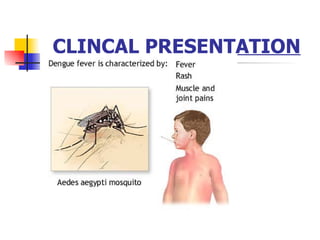
1) Dengue fever is caused by mosquitoes of the genus Aedes, mainly A. aegypti, and is prevalent during rainy seasons when mosquito populations increase. Improper waste disposal also contributes to mosquito propagation.
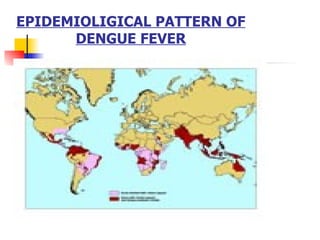
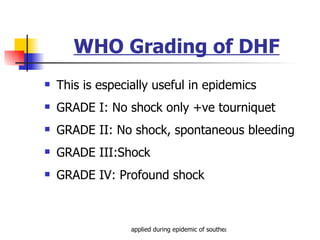
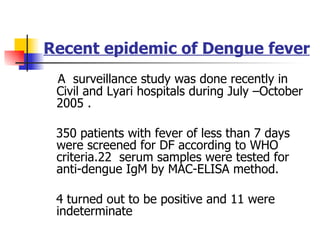
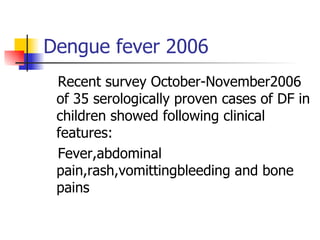
2) Dengue virus consists of 4 serotypes that cause disease in humans. Major epidemics have occurred across Asia and there have been recent outbreaks in Pakistan.
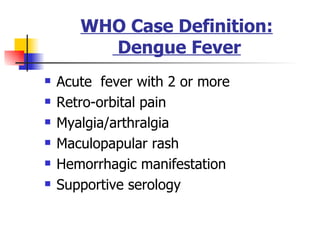
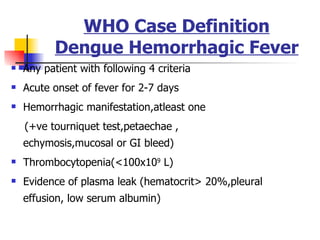
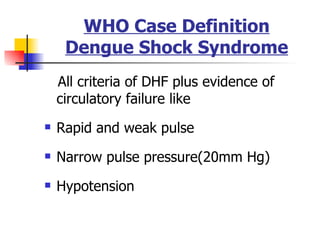
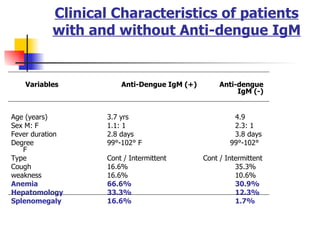
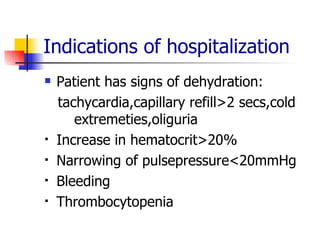
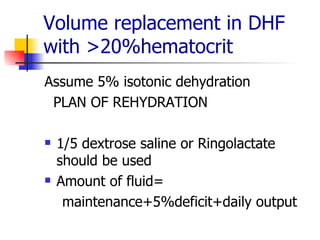
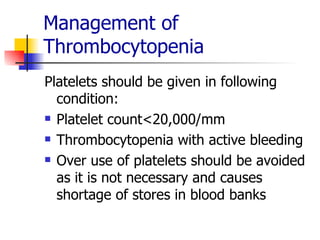
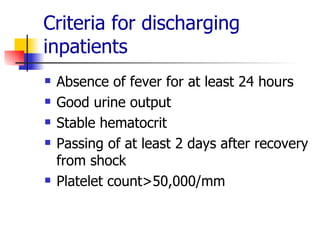
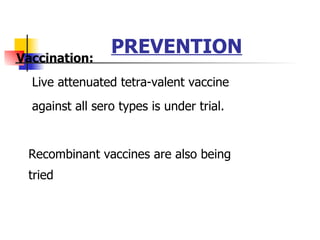
3) Clinical presentation ranges from mild dengue fever to severe dengue hemorrhagic fever/dengue shock syndrome. Outpatient management is usually sufficient but hospitalization may be needed for dehydration, bleeding, or low platelet count. Prevention relies on environmental controls and public education.