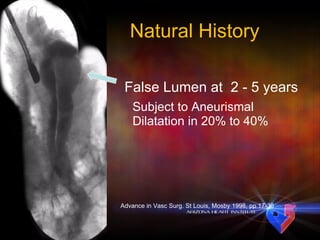
1. Endovascular techniques are increasingly being used to treat aortic pathologies like aneurysms and dissections as they can reduce mortality and morbidity compared to open surgery.
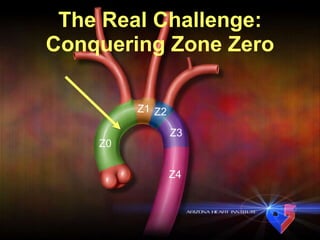
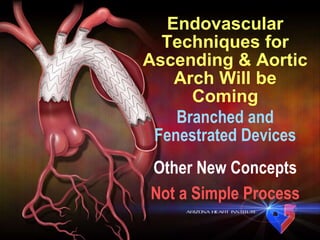
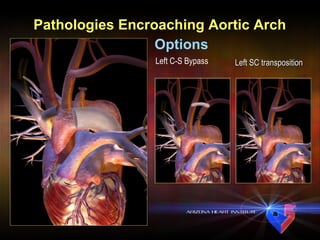
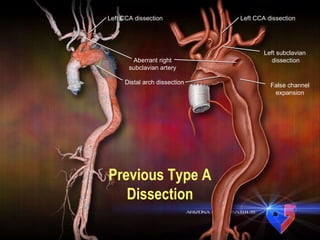
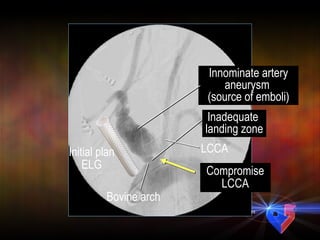
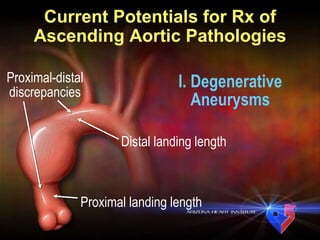
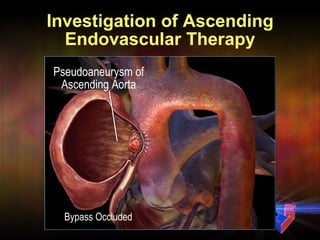
2. However, many challenging cases involve the ascending aorta and aortic arch, which are still difficult to treat using endovascular methods alone due to anatomical constraints.
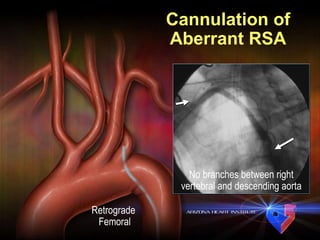
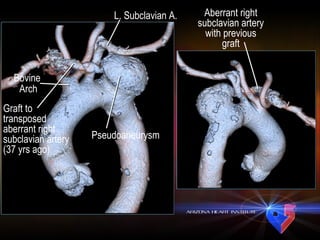
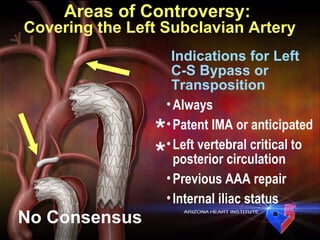
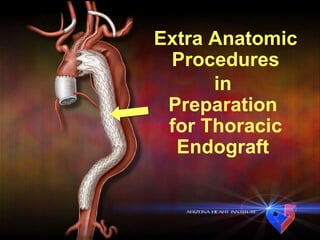
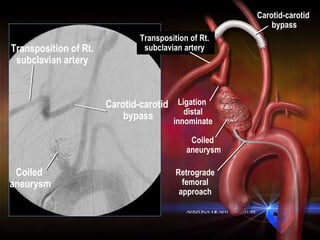
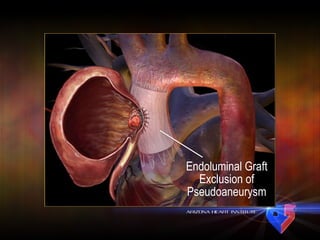
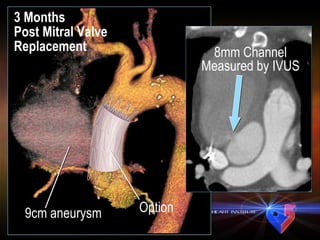
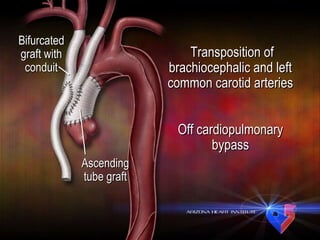
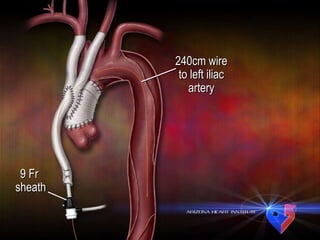
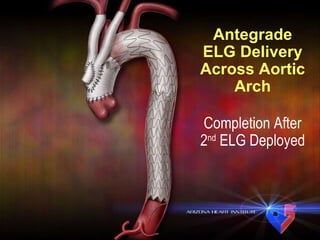
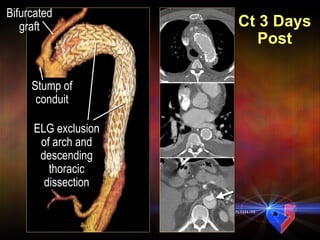
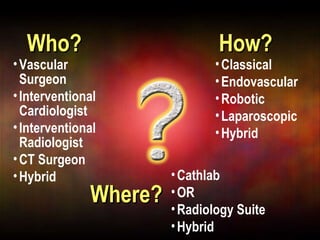
3. Hybrid procedures combining endovascular and open surgical techniques show promise for expanding the applications of endovascular therapy in complex cases, with extra-anatomic bypass grafts and branches helping to create adequate landing zones for endografts.




![Acute Type A Dissection No AI Limited to zone 0 [endovascular treatment] Type I arch/descending Ascending tube What Perspective? Progressive dissection not inconsequential](https://image.slidesharecdn.com/diethrich-sweden-1278075545-phpapp02/85/Diethrich-Sweden-7-320.jpg)