Sure! Here's a long and detailed explanation of the Digestive System in simple English. It’s great for study, presentations, or learning purposes.
---
Digestive System – Full Explanation
What is the Digestive System?
The digestive system is a group of organs that work together to break down food, absorb nutrients, and remove waste from the body.
It helps our body to use the food we eat by turning it into energy and building materials.
---
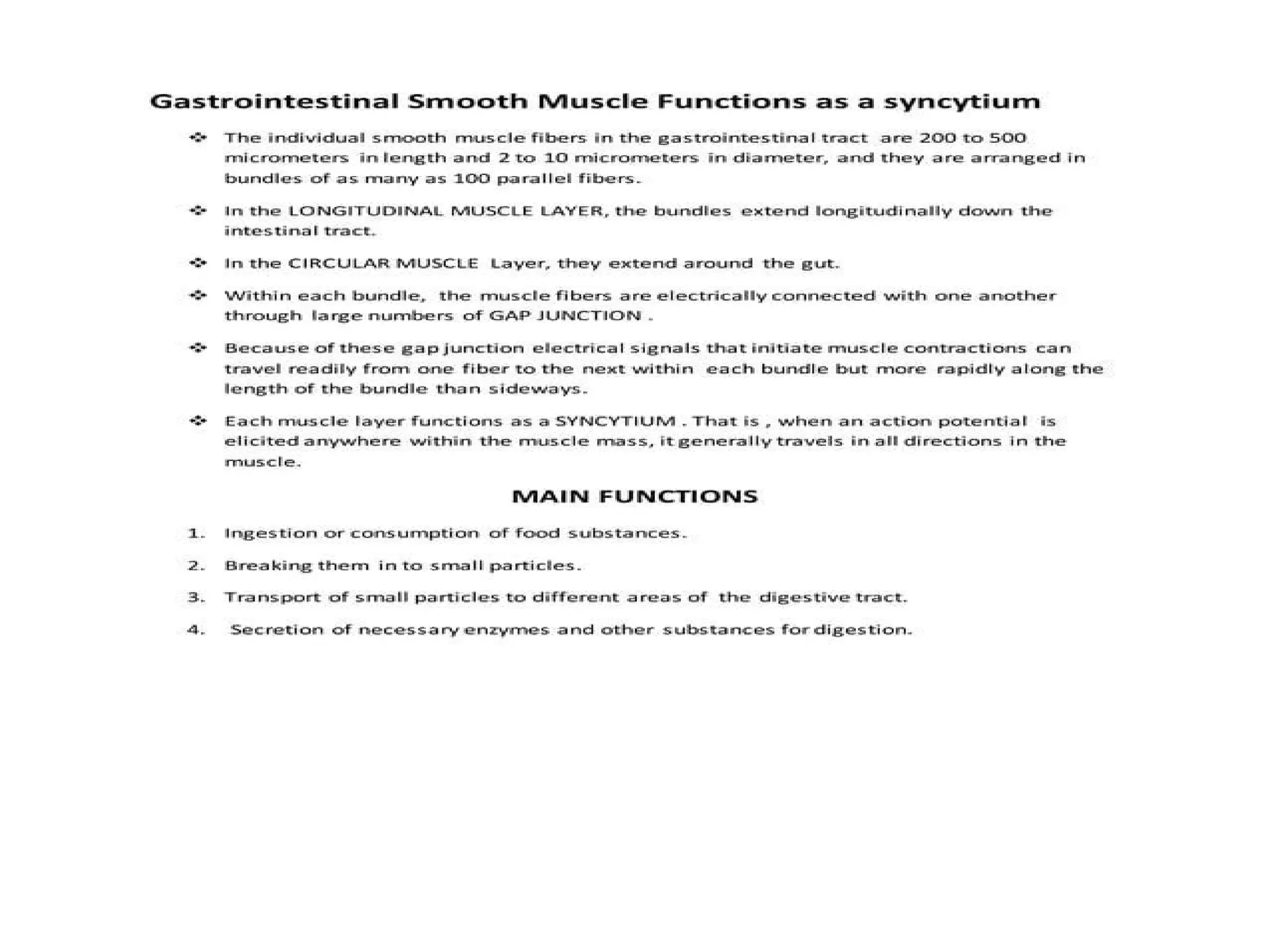
Main Functions of the Digestive System:
1. Ingestion – Taking in food through the mouth.
2. Digestion – Breaking food into smaller pieces (mechanically and chemically).
3. Absorption – Taking nutrients from food into the blood.
4. Excretion – Removing undigested waste from the body.
---
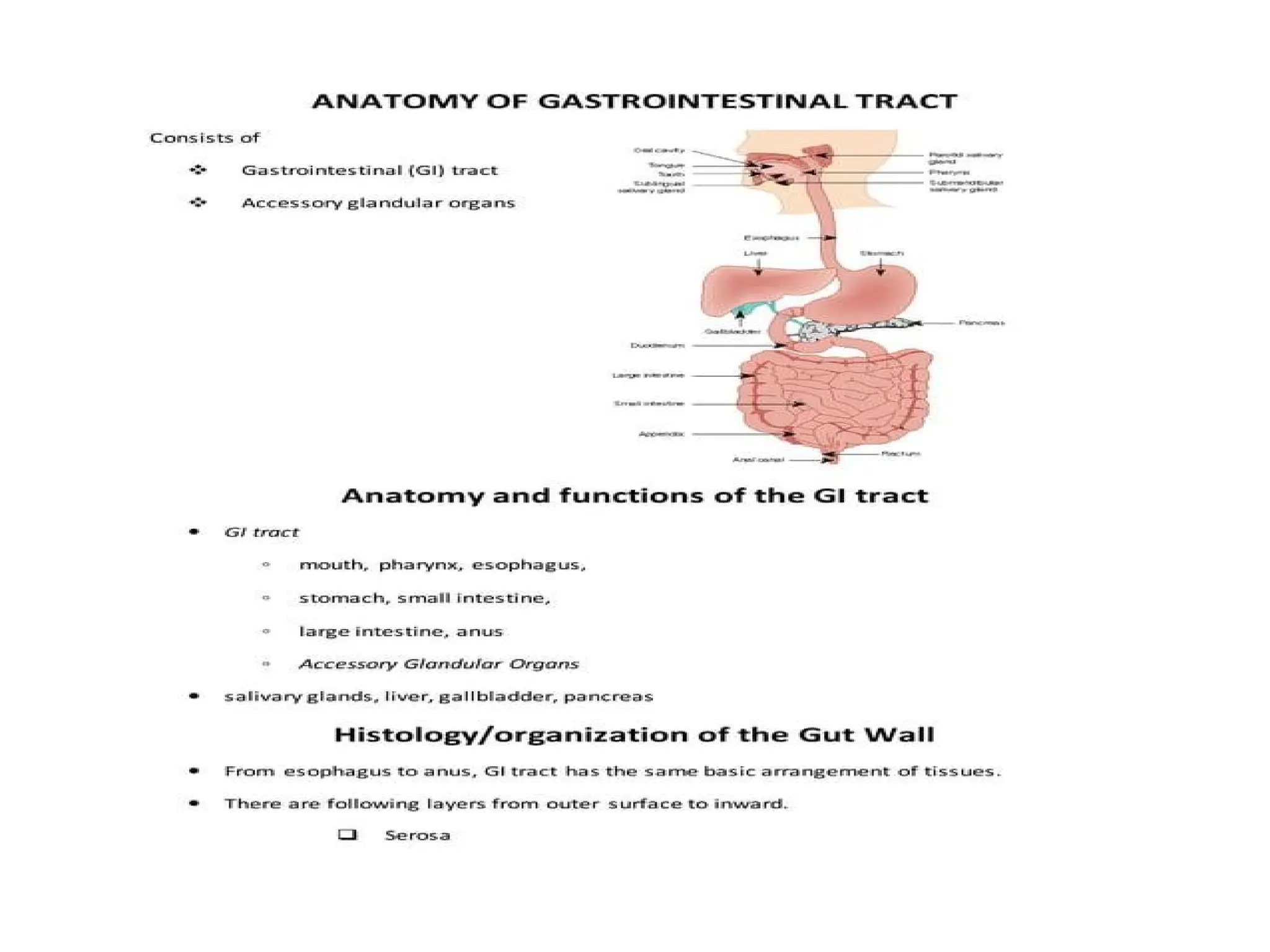
Major Organs of the Digestive System (in order):
1. Mouth
Digestion starts here.
Teeth chew food (mechanical digestion).
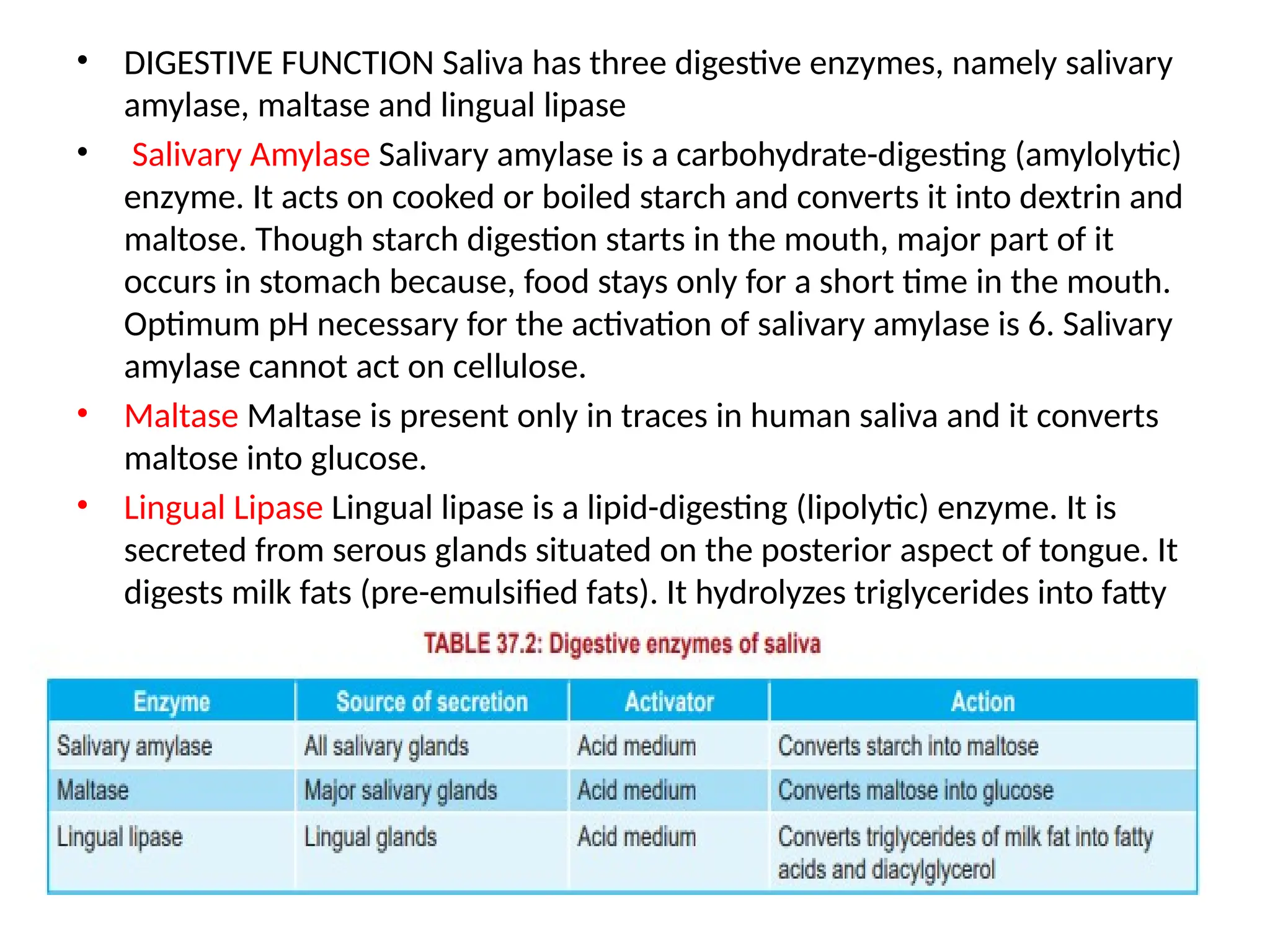
Saliva breaks down starch (chemical digestion).
