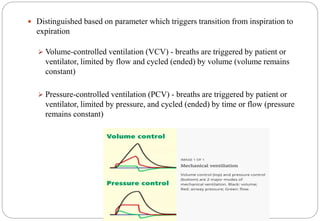
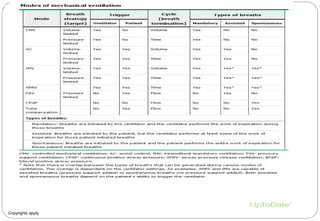
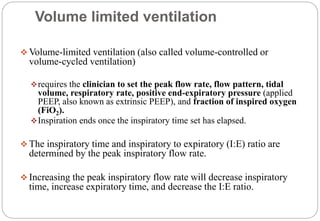
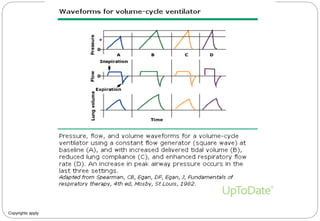
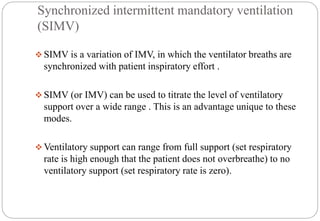
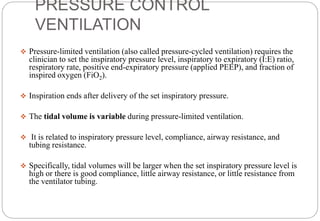
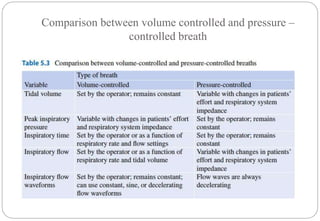
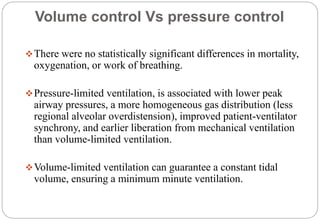
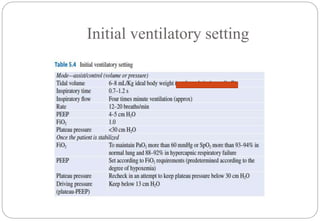
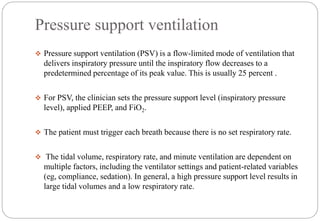
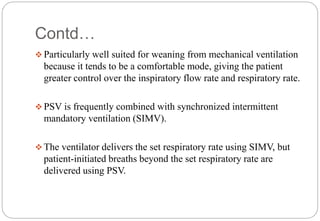
This document discusses different modes of mechanical ventilation. It begins by defining key terms like trigger, cycle, and limit. It then describes the four phases of a mechanical breath - trigger, limit, cycle, and expiration. The main modes discussed are volume-controlled ventilation, pressure-controlled ventilation, and pressure support ventilation. Volume-controlled ventilation delivers a set tidal volume, pressure-controlled ventilation delivers a set pressure level, and pressure support ventilation provides pressure assistance for patient-triggered breaths. Other modes like synchronized intermittent mandatory ventilation are also summarized briefly.
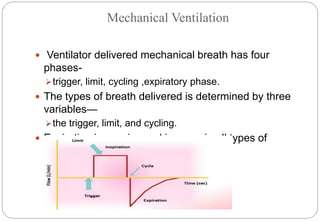

![ Inverse ratio ventilation (IRV) is not a mode of mechanical
ventilation, but rather a strategy employed during volume-
limited or pressure-limited mechanical ventilation.
The inspiratory time exceeds the expiratory time during IRV (the
inspiratory to expiratory [I:E] ratio is inversed), increasing the
mean airway pressure and potentially improving oxygenation.
A trial of IRV may be warranted when a patient is severely
hypoxemic despite optimal positive end-expiratory pressure
(PEEP) and fraction of inspired oxygen (FiO2).](https://image.slidesharecdn.com/differentmodesofventilationdrbikal-201223074455/85/Different-modes-of-ventilation-dr-bikal-24-320.jpg)