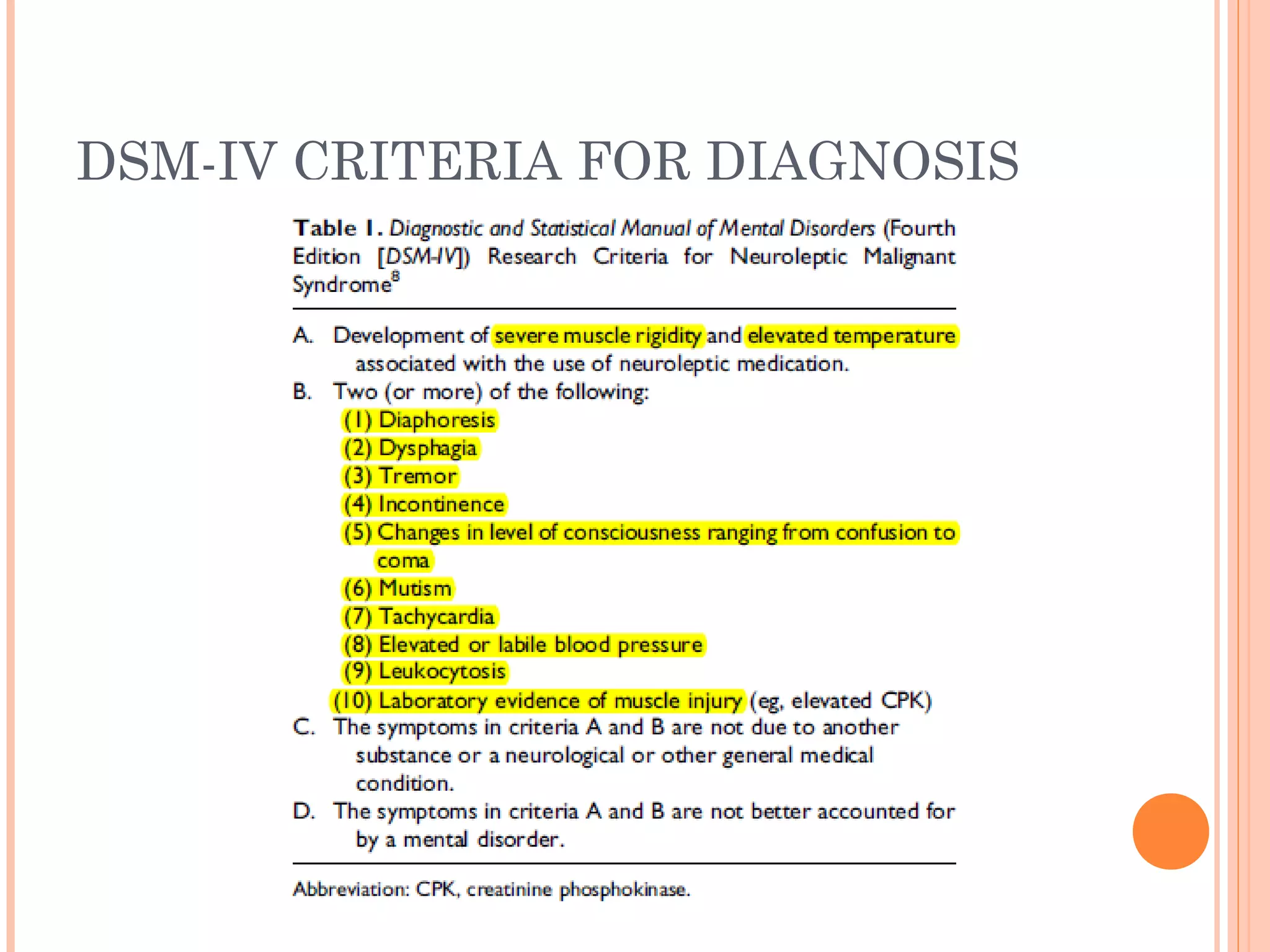
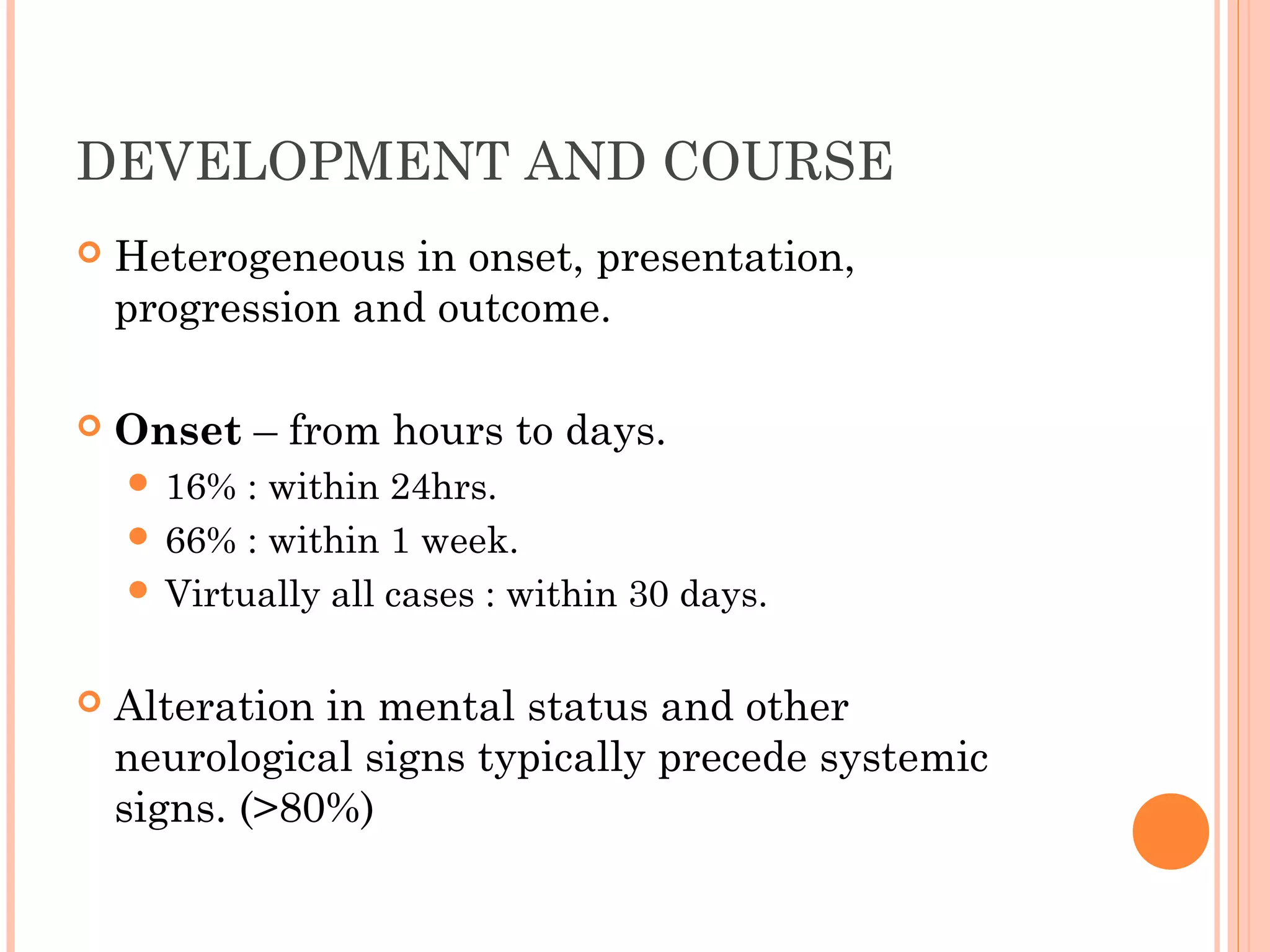
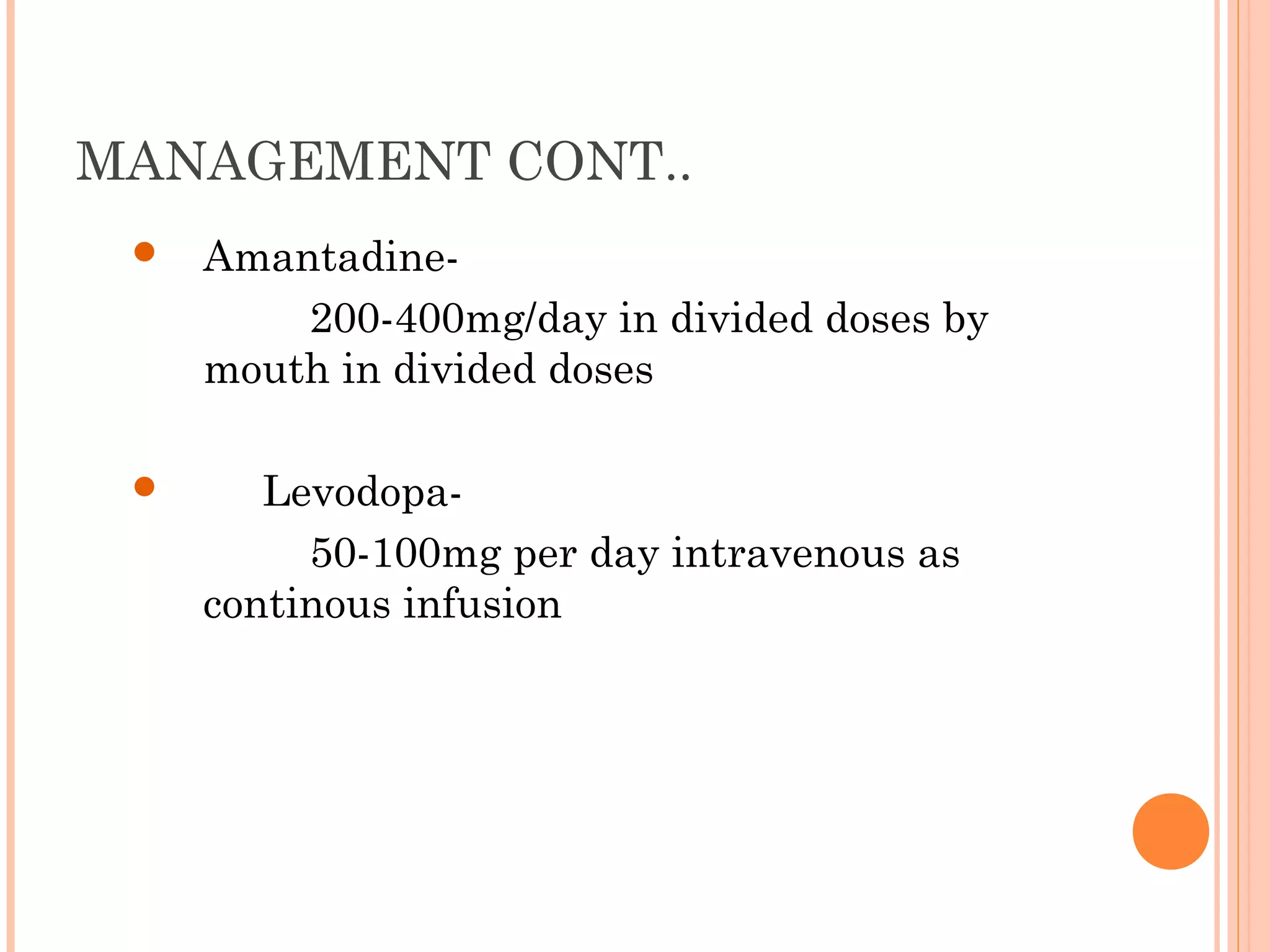
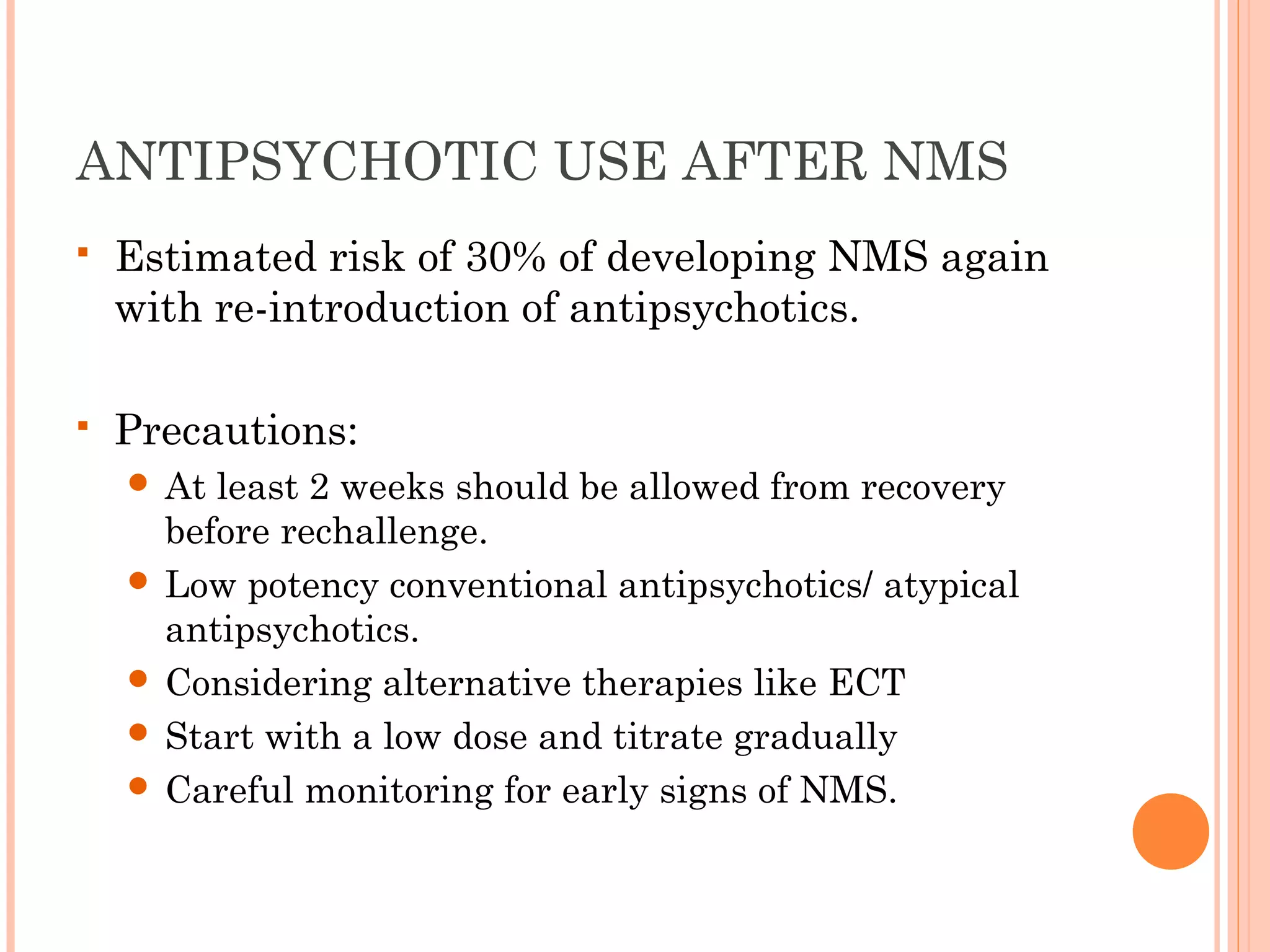
