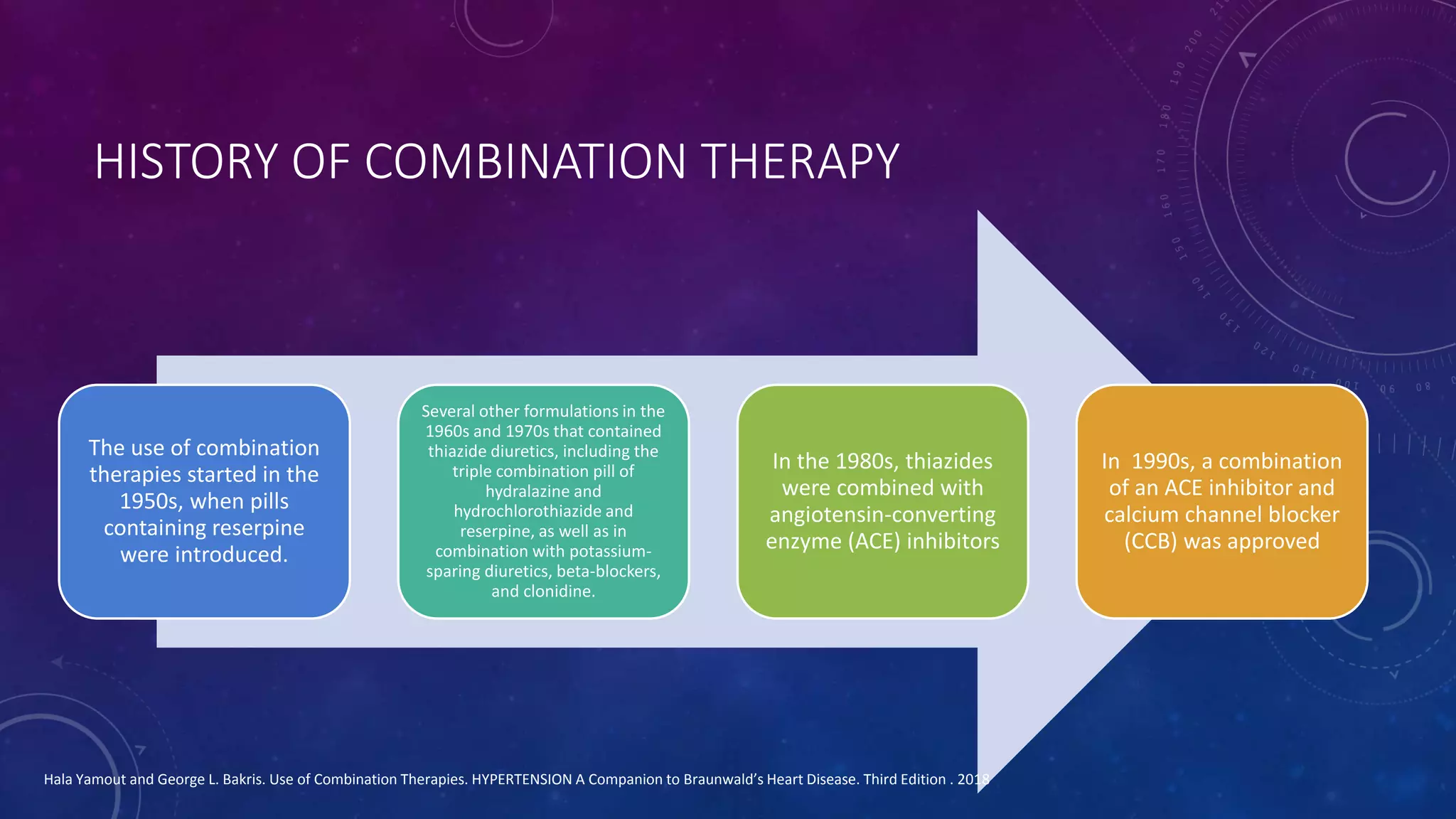
The document discusses the history and rationale for using combination therapy in the management of hypertension. It notes that combination therapy has been used since the 1950s, starting with pills containing reserpine. Major developments included the addition of thiazide diuretics in the 1960s-1970s and ACE inhibitors/calcium channel blockers in the 1980s-1990s. The rationale for initial combination therapy includes more effective blood pressure control, multi-factorial causes of hypertension, counteracting regulatory mechanisms, and improved patient adherence compared to monotherapy. Current guidelines recommend starting with dual combination therapy or advancing to triple therapy if blood pressure remains uncontrolled.