2. Esophagus
A muscular tube that connects the mouth to the stomach.
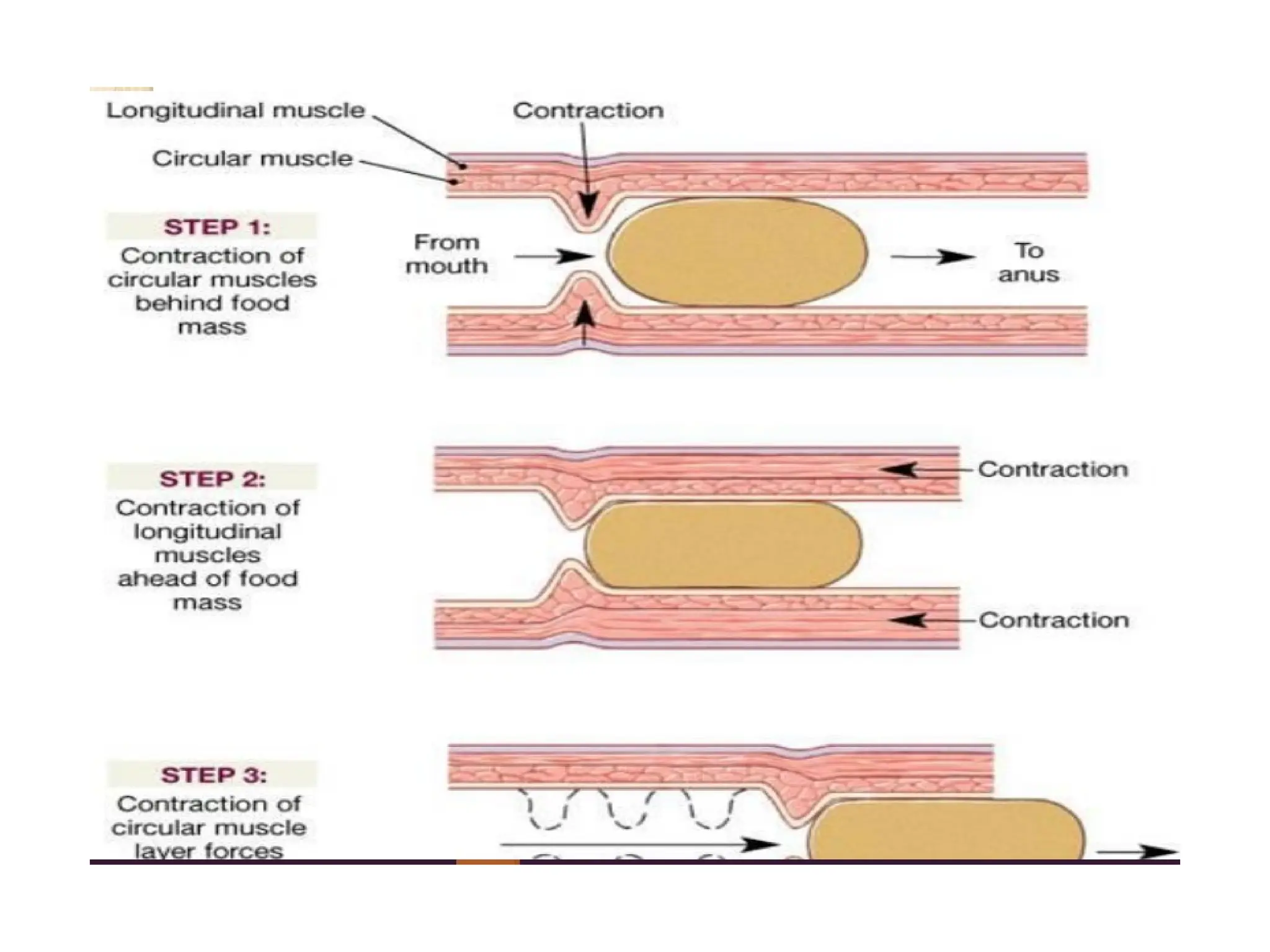
Food is pushed down by a movement called peristalsis.
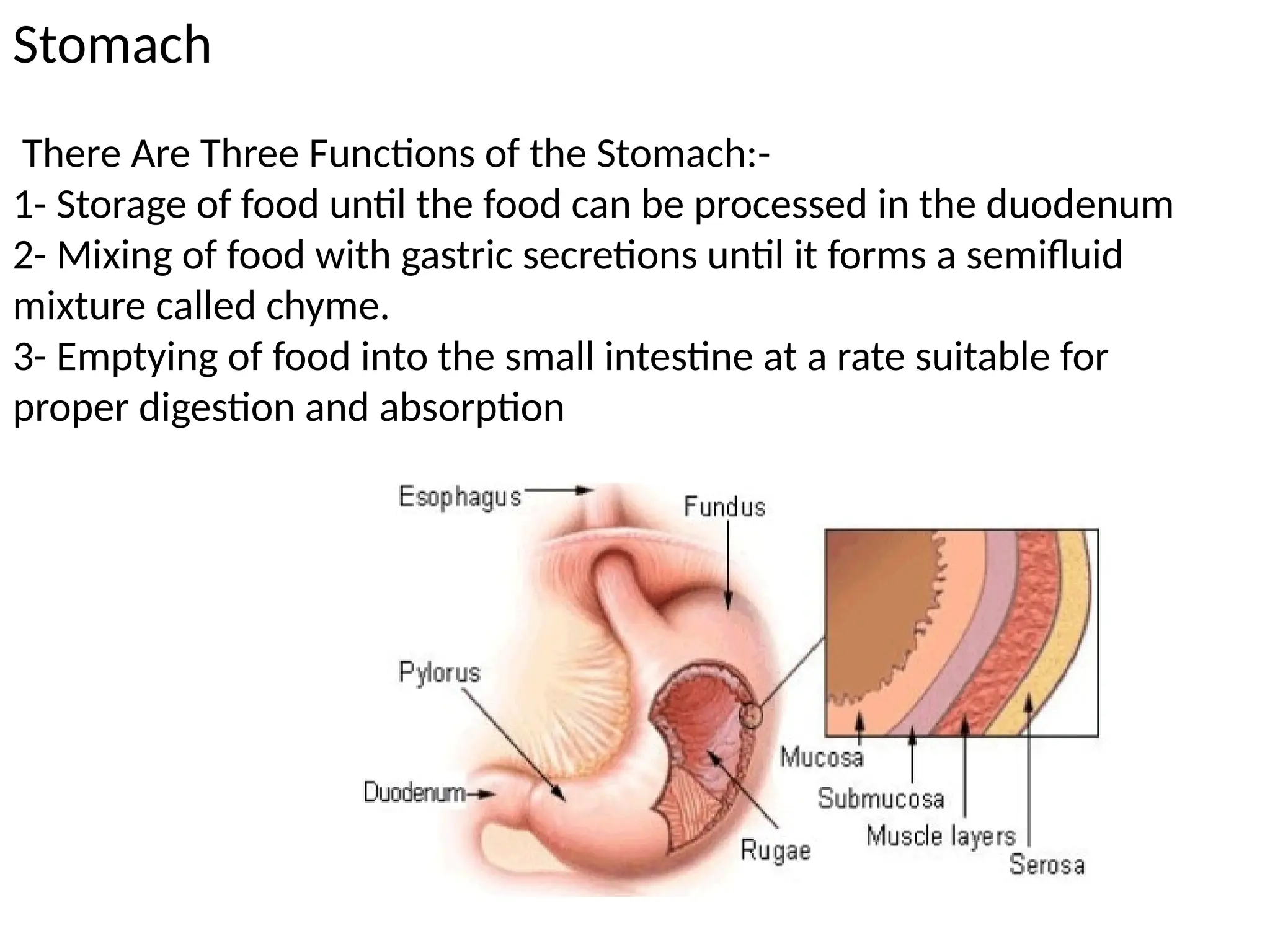
3. Stomach
A muscular organ that churns food.
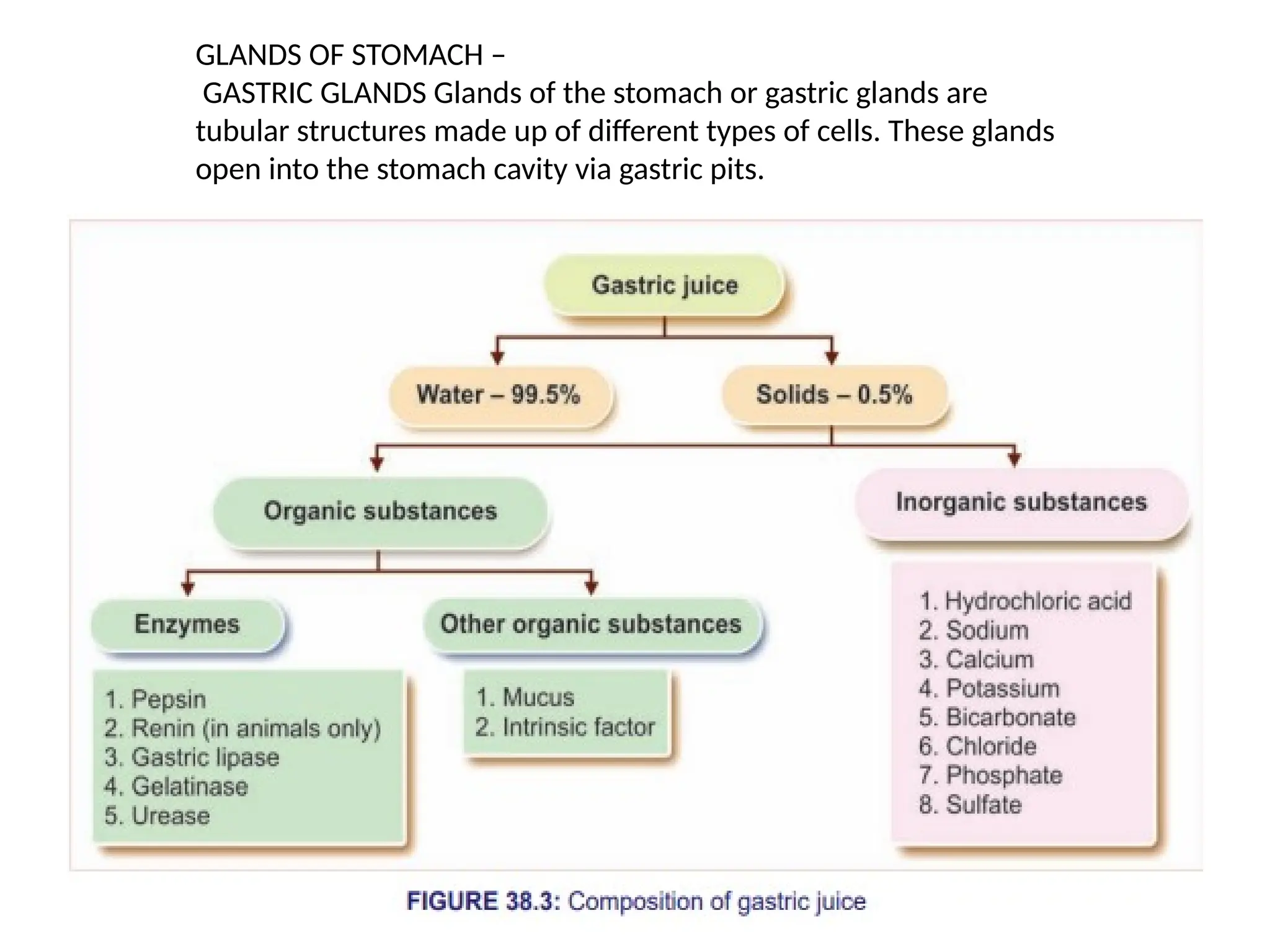
Releases gastric juice (contains acid and enzymes).
