This document discusses alcohol use disorder and provides information on its historical aspects, epidemiology, types of alcoholic beverages, effects on the body, etiology, and diagnostic criteria. Some key points:
- Alcohol has been used by humans for intoxication purposes throughout history, with the earliest evidence of intentionally fermented beverages dating back over 10,000 years.
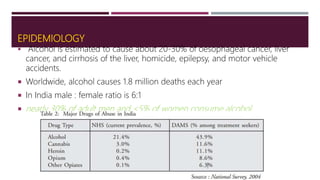
- Worldwide, alcohol causes over 1.8 million deaths per year through conditions like cancer, liver disease, accidents, and violence.
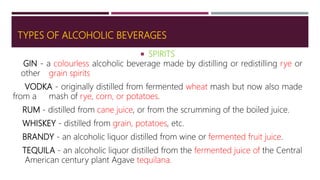
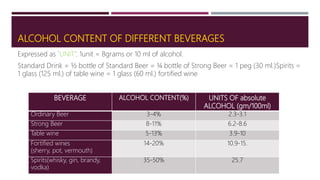
- Types of alcoholic beverages include spirits like whiskey and rum, wines, beers, and liqueurs. The alcohol content varies significantly between different types.
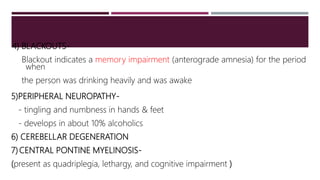
- Alcohol affects the brain through its interactions with neurotransmit

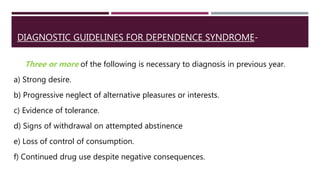
![FIVE-CHARACTER CODES FOR DEPENDENCE
F10.20 Currently abstinent
F10.21 Currently abstinent, but in a protected environment
F10.22 Currently on a clinically supervised maintenance or replacement regime
[controlled dependence]
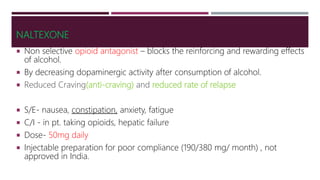
F10.23 Currently abstinent, but receiving treatment with aversive or blocking
drugs (e.g. naltrexone or disulfiram)
F10.24 Currently using the substance [active dependence]
F10.25 Continuous use
F10.26 Episodic use [dipsomania]](https://image.slidesharecdn.com/alcoholusedisorder-180422195347/85/Alcohol-use-disorder-25-320.jpg)