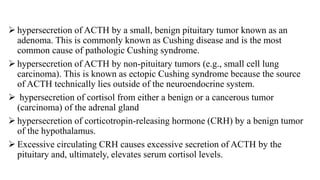
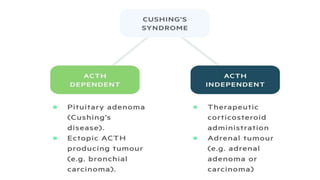
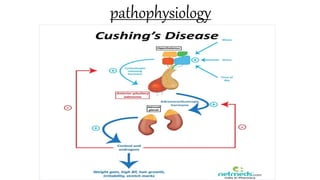
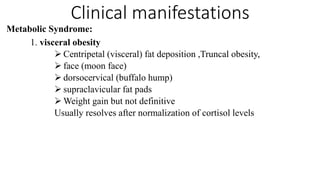
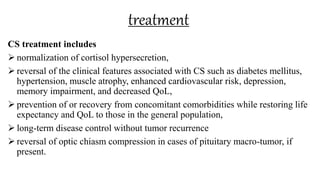
Cushing syndrome results from excessive cortisol secretion and is characterized by central obesity, muscle wasting, hyperglycemia, and hypertension. It can be caused by prolonged glucocorticoid use or tumors that secrete cortisol or ACTH. Diagnosis involves testing for cortisol levels, and treatment focuses on treating the underlying cause and managing complications through lifestyle changes and medications. Nursing care aims to prevent injuries and infections while promoting skin integrity and a healthy body image and thought processes.