Breaks down proteins.
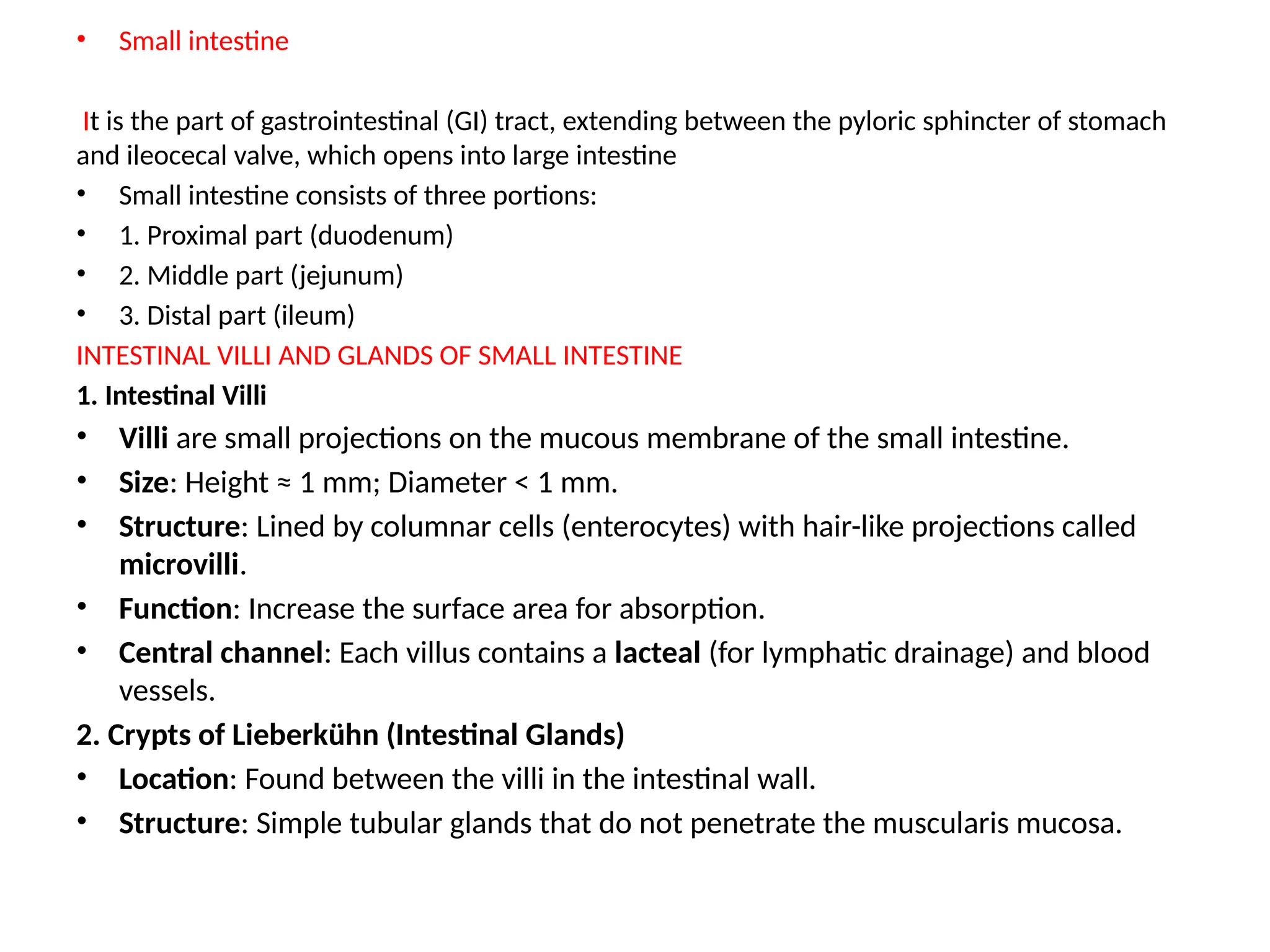
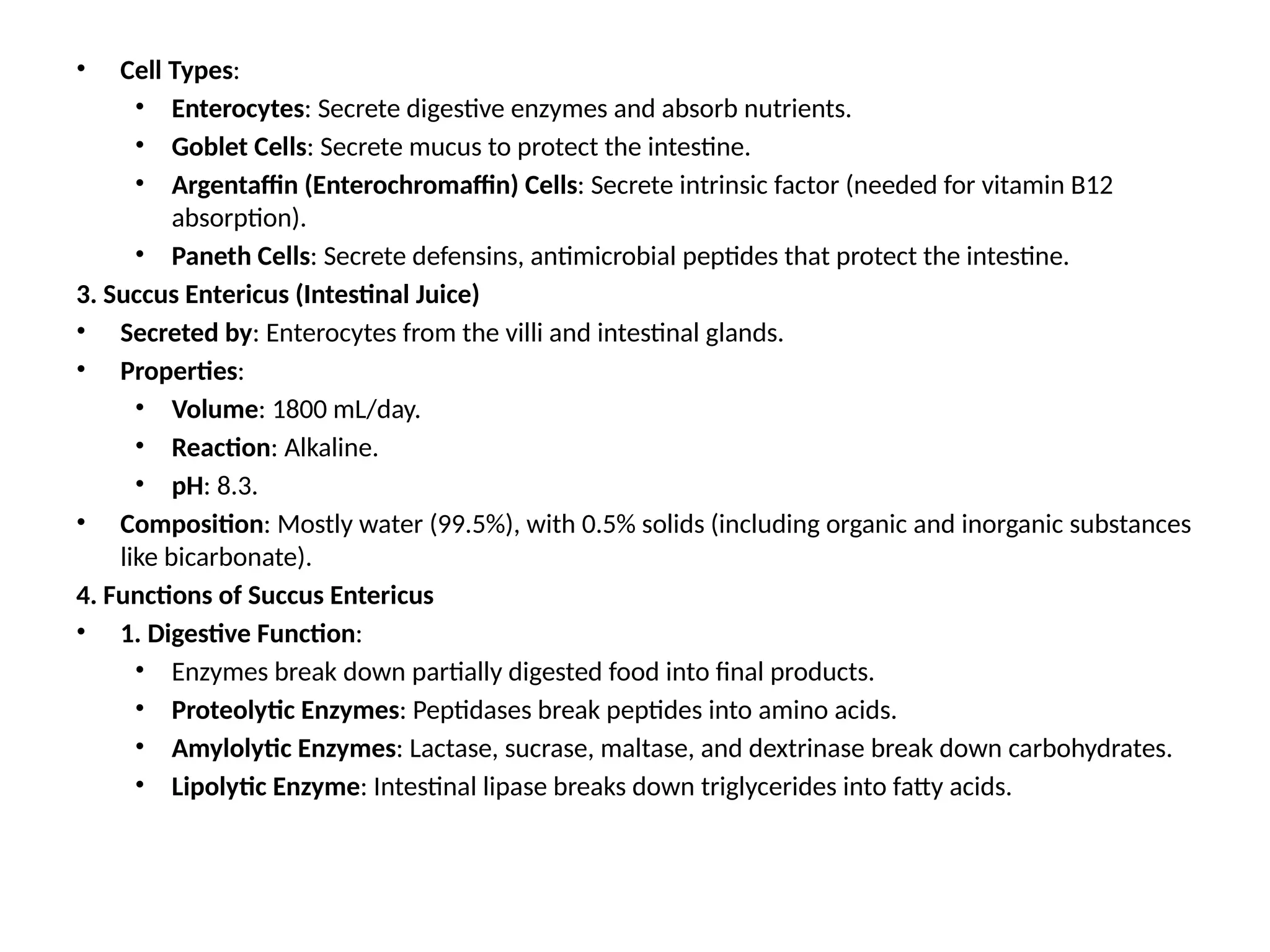
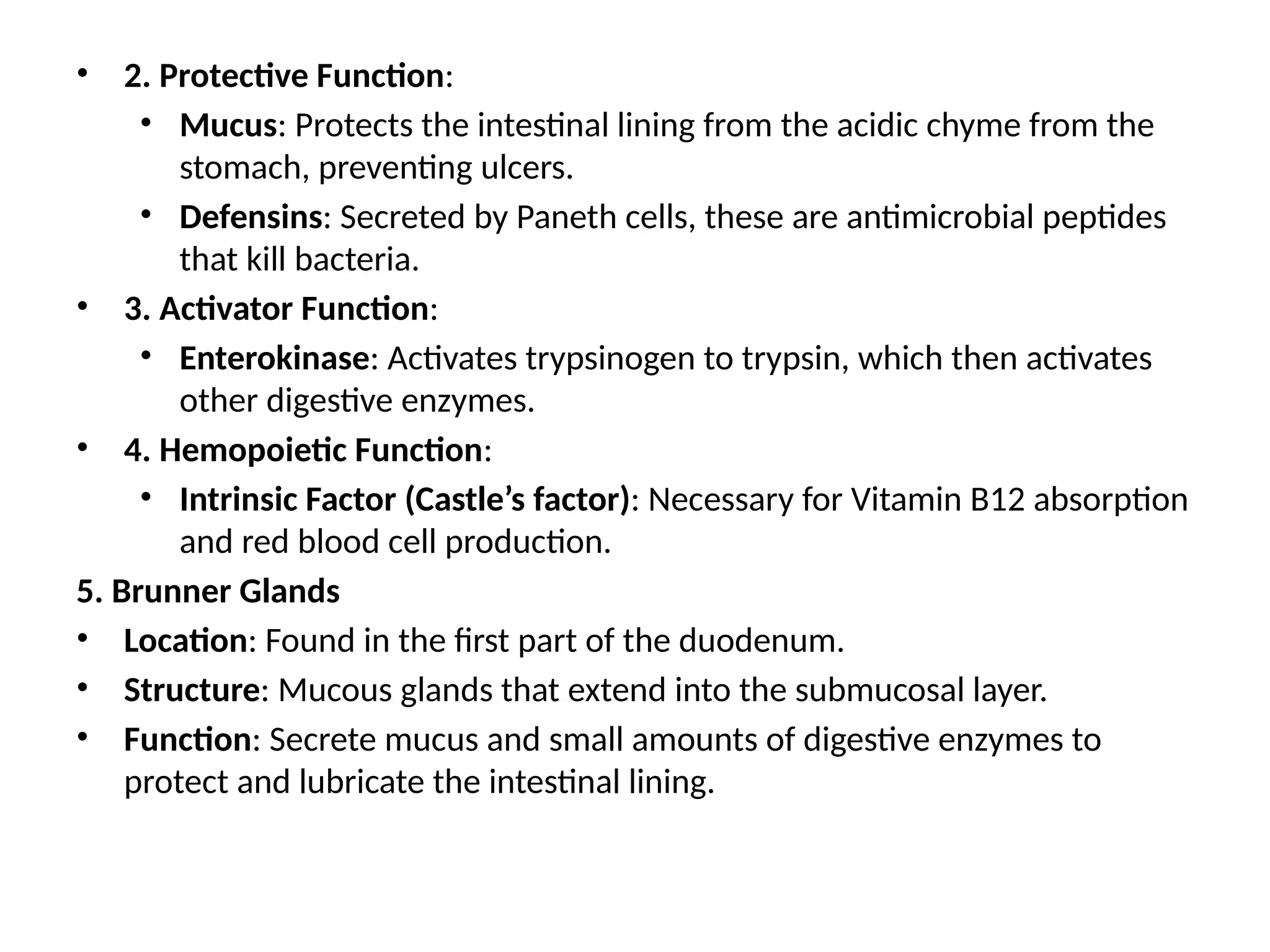
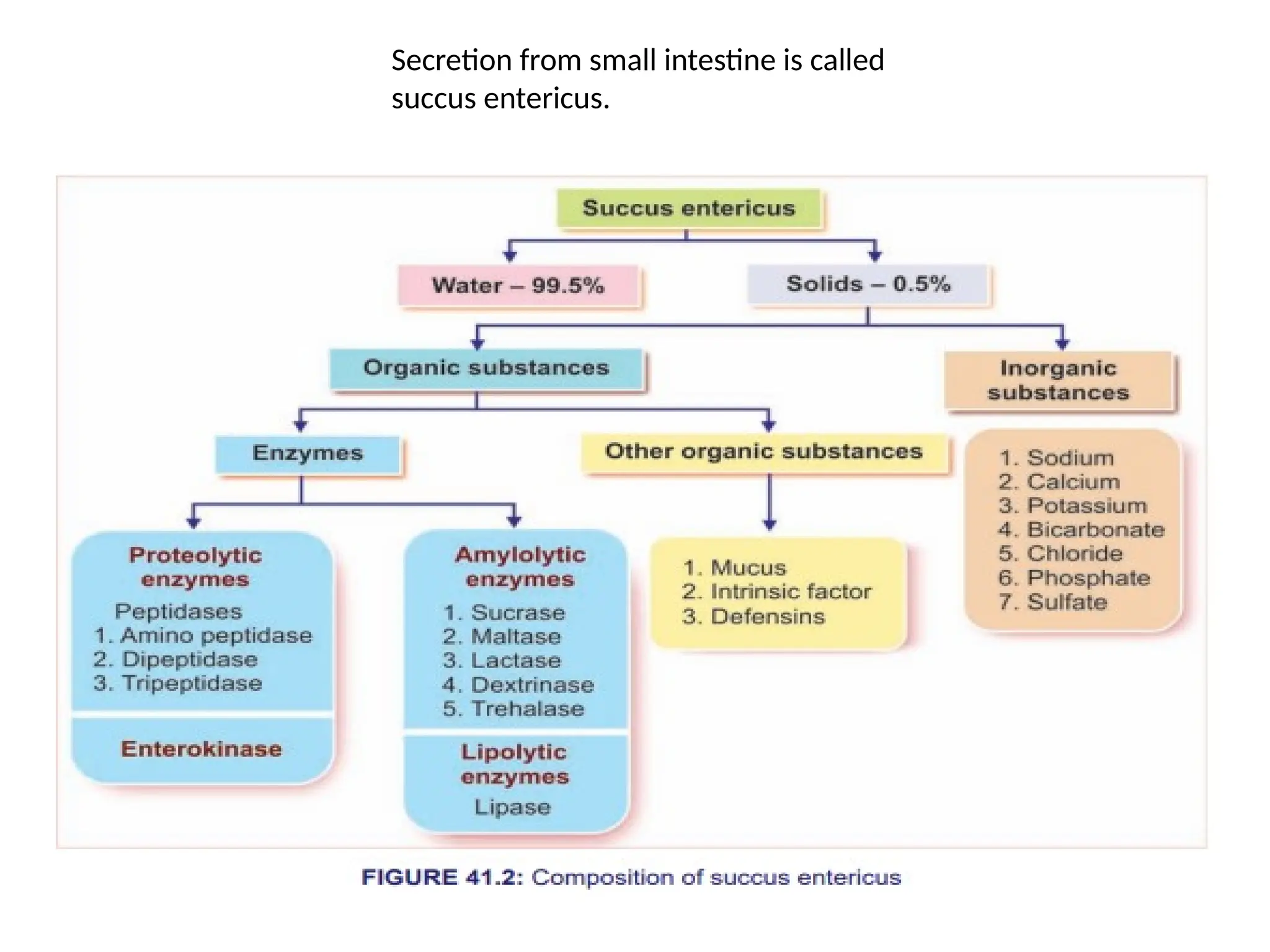
