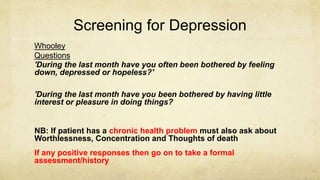
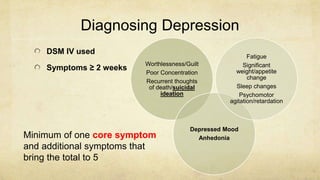
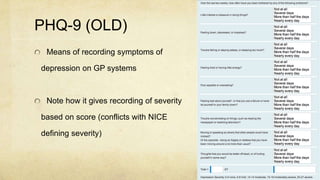
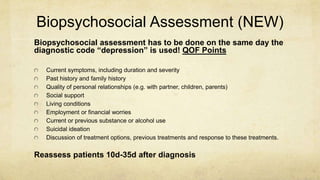
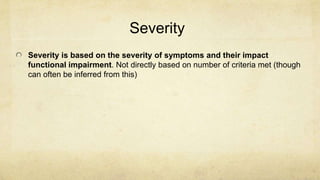
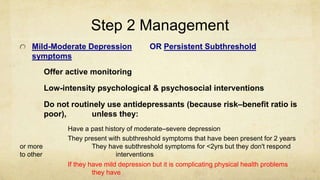
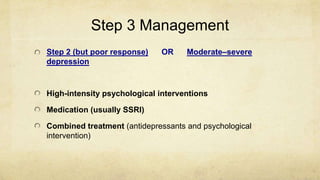
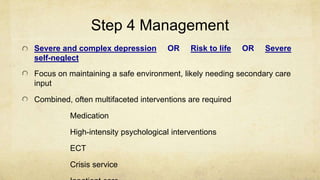
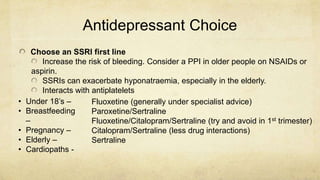
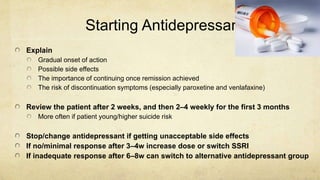
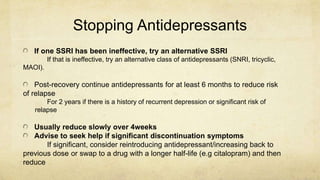
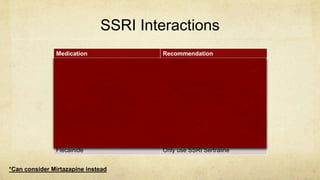
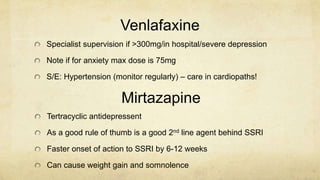
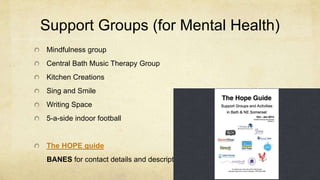
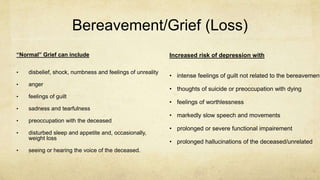
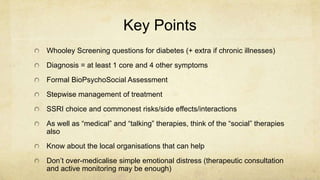
This document provides guidance on assessing and managing depression in primary care. It outlines how to screen for depression using the Whooley questions, assess severity using tools like the PHQ-9, and conduct a biopsychosocial evaluation. A stepwise treatment approach is recommended starting with active monitoring or low-intensity therapies for mild cases, and introducing antidepressants and high-intensity therapies for more severe or treatment-resistant depression. Guidance is given on choosing, starting, monitoring, and stopping antidepressants safely. Local support services and resources are also reviewed.