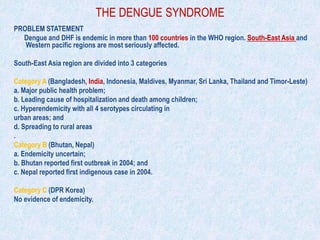
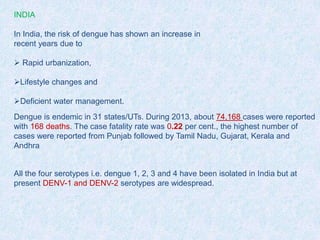
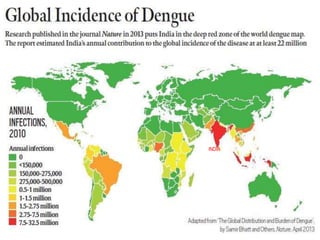
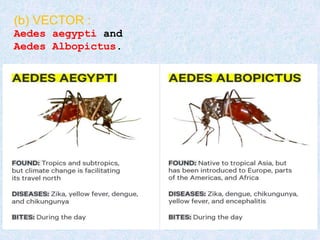
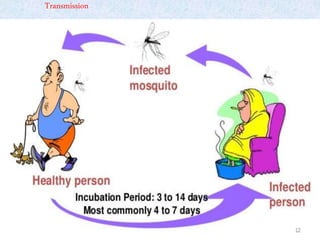
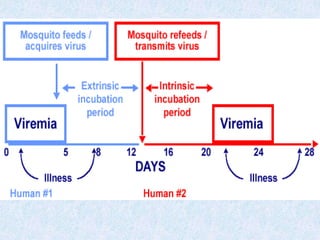
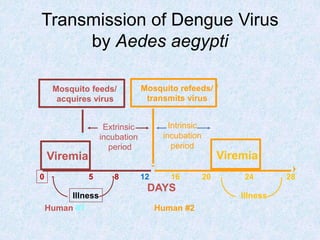
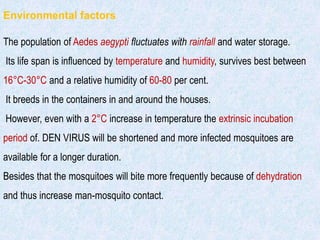
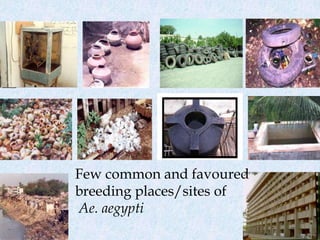
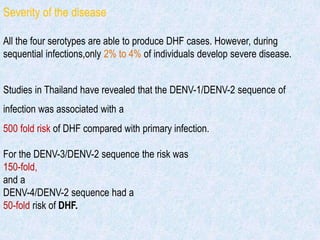
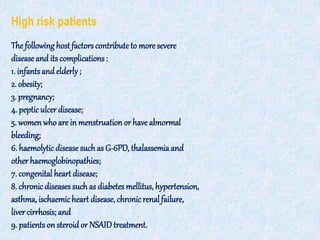
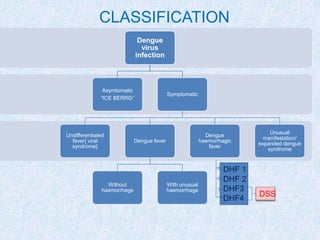
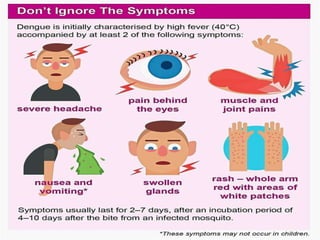
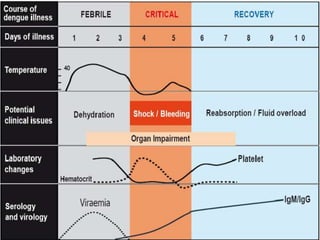
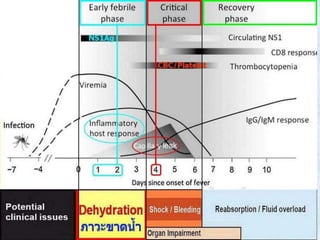
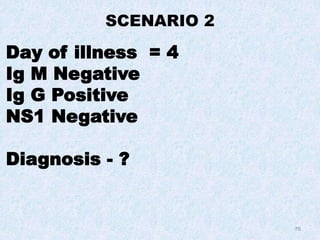
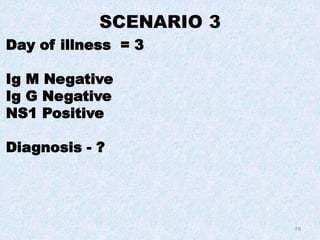
The document discusses dengue, which is endemic in many countries in Southeast Asia and the Western Pacific. It categorizes countries in Southeast Asia based on their dengue situation. India is experiencing an increase in dengue risk due to factors like rapid urbanization and lifestyle changes. The dengue virus has four serotypes and infection with one provides immunity to that serotype. Secondary infection or infection with multiple serotypes can cause severe dengue hemorrhagic fever. The Aedes mosquito transmits dengue virus between humans. Environmental factors like rainfall and temperature affect mosquito populations and transmission rates.