4. Small Intestine
The most important part of digestion and absorption.
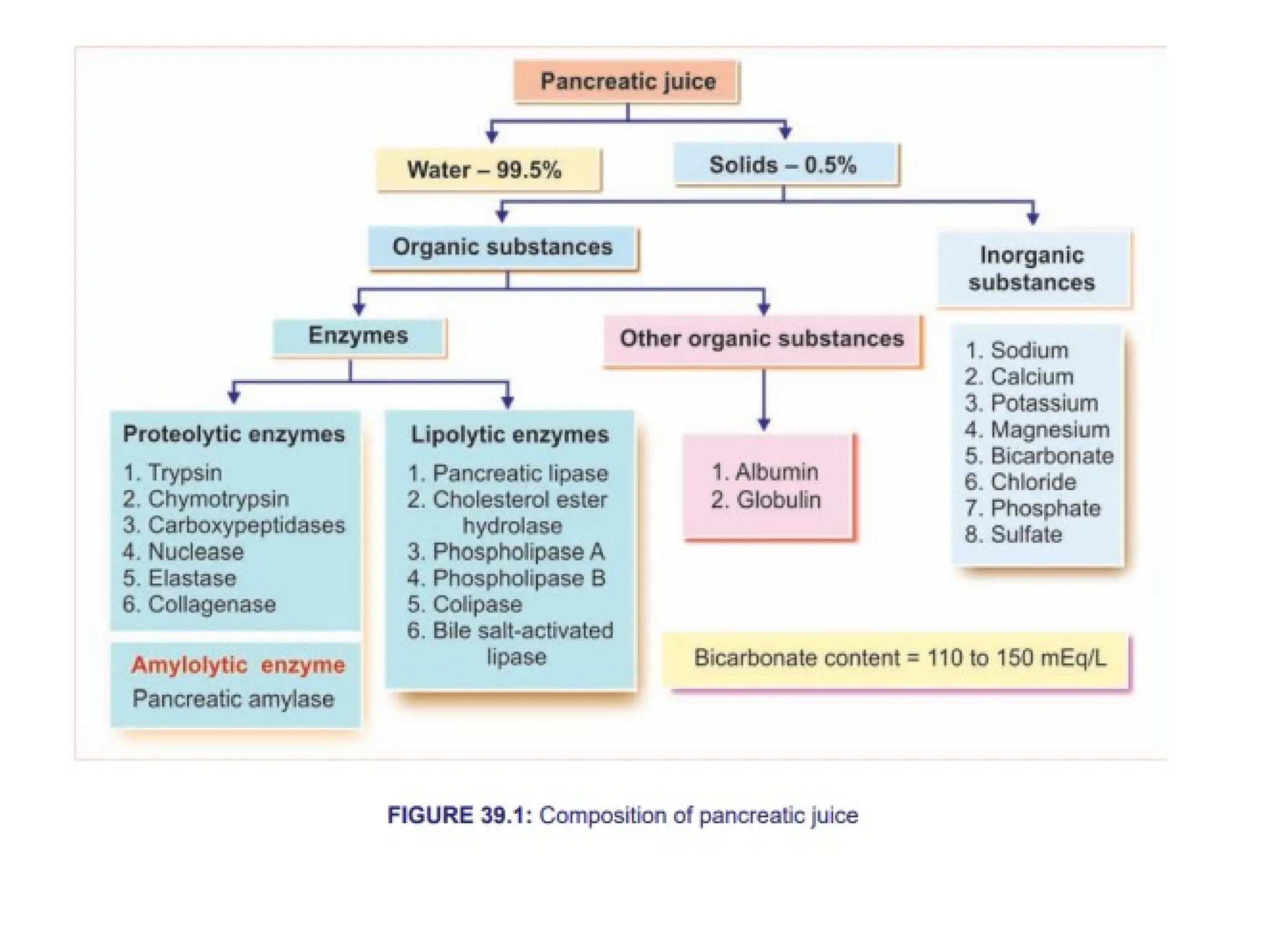
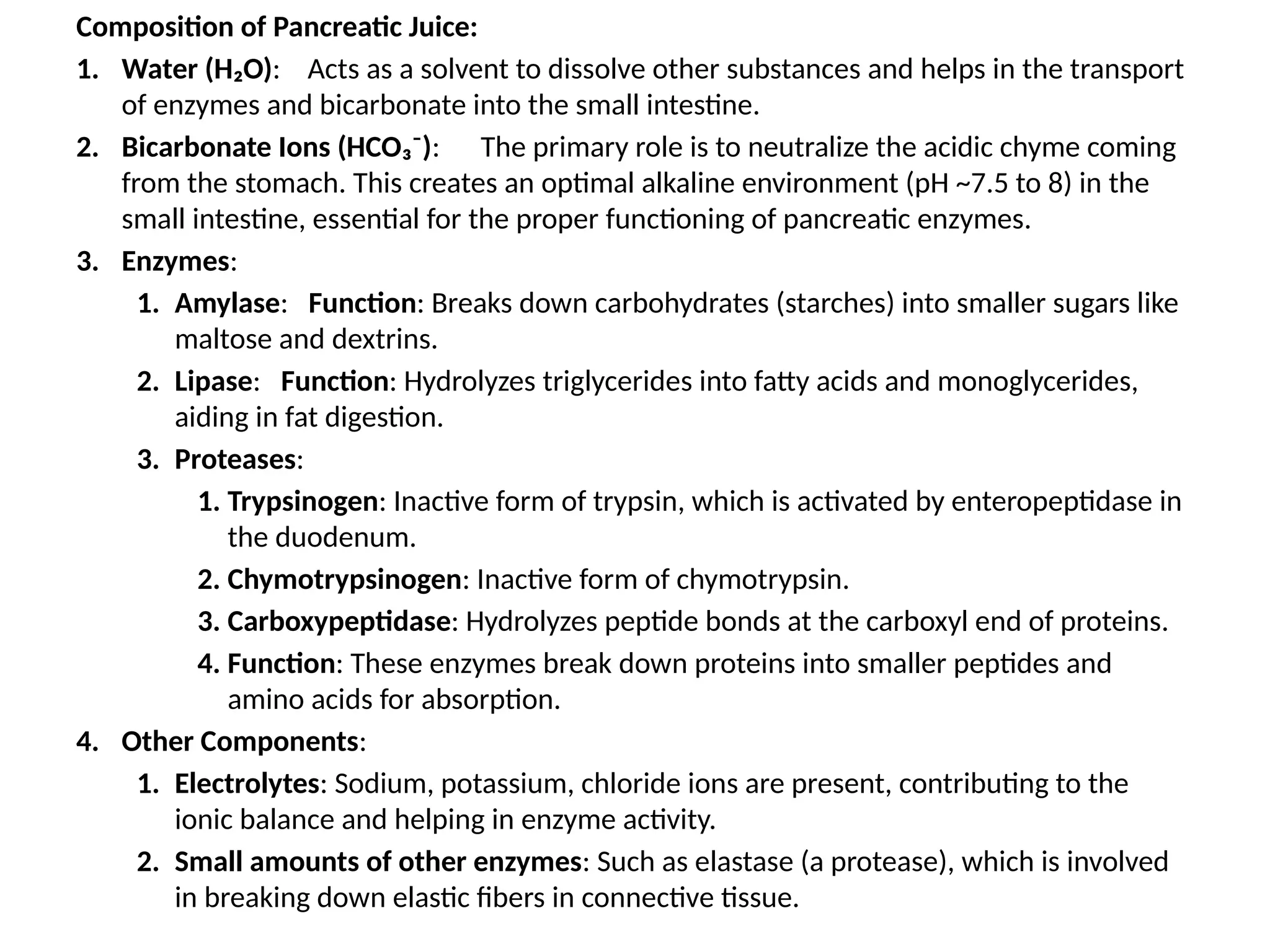
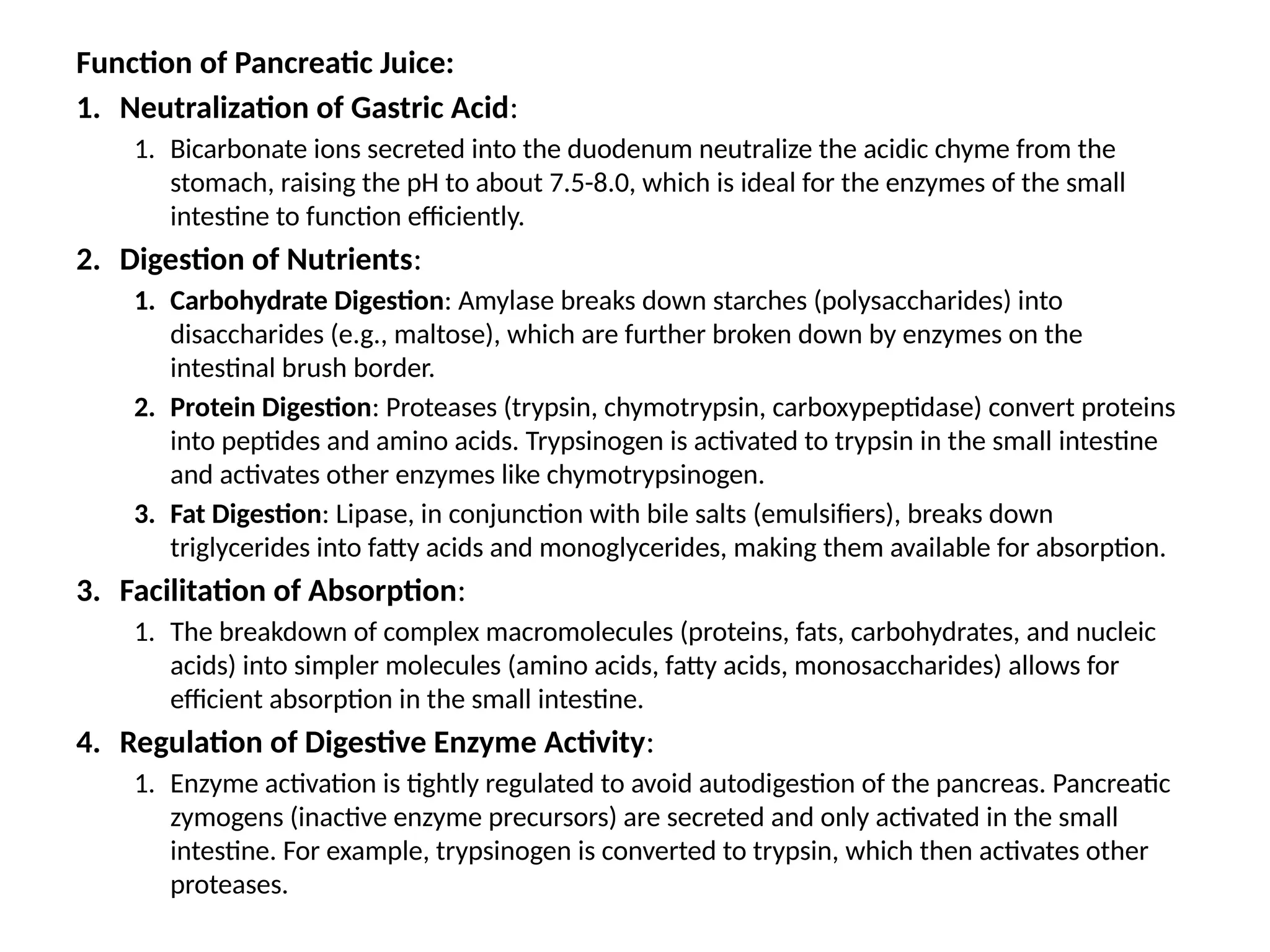
