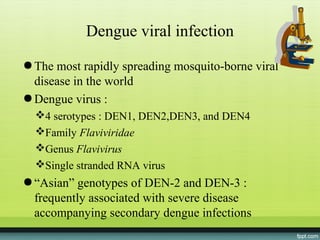
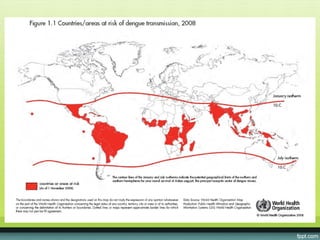
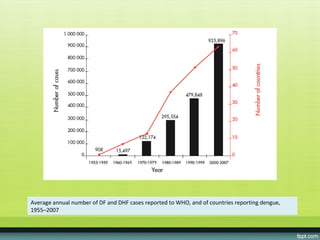
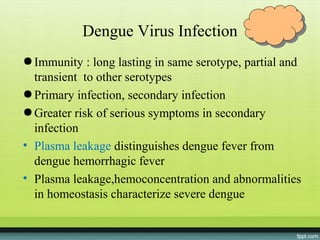
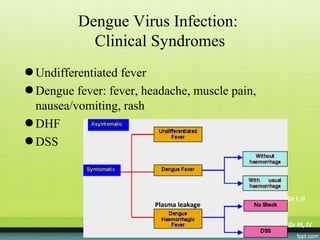
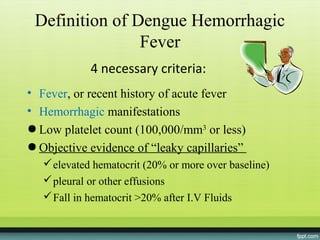
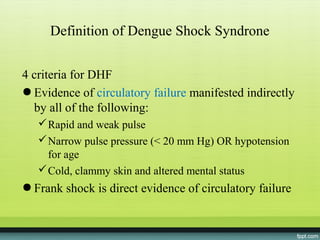
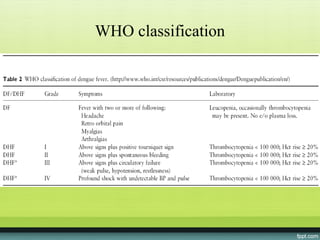
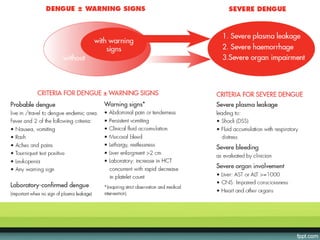
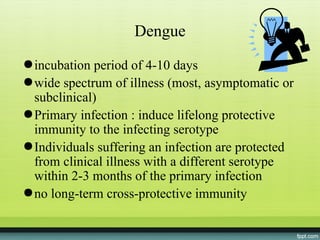
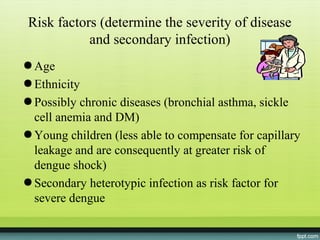
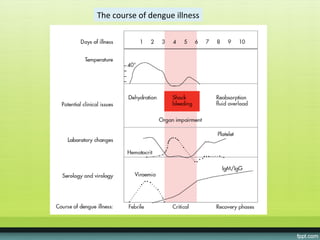
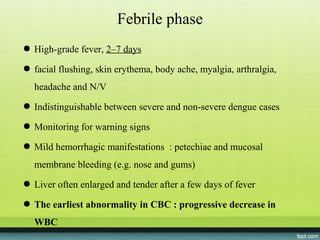
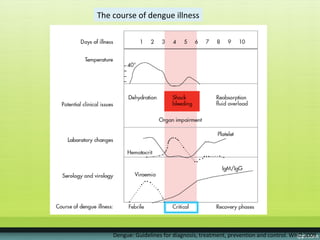
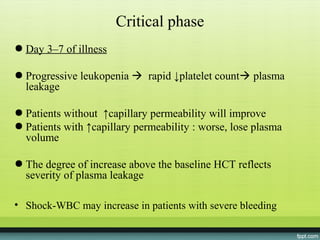
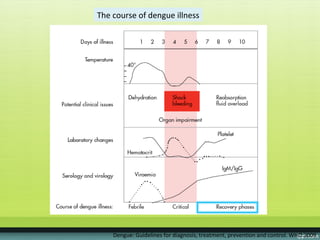
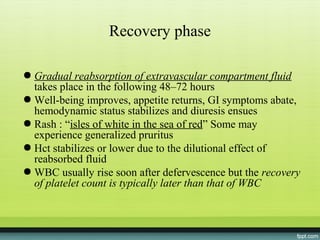
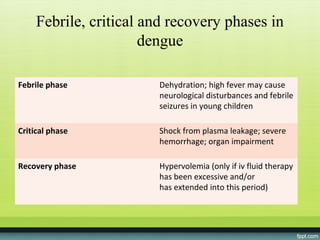
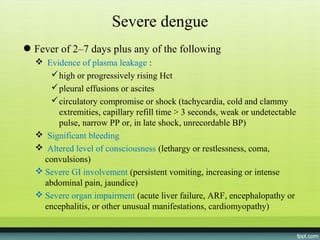
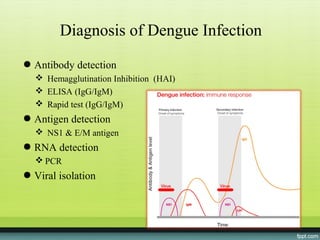
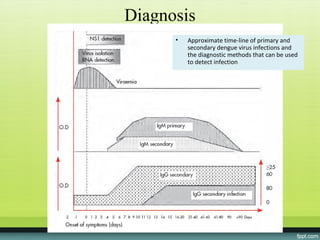
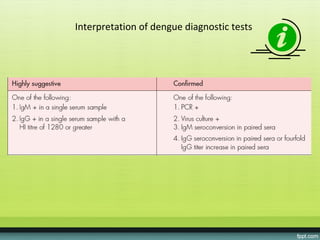
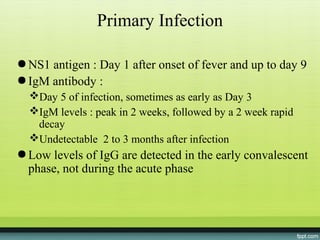
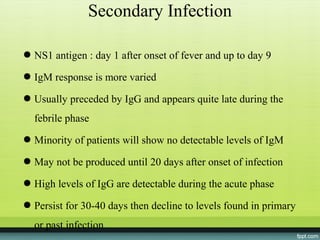
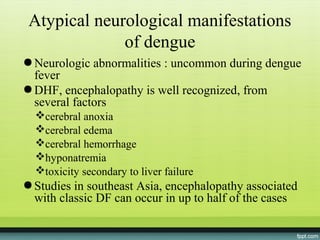
