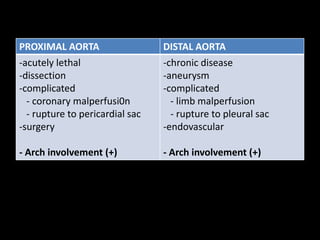
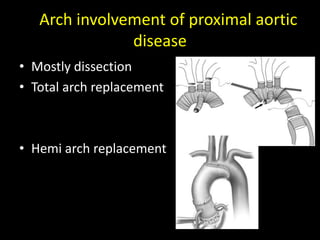
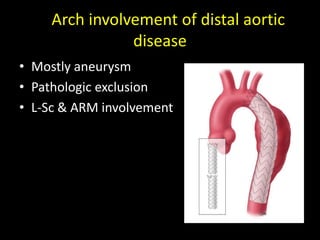
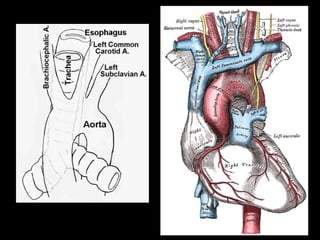
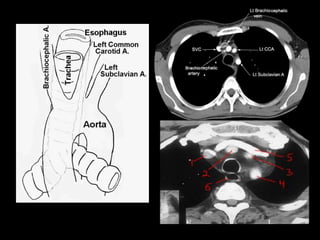
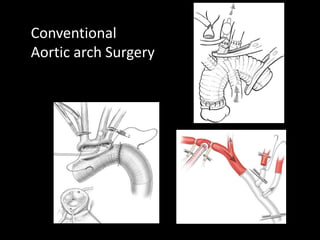
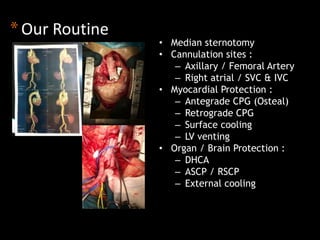
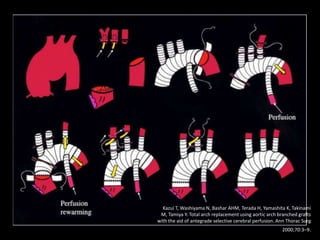
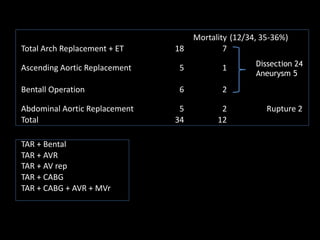
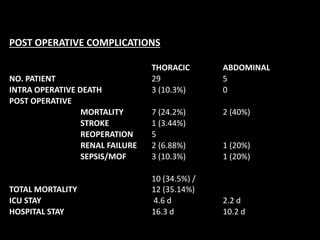
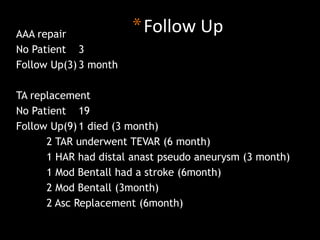
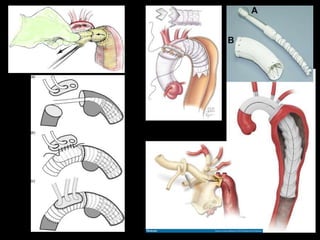
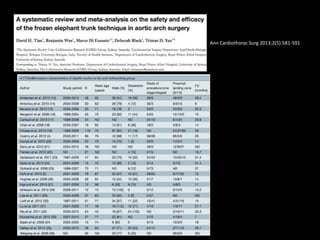
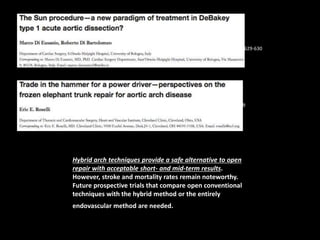
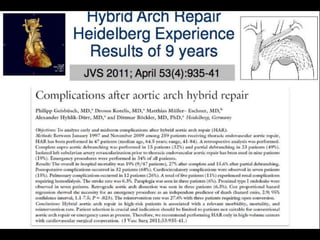
This document summarizes surgical management of complex aortic arch pathology. It discusses techniques for aortic arch surgery including conventional approaches using median sternotomy with cannulation of the axillary or femoral artery and selective cerebral perfusion. It also discusses hybrid techniques combining endovascular stent grafting with open surgery. Outcomes from one institution treating 29 patients with complex aortic arch pathology using conventional surgery are presented, with in-hospital mortality of 35% and stroke rate of 3.4%. The document concludes that aortic arch surgery remains challenging but some advances have been made, though drawbacks still exist.