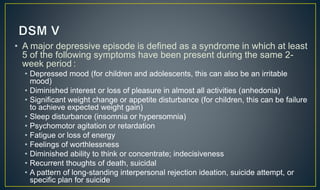
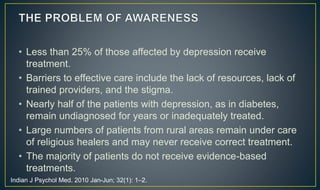
The document discusses depressive disorders, including major depressive disorder (MDD). Some key points:
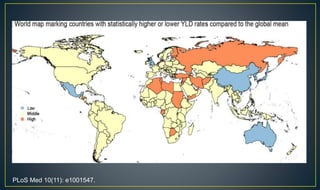
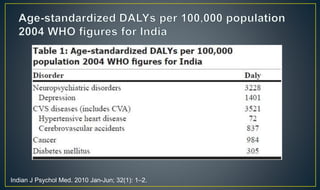
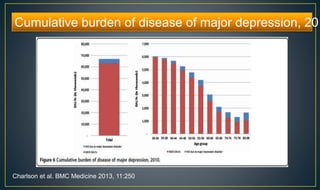
- Depressive disorders are common worldwide and a leading cause of disability. MDD accounted for 8.2% of disabilities globally in 2010.
- Prevalence of depression varies widely between studies but is estimated to be 7.9-15.1% in India. Rates are higher in urban areas, primary care clinics, and the elderly.
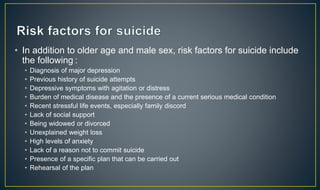
- Depression is associated with high suicide rates, accounting for 50-70% of suicides. India has high suicide rates, with 37.8% of those committing suicide being under 30.