This document discusses the evaluation and management of acute diarrhea. It defines diarrhea and differentiates between acute, persistent, and chronic diarrhea. The major causes of acute infectious diarrhea are discussed as viruses, bacteria, and protozoa. The document outlines the pathogenesis of infectious diarrhea including osmotic/malabsorptive, secretory, intestinal barrier disruption, intestinal motility changes, and inflammatory mechanisms. Key points on history taking and physical examination are provided. Indications for laboratory and stool diagnostic testing include severe illness, bloody diarrhea, high-risk hosts, prolonged symptoms, and public health concerns.


![ETIOLOGY
Most cases of acute diarrhea are due to infections and are self-limited.
The major causes of acute infectious diarrhea include
viruses (norovirus, rotavirus, adenoviruses, astrovirus, and others),
bacteria (Salmonella, Campylobacter, Shigella, enterotoxigenic Escherichia
coli, Clostridioides [formerly Clostridium] difficile, and others), and
protozoa (Cryptosporidium, Giardia, Cyclospora, Entamoeba, and others)
Taken together, most cases of acute infectious diarrhea are likely viral, as indicated by
the observation that stool cultures are positive in only 1.5 to 5.6 percent of cases in most
studies
Among those with severe diarrhea, however, bacterial causes are responsible for most
cases. As an example, in a study of 173 healthy adults with severe acute community-
acquired diarrhea (defined in this study as ≥4 fluid stools per day for more than three
days), a bacterial pathogen was identified in 87 percent of cases .
Protozoa are less commonly identified as the etiologic agents of acute gastrointestinal
illness.
Noninfectious etiologies become more common as the course of the diarrhea persists
and becomes chronic.](https://image.slidesharecdn.com/diarrhea-201014122317/85/Diarrhea-3-320.jpg)


















![Gut Physiology
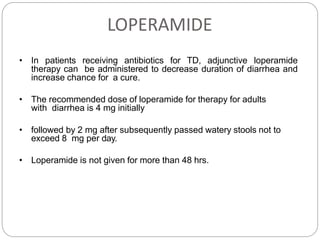
Intestinal physiologyAbsorption and secretion regulated by ion transporters
• 1. Sodium/hydrogen exchangers
(NHEs)
• 2. Sodium/glucose cotransporter
(SGLT1, SLC5A1)
• 3. Down-regulated in adenoma
(DRA [SLC26A3)
• 4. Epithelial sodium channel (ENaC)
• 5. Ca-activated chloride channels
• 6. Sodium/potassium/chloride
cotransporter 1 (NKCC1,
[SLC12A2])
• 7. Cystic fibrosis transmembrane
conductance regulator (CFTR)
• 8. Na,K ATPase:](https://image.slidesharecdn.com/diarrhea-201014122317/85/Diarrhea-22-320.jpg)