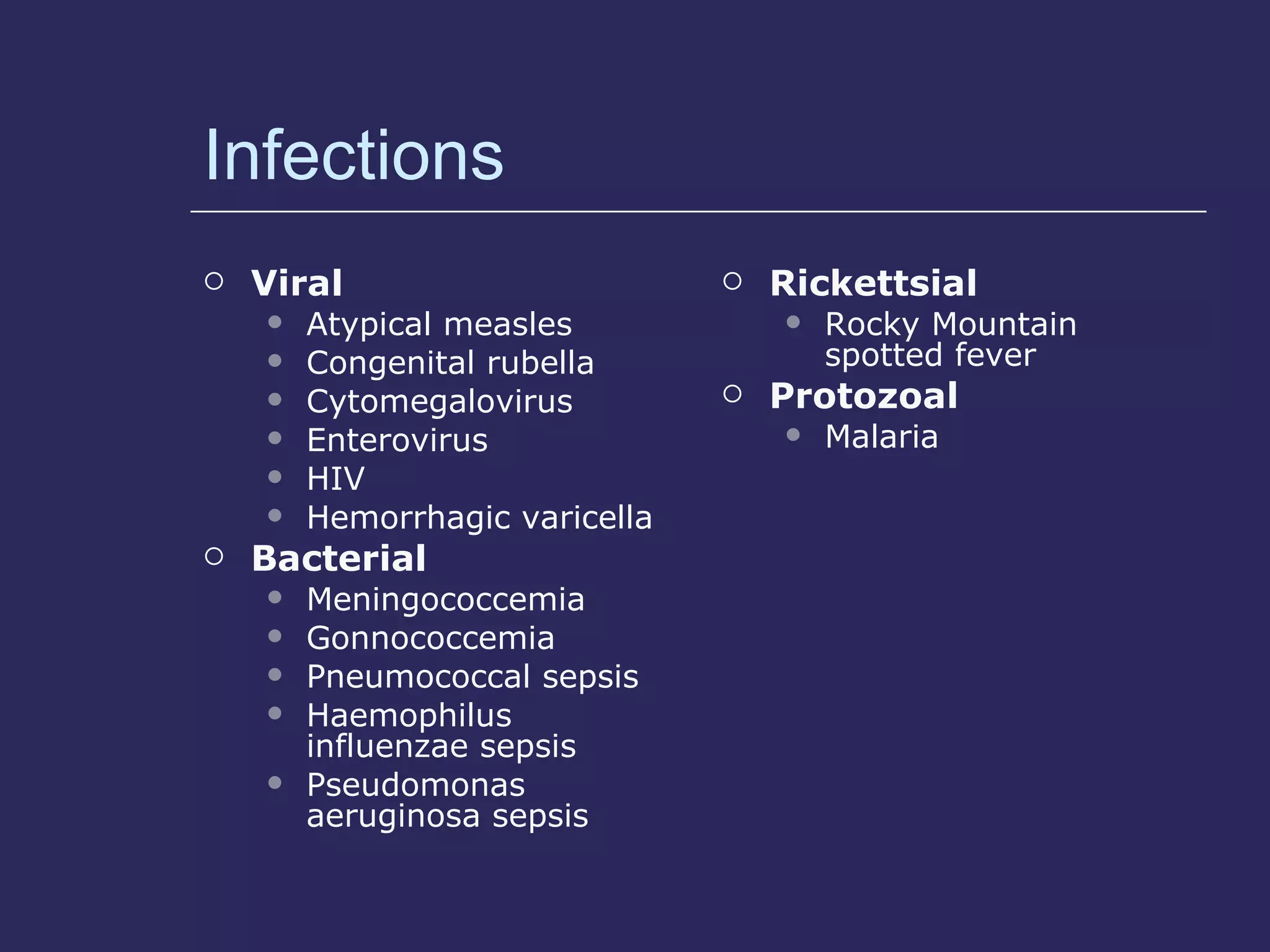
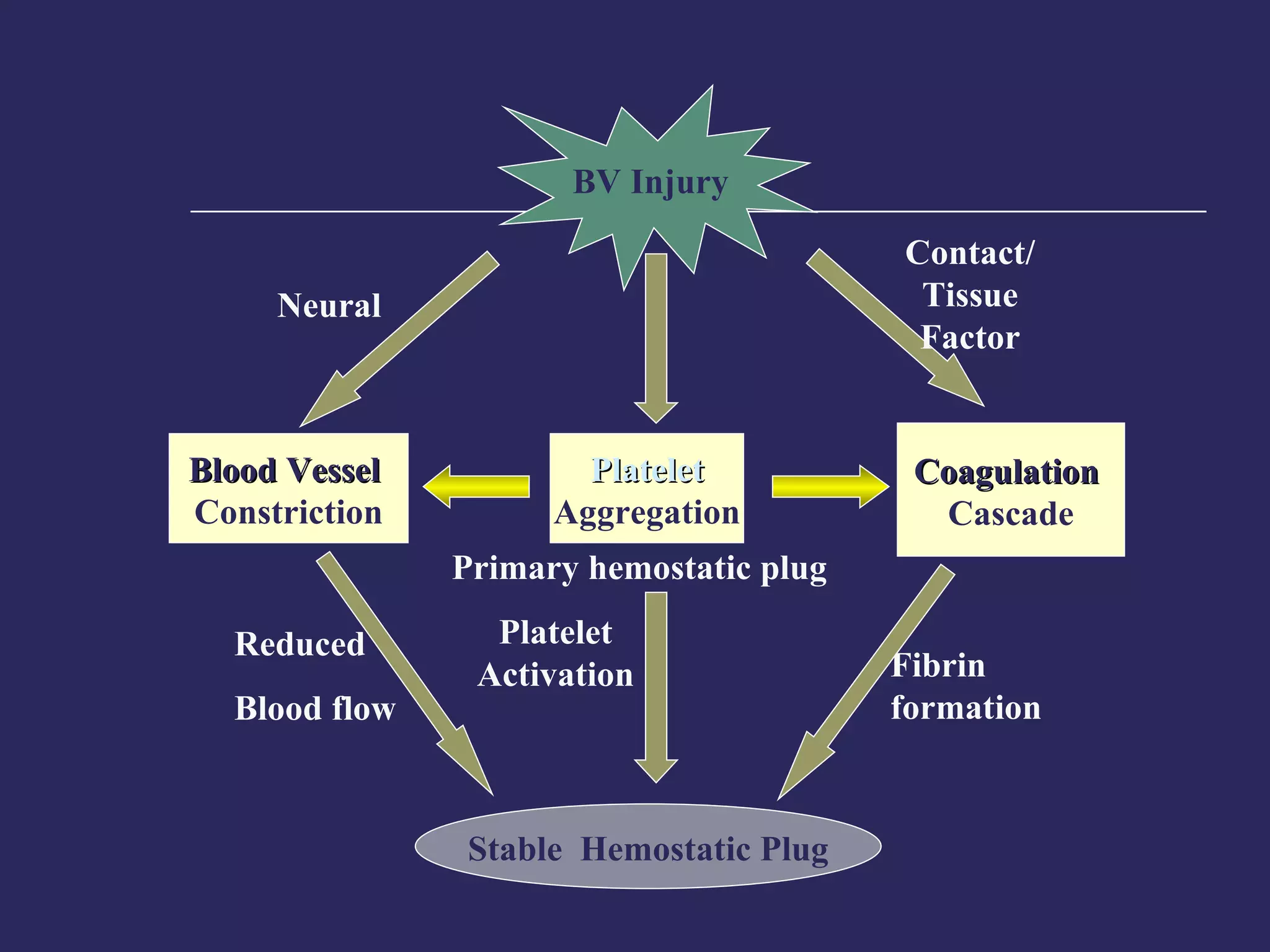
The document discusses various bleeding disorders including their causes, presentations, and treatments. It covers platelet disorders, coagulation factor deficiencies, von Willebrand disease, hemophilia A and B, disseminated intravascular coagulation (DIC), and liver disease. Treatment options discussed include cryoprecipitate, factor concentrates, DDAVP, vitamin K, fresh frozen plasma, and recombinant factor VIIa.