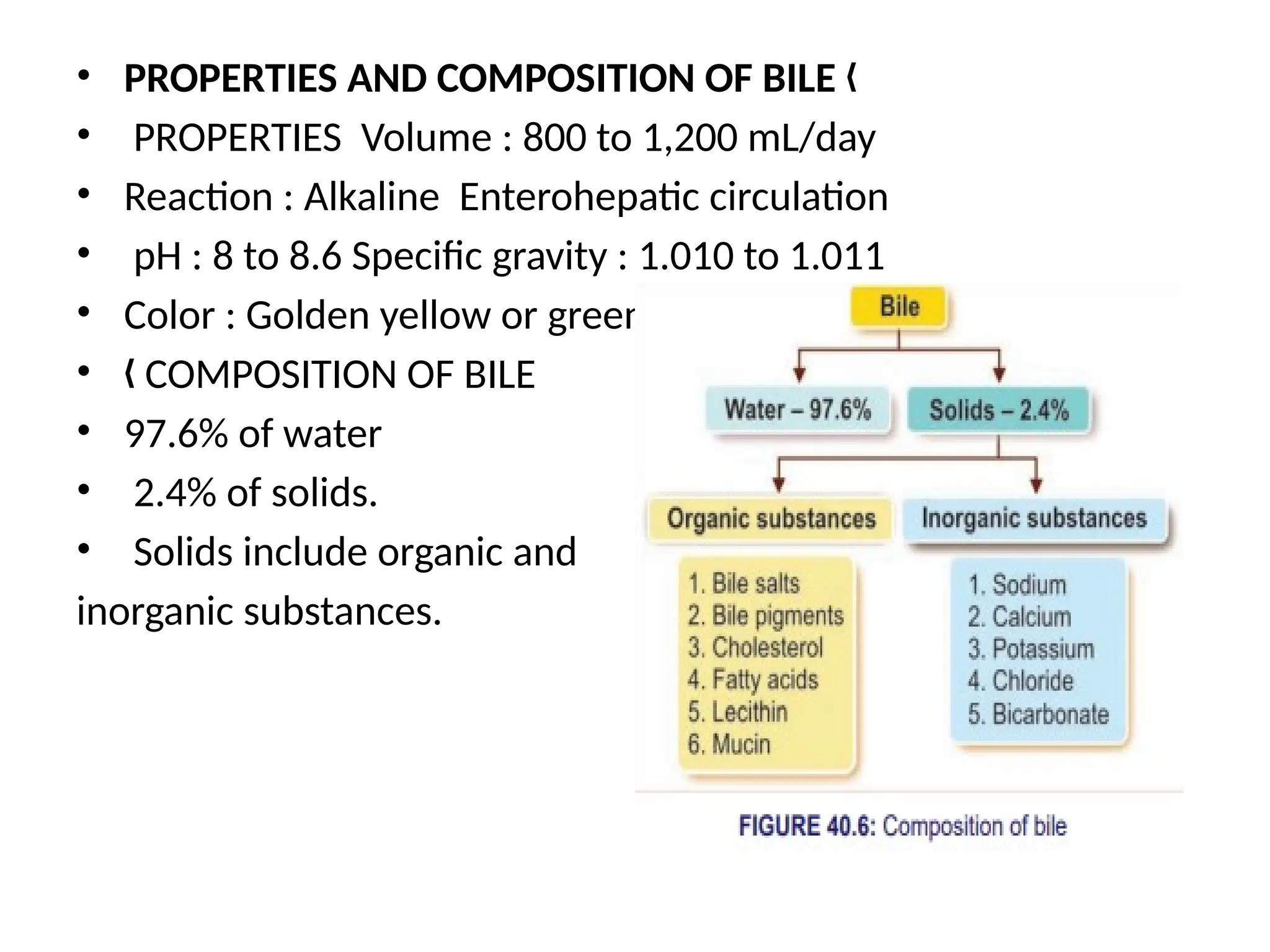
Bile (from liver) and pancreatic juice (from pancreas) help in digestion.
Villi (tiny finger-like projections) absorb nutrients into the blood.
