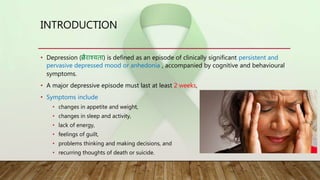
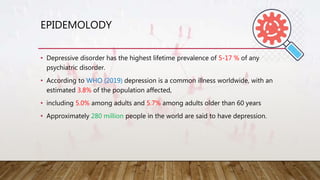
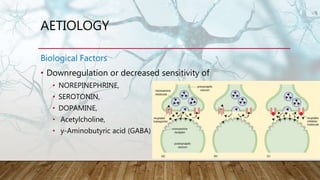
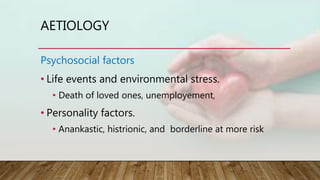
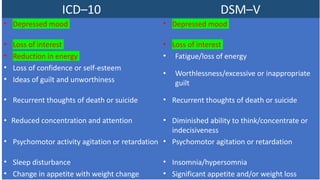
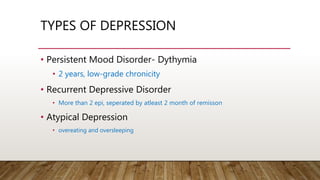
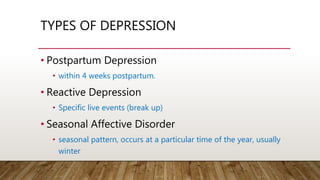
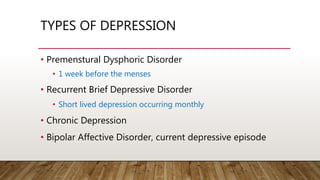
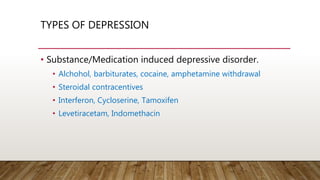
This document provides information on different types and aspects of depression. It begins with introducing depression and outlining its diagnostic criteria according to the ICD-10 and DSM-V. It then discusses the epidemiology of depression, including prevalence rates. Next, it covers various correlates, risk factors, and causes of depression including genetic, biological, and psychosocial factors. The document also describes different types of depression and discusses depression in special populations such as children/adolescents, the elderly, pregnant women, and those with medical conditions like stroke, diabetes, heart disease, and cancer. Finally, it outlines treatment approaches for depression including psychotherapy, lifestyle changes, and pharmacotherapy.