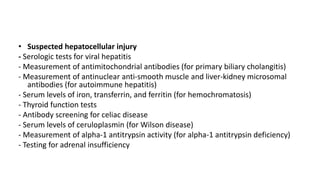
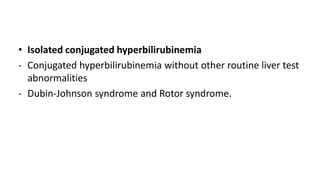
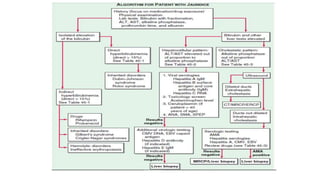
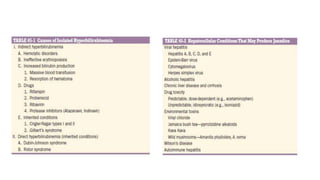
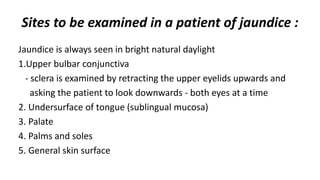
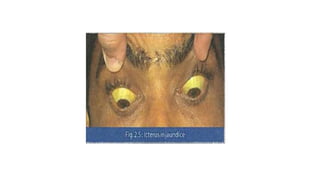
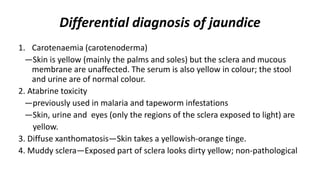
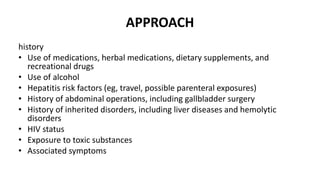
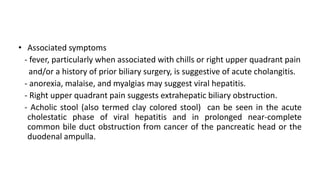
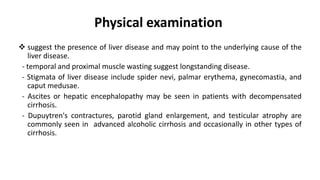
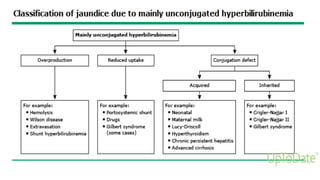
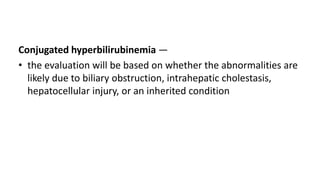
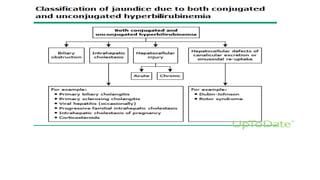
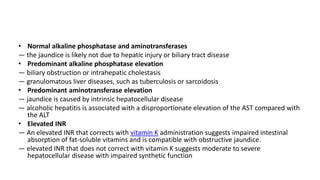
This document provides an overview of the approach to evaluating and diagnosing a patient with jaundice. It discusses examining various sites on the body for signs of jaundice. Common causes of jaundice are discussed such as those resulting from prehepatic, hepatic, and posthepatic issues. The document outlines the importance of obtaining a thorough history and physical exam. It also discusses initial laboratory tests that should be ordered and how to interpret the results to determine if the jaundice is caused by hepatocellular injury, biliary obstruction, or other issues. Imaging studies and additional lab tests are recommended based on the initial findings.

![Initial laboratory tests
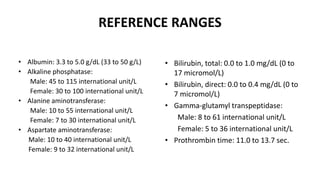
• serum total and unconjugated bilirubin,
• alkaline phosphatase
• aminotransferases (aspartate aminotransferase [AST] and
alanine aminotransferase [ALT]),
• prothrombin time/international normalized ratio (INR)
• albumin](https://image.slidesharecdn.com/approachtojaundicebikal-201014122312/85/Approach-to-jaundice-bikal-16-320.jpg)
![• suspected biliary obstruction or intrahepatic cholestasis
— ultrasound, magnetic resonance cholangiopancreatography [MRCP],
endoscopic retrograde cholangiopancreatography [ERCP]) to look for
evidence of intra- or extrahepatic bile duct dilation
• If imaging is negative, the evaluation typically will also include obtaining an
antimitochondrial antibody to evaluate for primary biliary cholangitis
• In the patient with
— low probability of obstruction: abdominal CT should be performed
— dilated biliary ducts are visualized: direct imaging of the biliary tree (eg,
with ERCP) should be performed.
— extrahepatic obstruction : endoscopic ultrasound (EUS) or ERCP](https://image.slidesharecdn.com/approachtojaundicebikal-201014122312/85/Approach-to-jaundice-bikal-22-320.jpg)