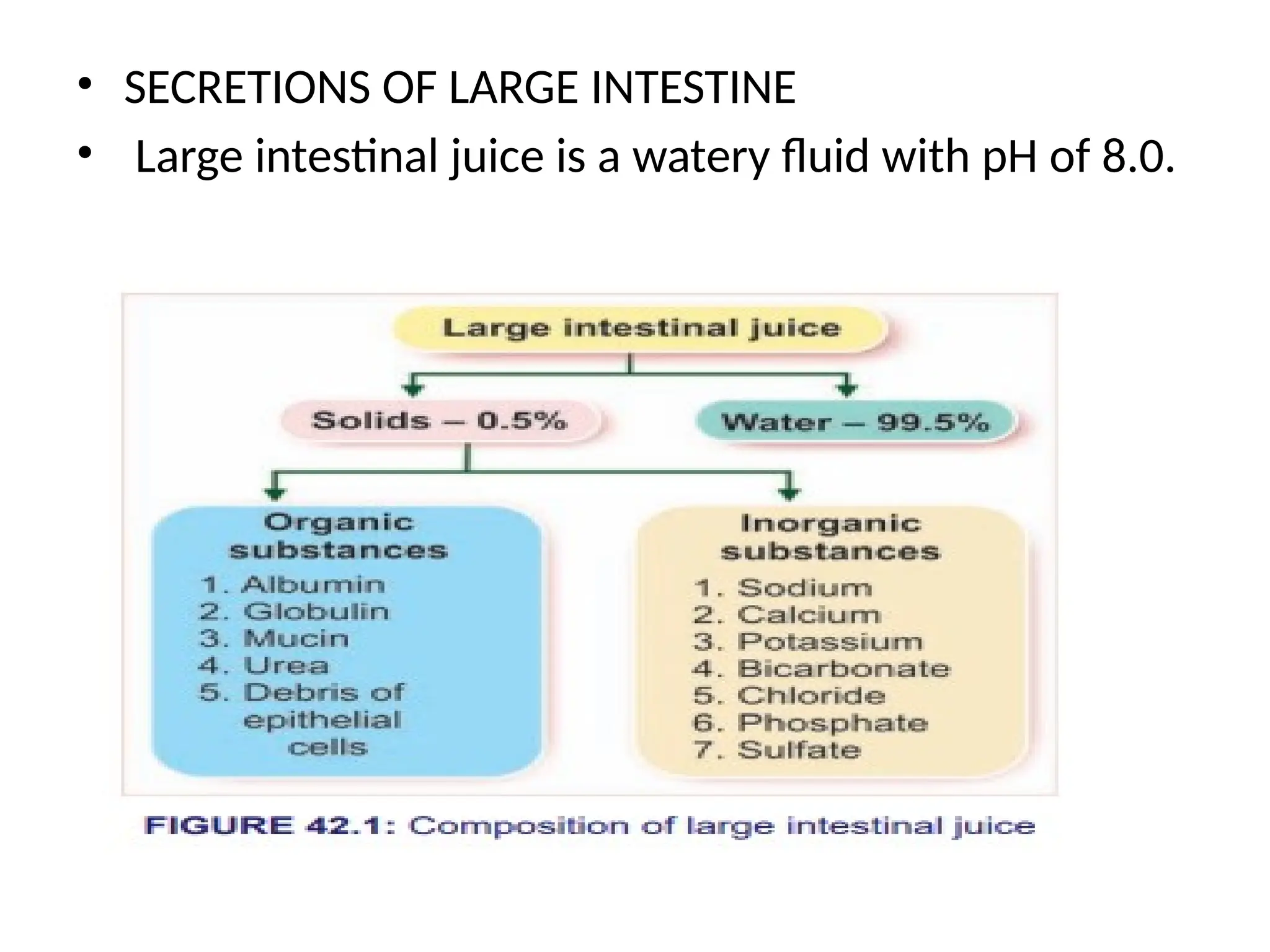
5. Large Intestine
Absorbs water and minerals from undigested food.
Prepares solid waste (feces).
6. Rectum and Anus
Stores waste until it is excreted from the body through the anus.
---
Helper Organs (Accessory Organs):
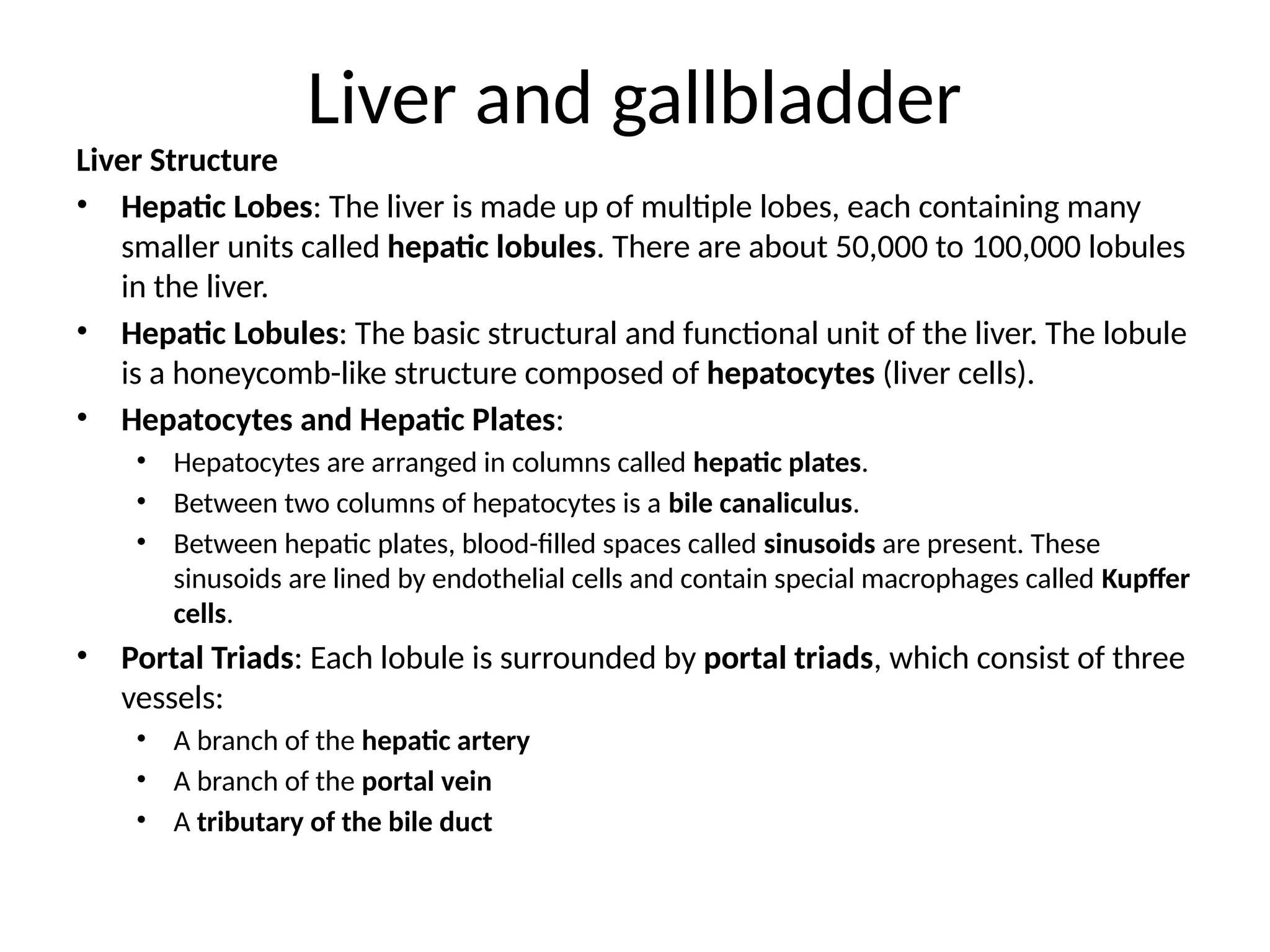
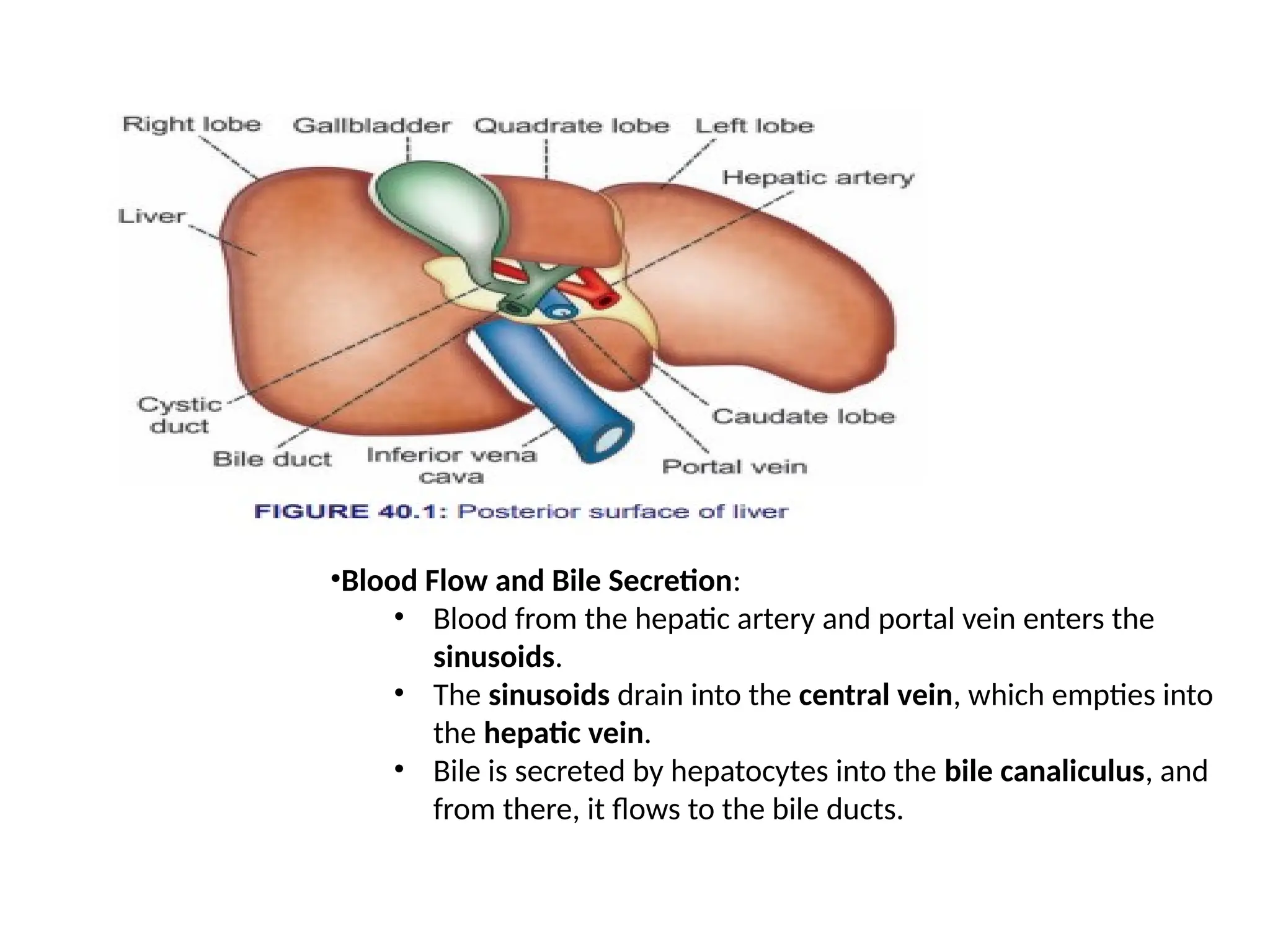
1. Liver
Produces bile to break down fats.
Stores nutrients and detoxifies harmful substances.
