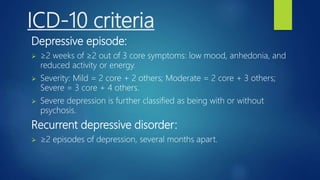
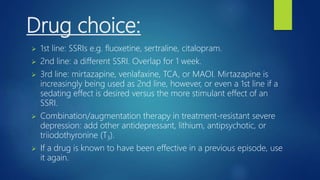
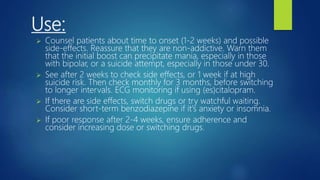
The document provides an overview of depression, including its pathophysiology, epidemiology, presentation criteria, and management strategies. It details diagnostic criteria from DSM-4 and ICD-10, treatment options including psychological interventions and antidepressants, as well as considerations for different populations such as older adults. Additionally, the document discusses the prognosis, complications, and therapeutic approaches including cognitive behavioral therapy and various classes of antidepressant medications.