This document discusses dental calculus, including its definition, composition, formation, and classification. It provides the following key points:
- Dental calculus is mineralized bacterial plaque that forms on tooth surfaces. It consists of inorganic minerals like calcium phosphate embedded within an organic matrix.
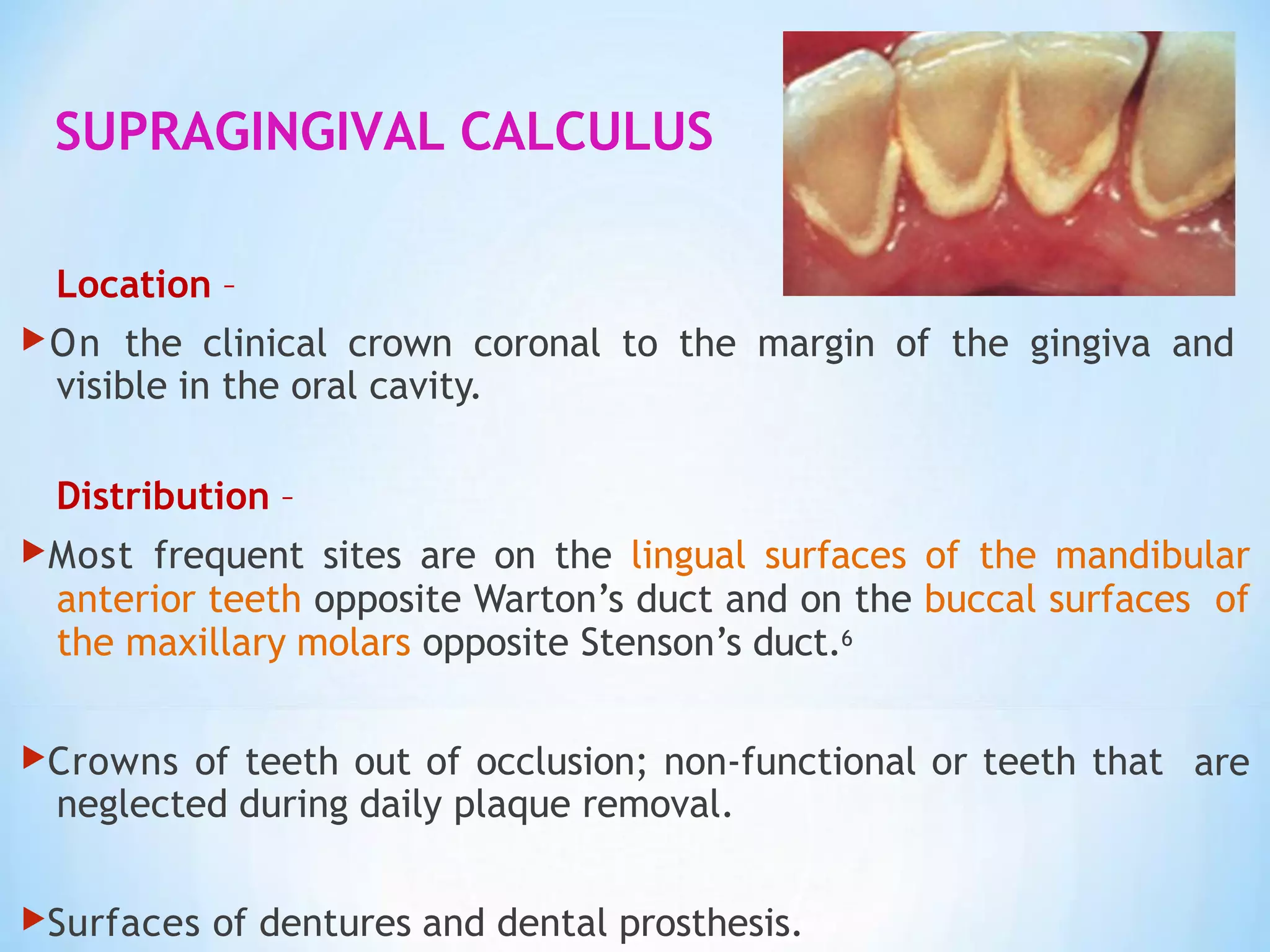
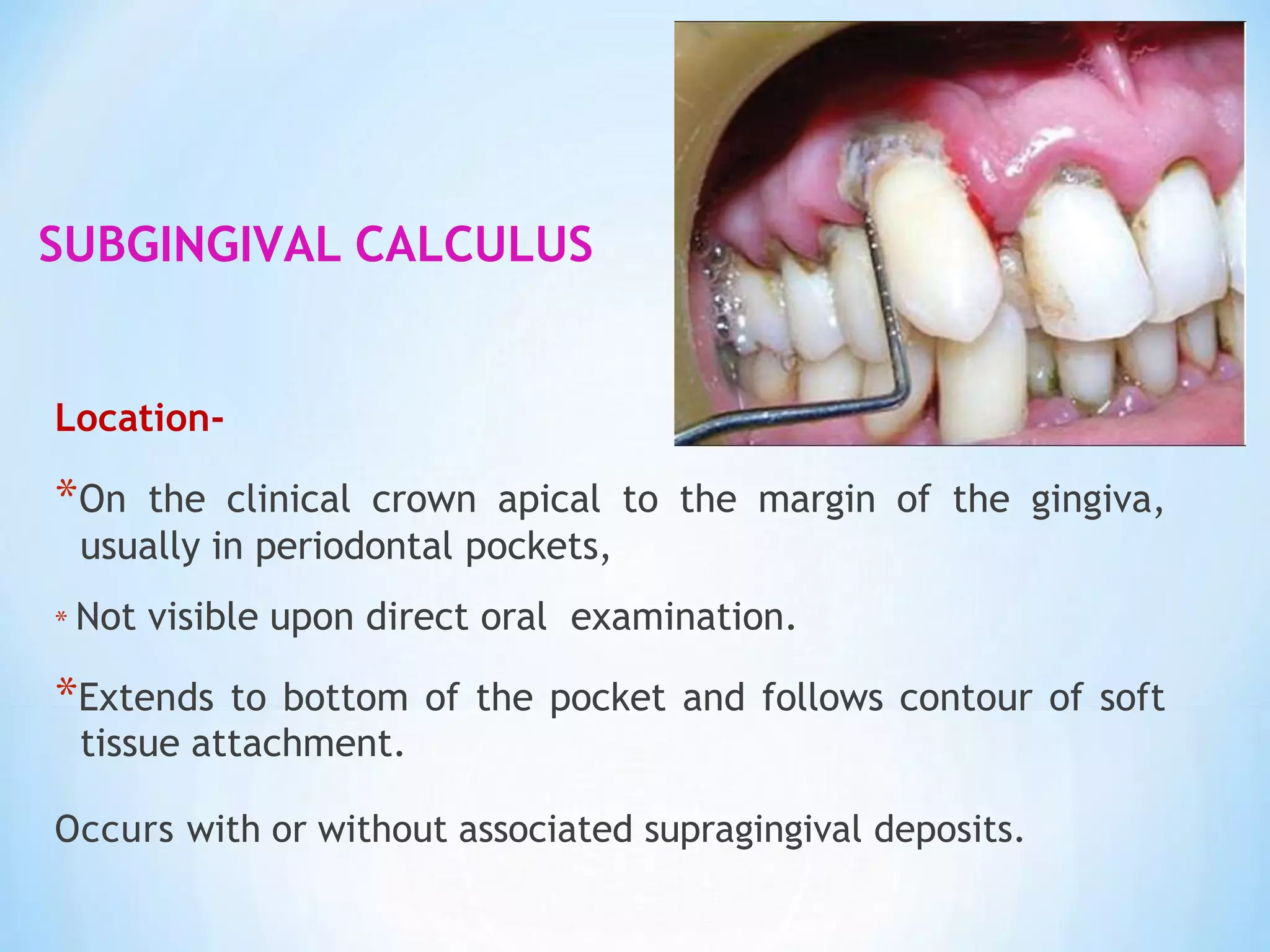
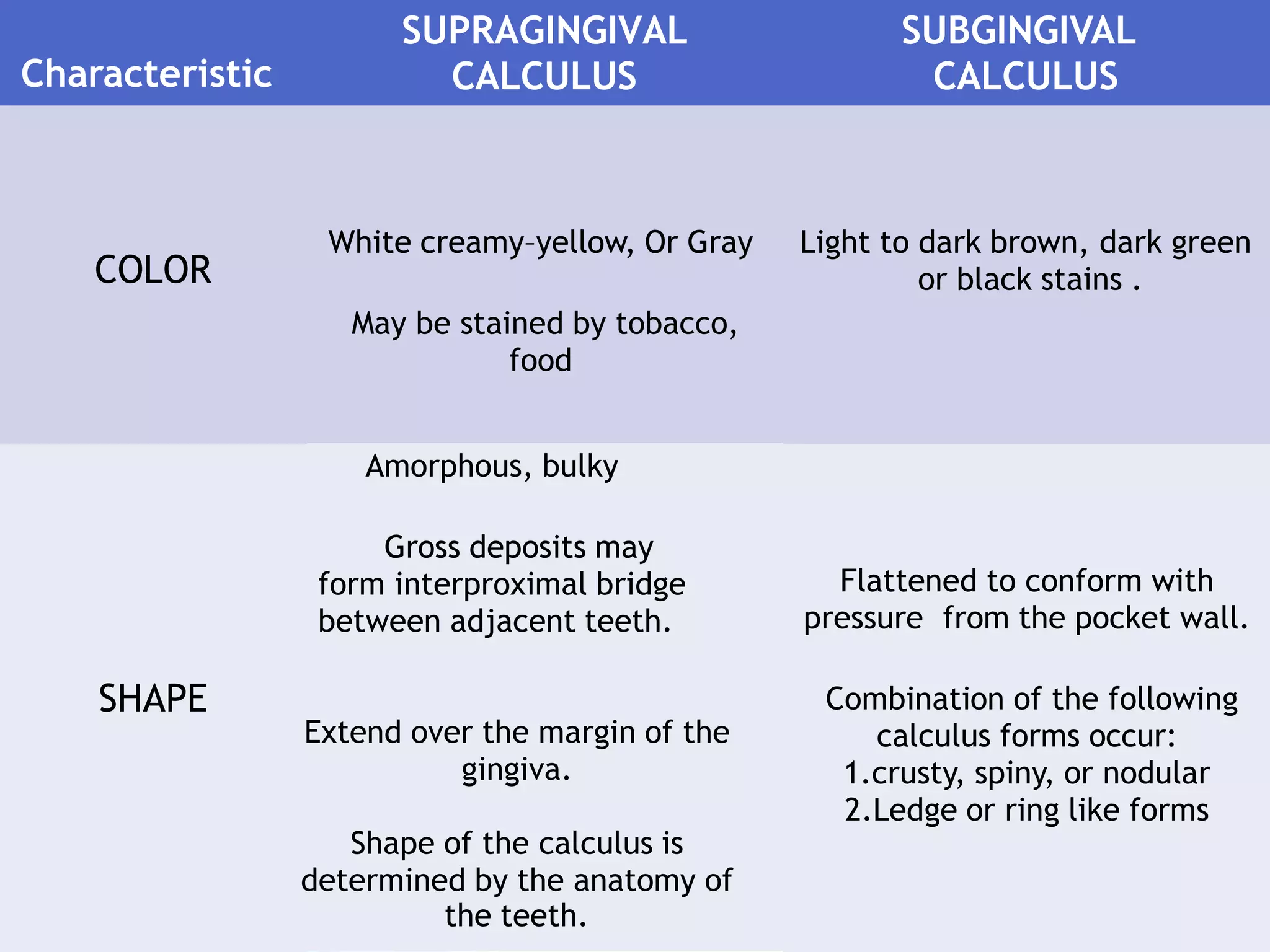
- Calculus is classified as supragingival or subgingival based on its location relative to the gingival margin. Supragingival calculus is visible while subgingival is within the gingival pocket.