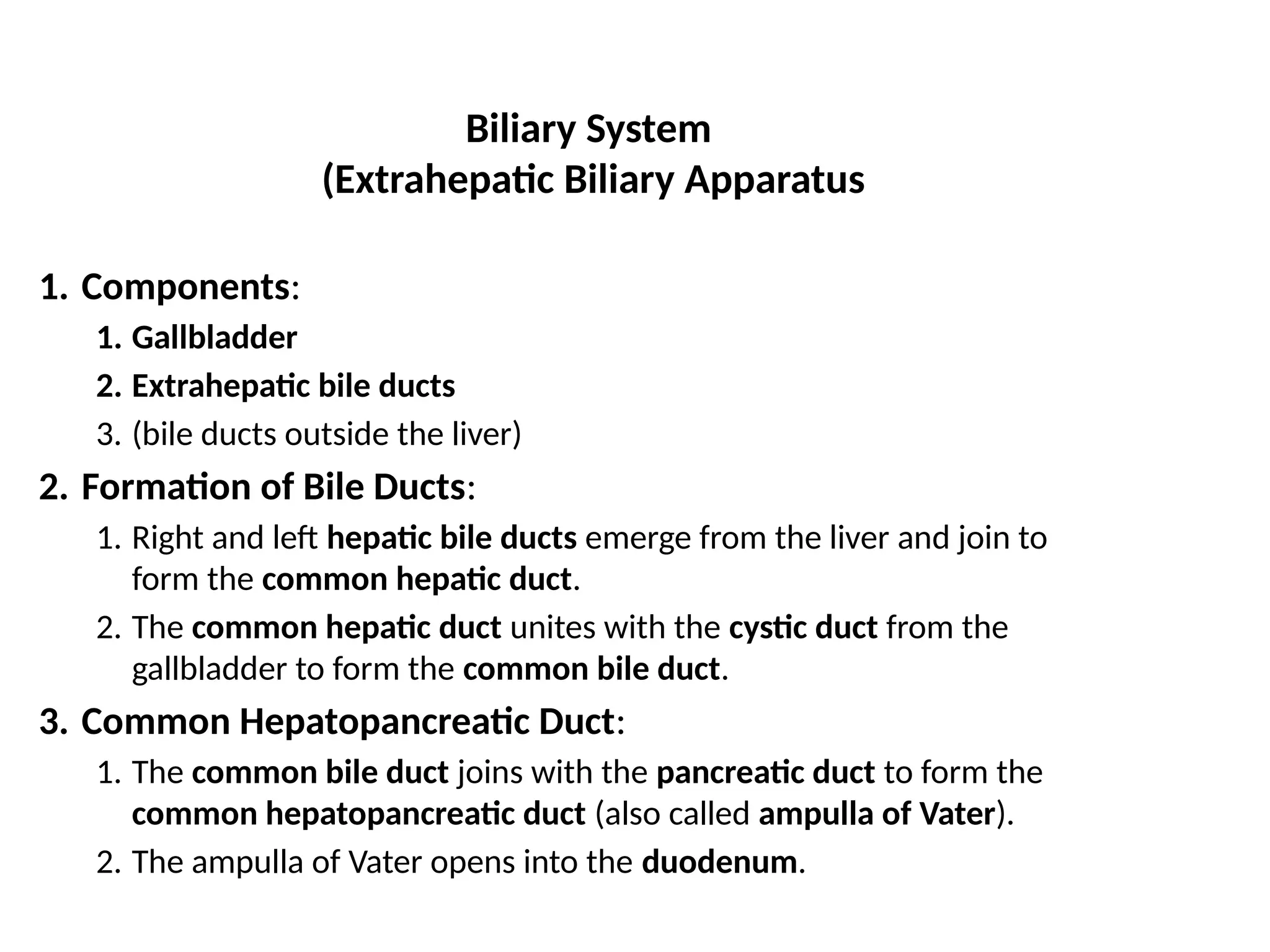
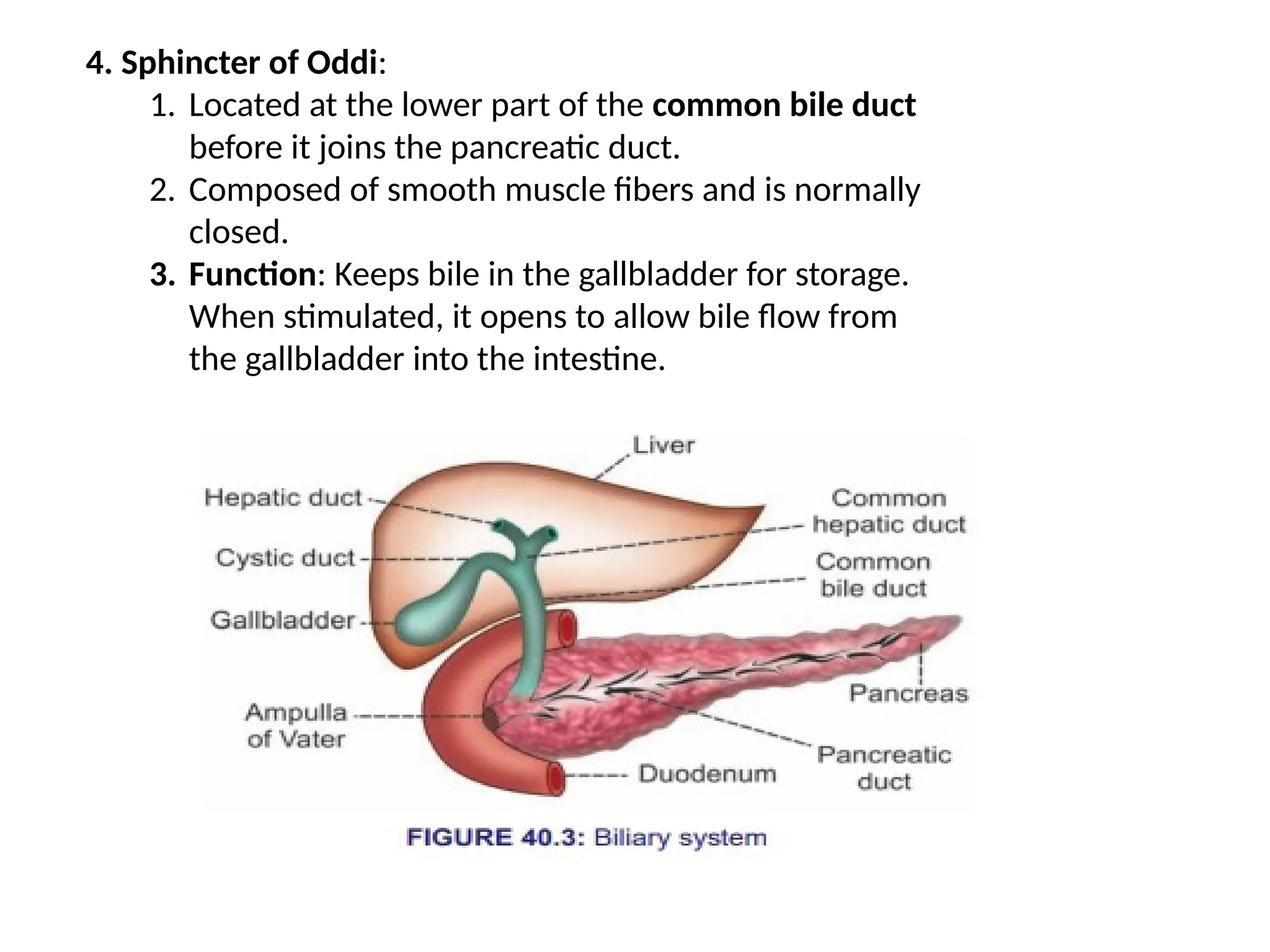
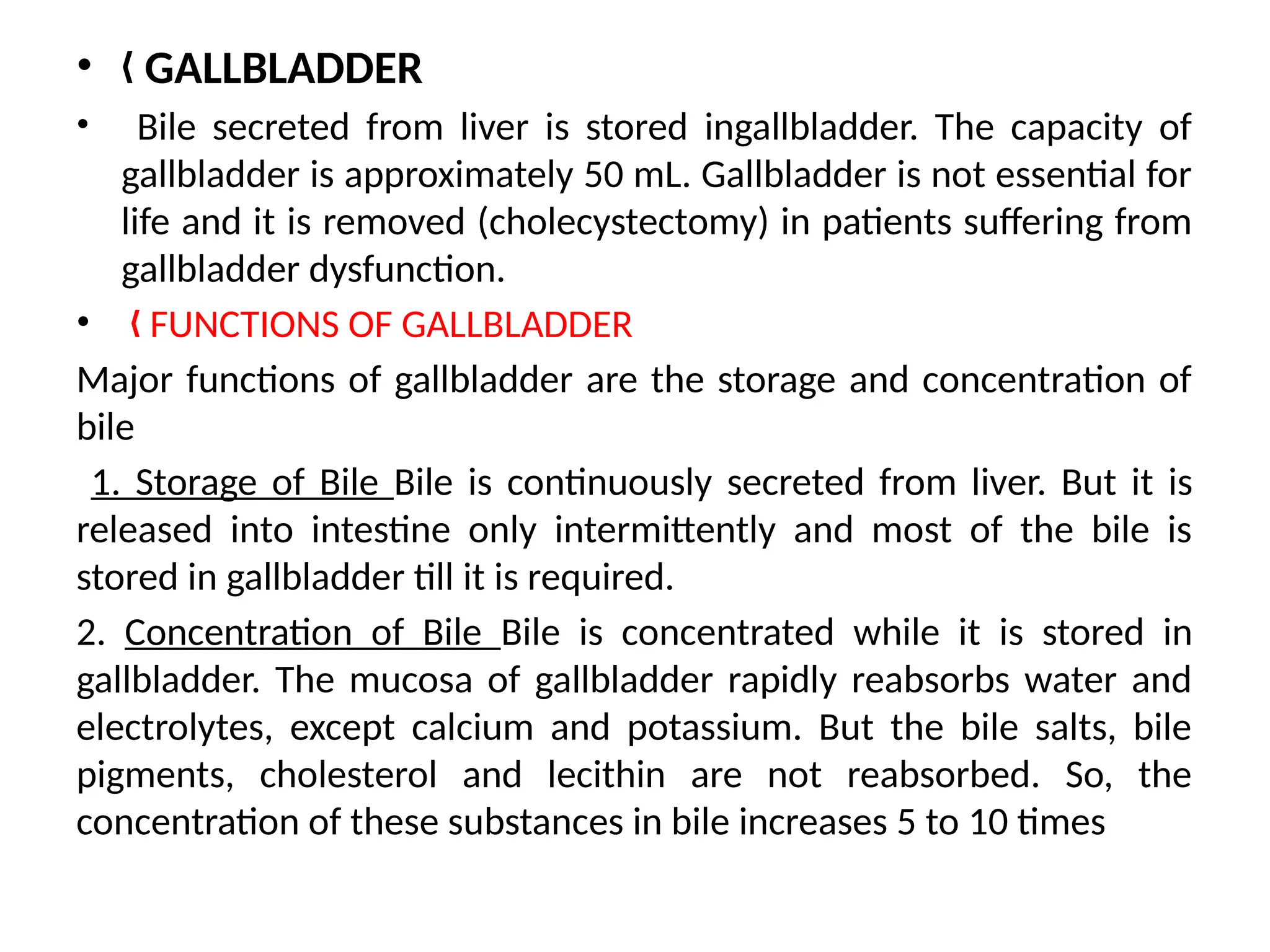
2. Gallbladder
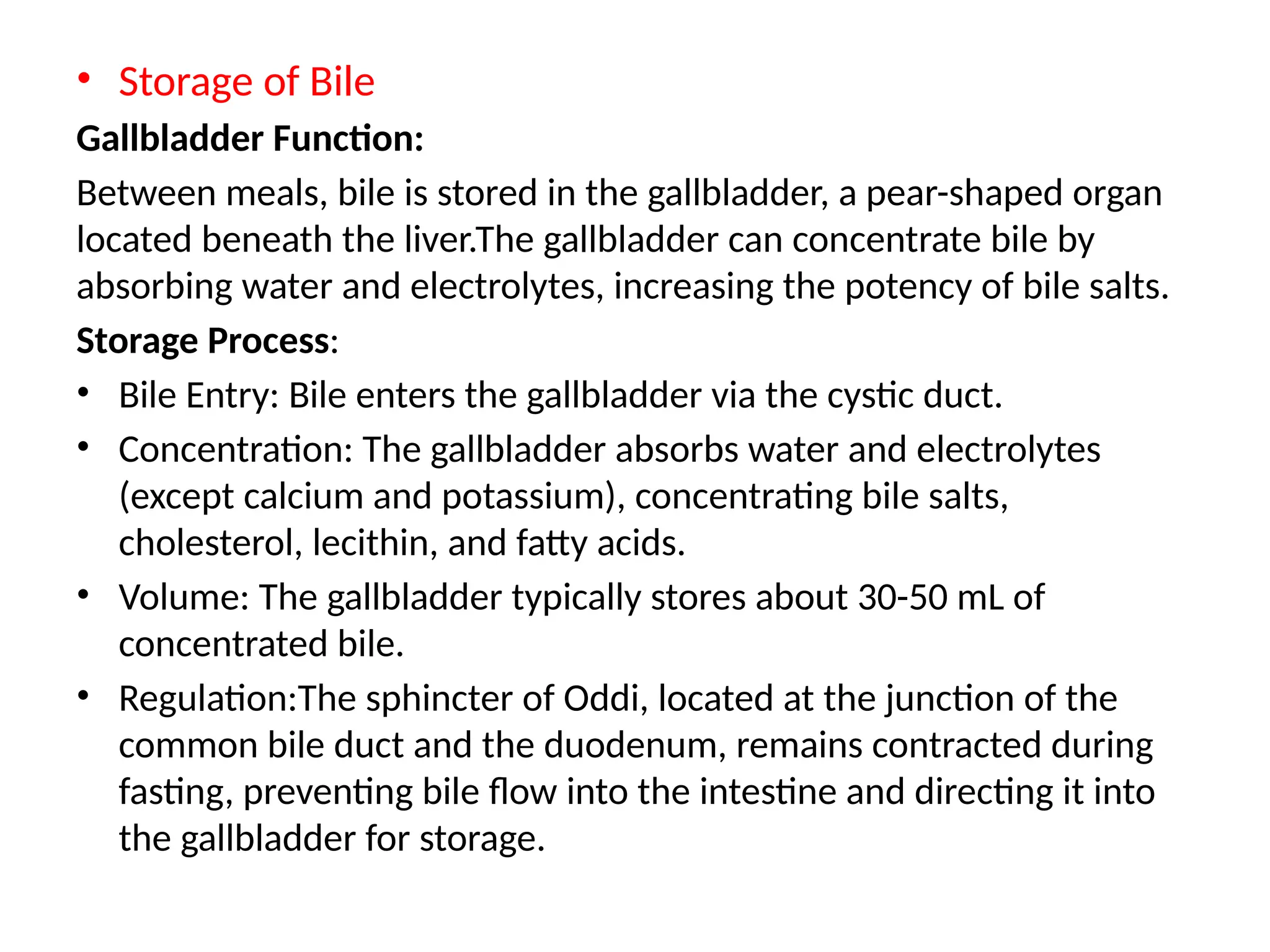
Stores and releases bile into the small intestine.