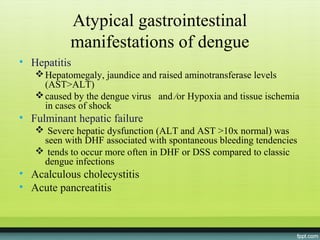
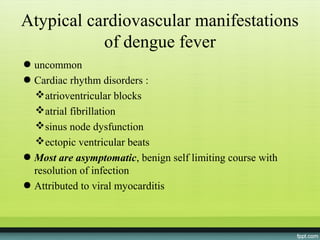
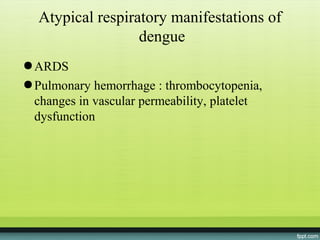
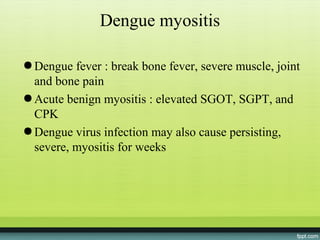
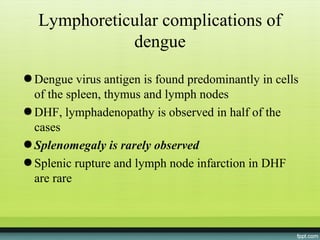
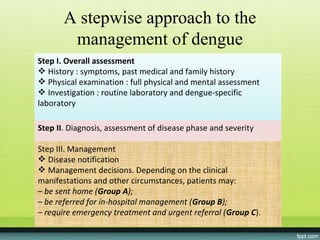
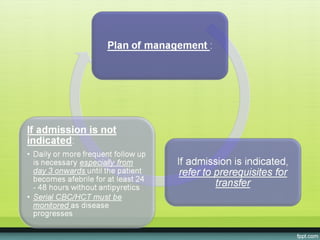
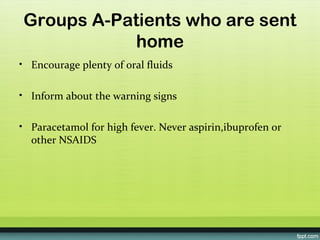
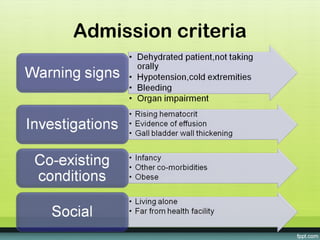
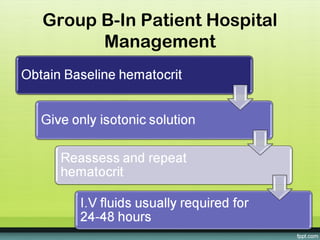
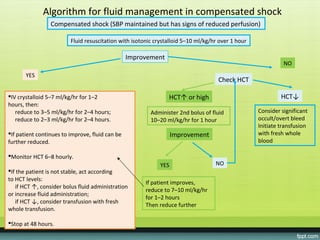
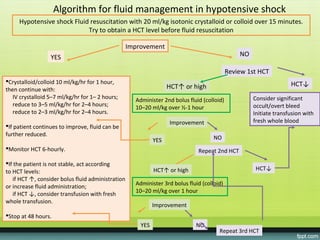
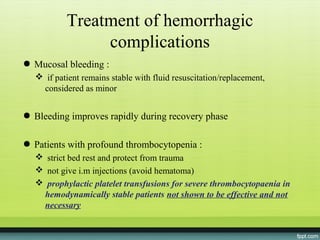
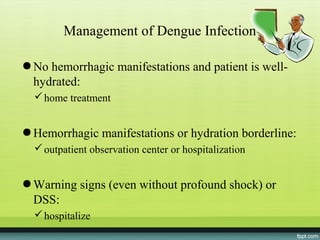
The document provides guidelines on dengue infection, discussing the clinical syndromes of dengue fever and dengue hemorrhagic fever, their diagnosis and classification, management approaches including fluid resuscitation, and treatment of complications. It describes dengue virus and the disease it causes, including its pathophysiology, clinical course, and atypical manifestations. Risk factors, vectors, and the immune response to primary and secondary infections are also covered.