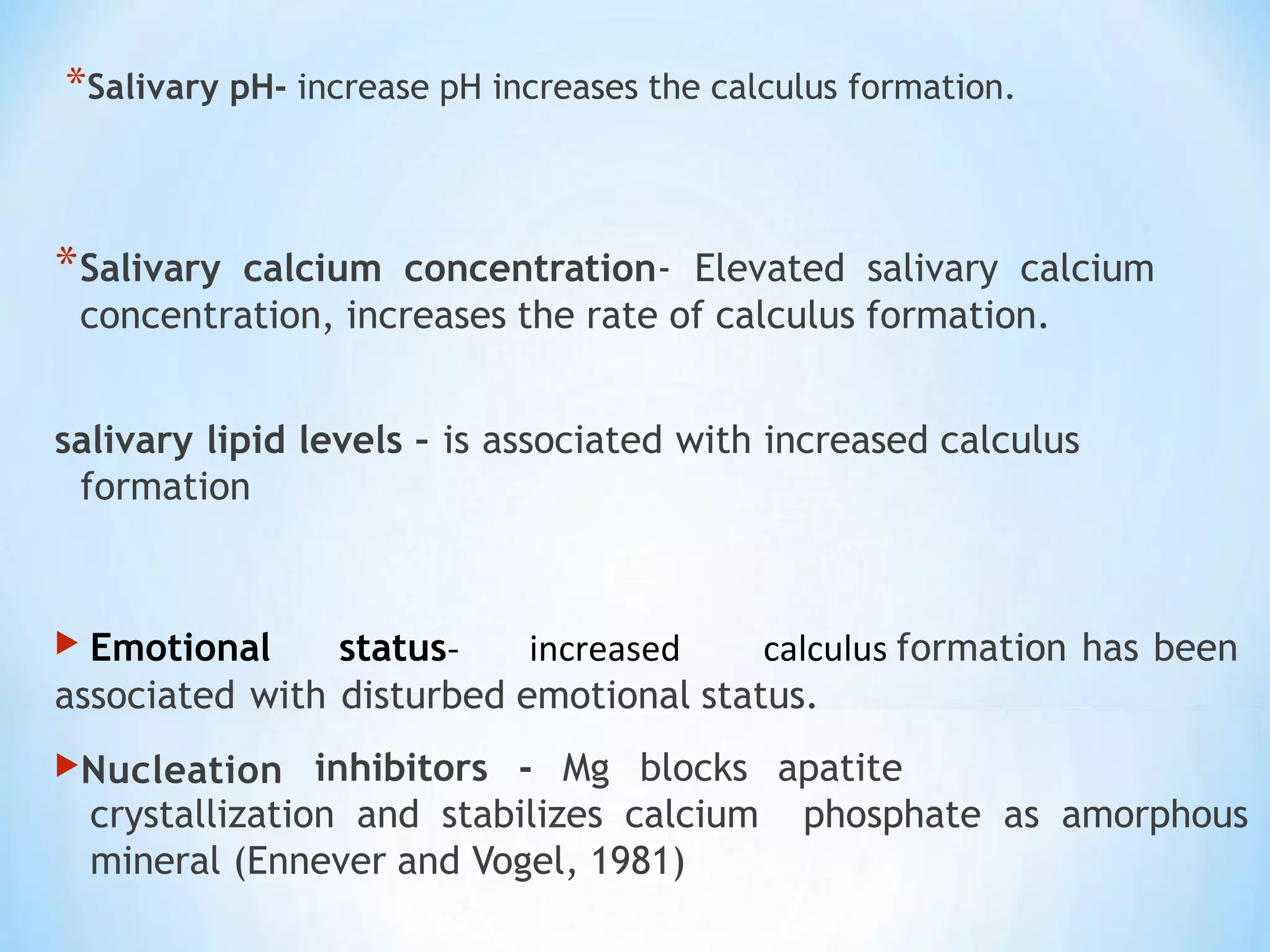
- Calculus formation occurs as plaque mineralizes over time. Various local and systemic factors can influence the rate of calculus accumulation on teeth. Regular removal is needed to prevent its buildup.


![Dental calculus can be considered as an ectopic
mineralized structure.
Dental Calculus consists of mineralized bacterial
plaque that forms on the surfaces of natural teeth and
dental prosthesis. [Carranza ]
The word "calculus" was derived from the Latin word for a
pebble or stone.
Tartar, a common synonym for dental calculus, is taken from
the Latin word tartarum which means the accumulated
sediment or crust.](https://image.slidesharecdn.com/dentalcalculusishu-230614041838-27dbf546/75/dental-calculus-ishu-pptx-3-2048.jpg)
![Calculus can be defined as a hard concretion that forms on teeth or
dental prostheses through calcification of bacterial plaque
[GPT 4th edition].
▶ Calculus is Mineralized dental plaque that is permeated with
crystals of various calcium phosphates (Schroeder,1969).
▶when dental plaque calcifies, the resulting deposit is called
CALCULUS (GRANT).](https://image.slidesharecdn.com/dentalcalculusishu-230614041838-27dbf546/75/dental-calculus-ishu-pptx-4-2048.jpg)