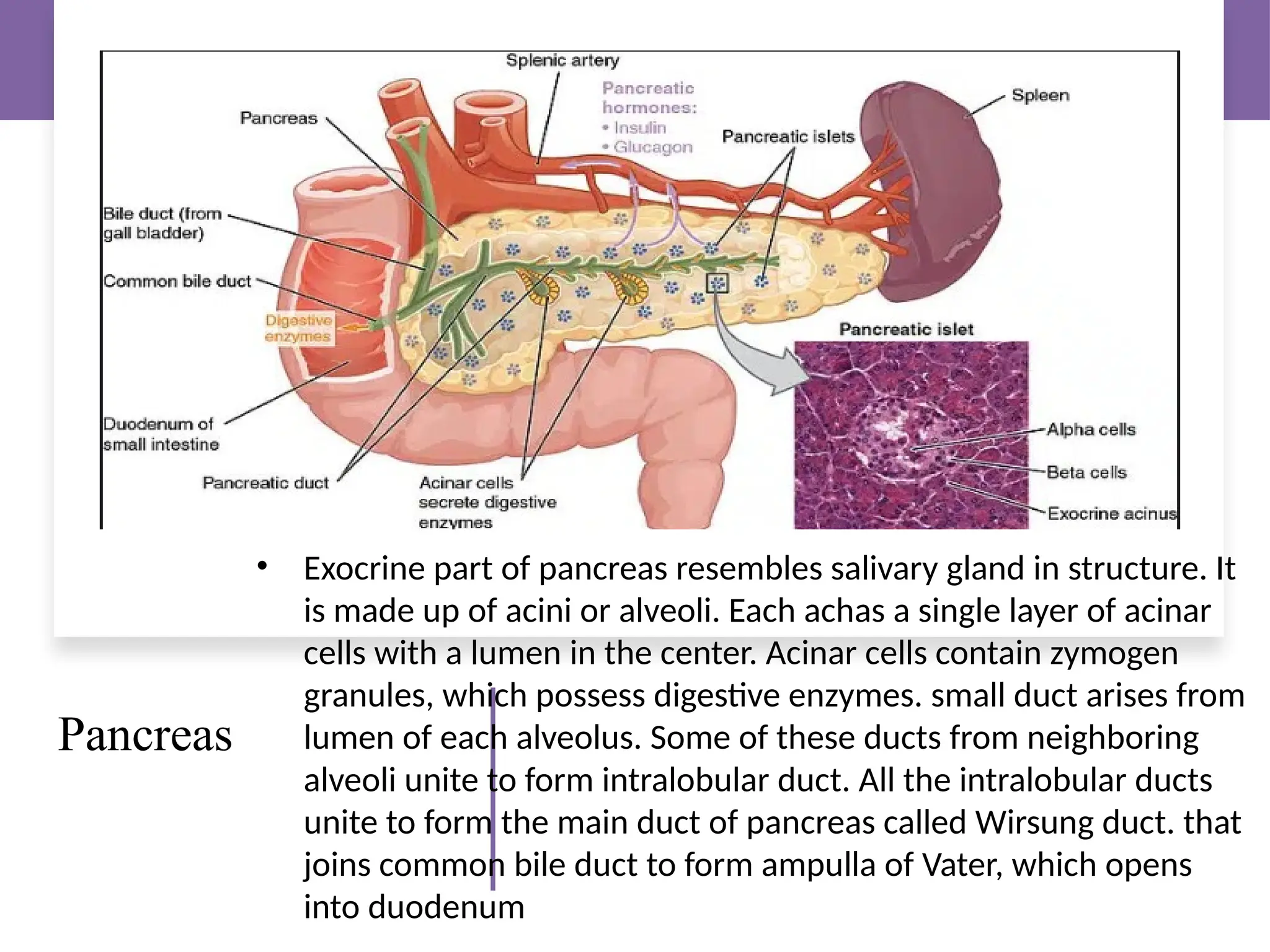
3. Pancreas
Produces enzymes for digesting proteins, fats, and carbohydrates.
Also helps in controlling blood sugar (produces insulin).
---
Types of Digestion:
1. Mechanical Digestion:
Physical breakdown of food (chewing, stomach churning)
2. Chemical Digestion:
Enzymes and acids break down food molecules
---
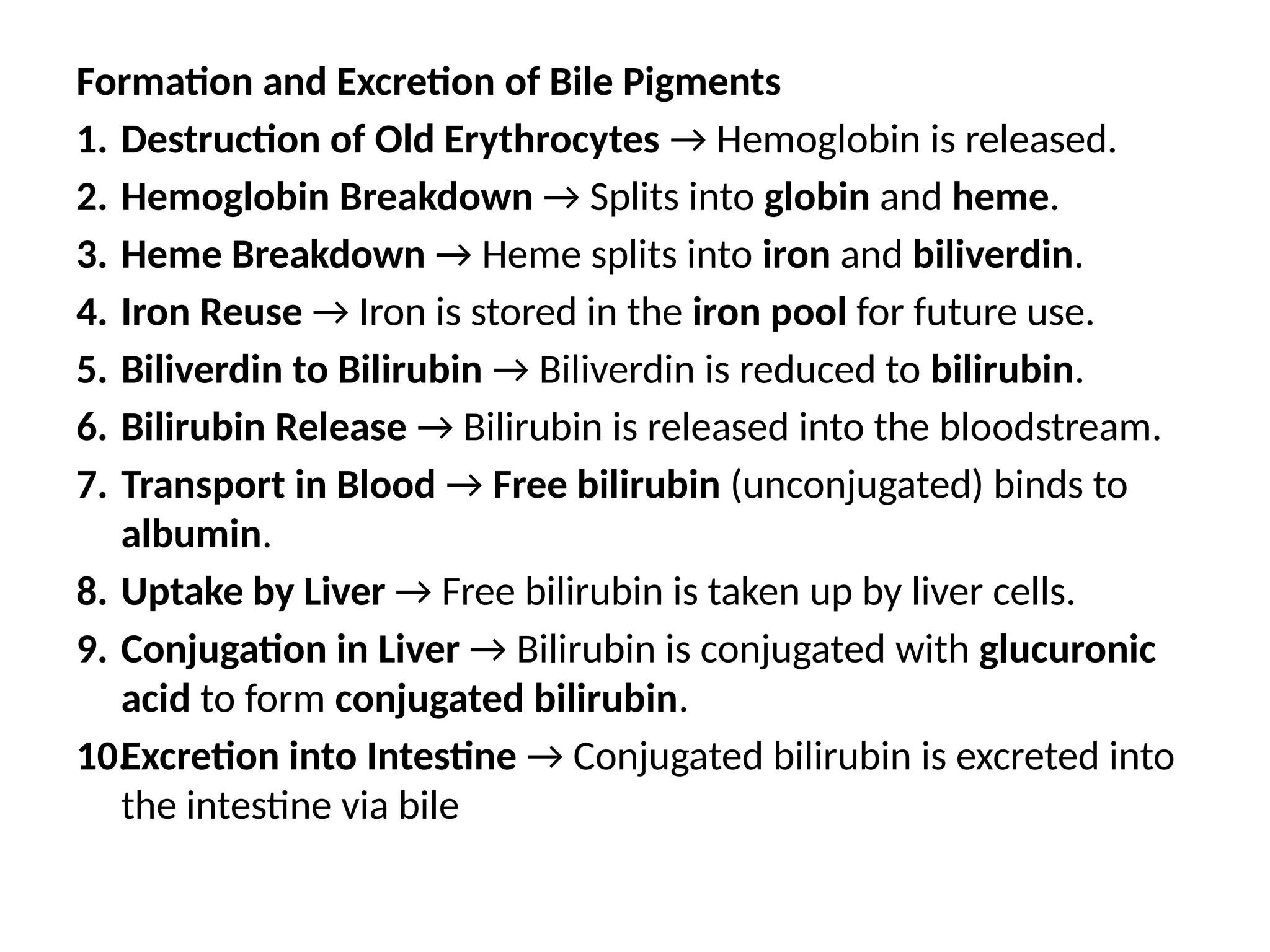
What Happens to Food? (Step-by-step)
---
Common Digestive Problems:
Constipation – Trouble passing stool
Diarrhea – Loose, watery stool
Indigestion – Discomfort or pain in the stomach
Ulcers – Sores in the stomach lining
Acid reflux – Stomach acid moves up to the esophagus
---
How to Keep the Digestive System Healthy:
Eat fiber-rich foods (fruits, vegetables, whole grains)
Drink enough water
Exercise regularly
Avoid too much junk food and soft drinks
Eat slowly and chew well
---
Conclusion:
The digestive system is essential for life. It allows our body to use the food we eat by breaking it into nutrients and removing the waste. A healthy digestive system means a healthy body!
---
Would you like me to create a PowerPoint slide of this topic too?