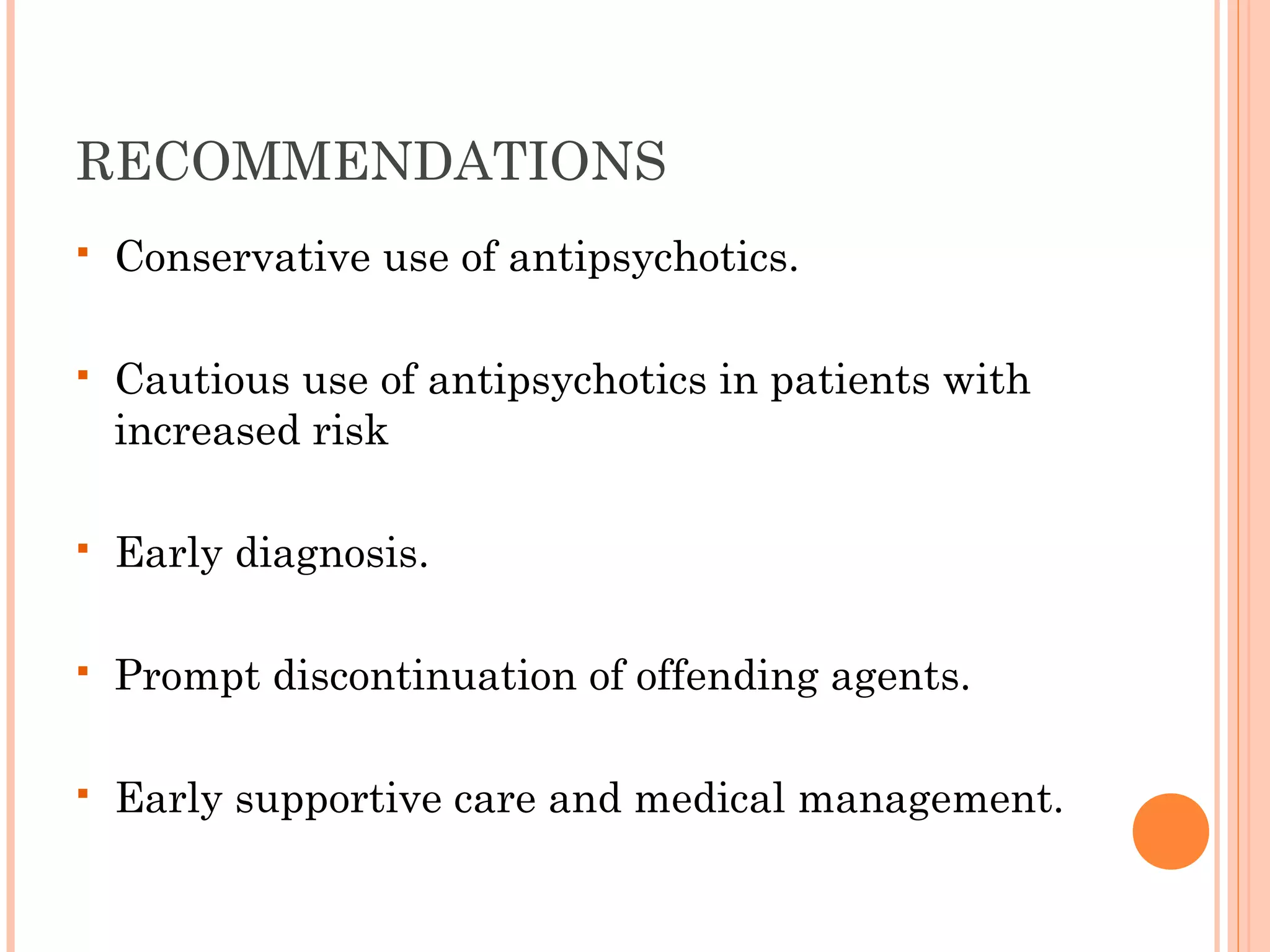
Neuroleptic malignant syndrome (NMS) is a rare but potentially life-threatening disorder associated with the use of dopamine receptor antagonists like antipsychotics. It is characterized by a tetrad of symptoms including hyperpyrexia, muscle rigidity, altered mental status, and autonomic dysfunction. Treatment involves immediate withdrawal of the offending agent, aggressive supportive care, and in severe cases, pharmacological interventions like dantrolene or bromocriptine. Prognosis is generally good if diagnosed and treated early, but mortality can result from complications and occurs in around 10% of cases.