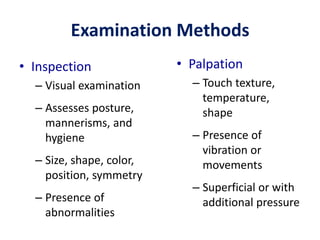
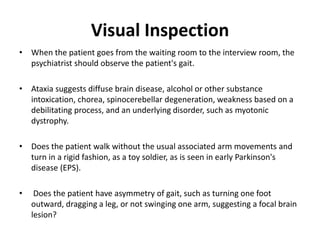
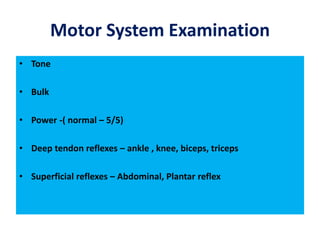
The document provides guidance on conducting a general physical examination in psychiatry. It outlines the importance of screening for physical disorders that may present with psychiatric symptoms. The general physical exam should evaluate overall appearance, vital signs, and specific organ systems. For psychiatric patients, the exam aims to identify any medical conditions contributing to their mental state. Neurological exams are particularly important to detect signs of focal brain lesions or diffuse cerebral dysfunction. Certain physical exam findings can help differentiate conversion disorder from organic conditions.