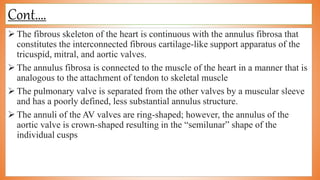
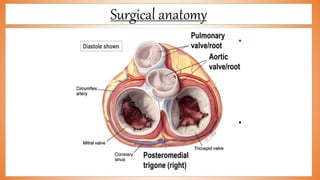
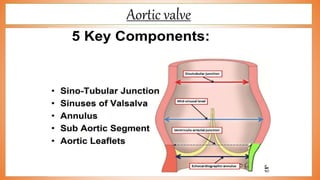
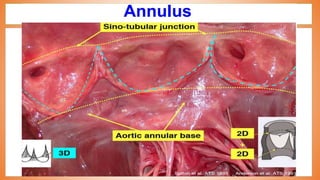
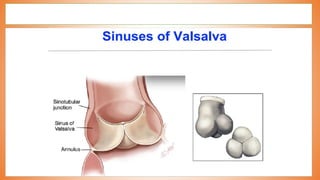
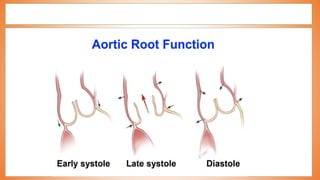
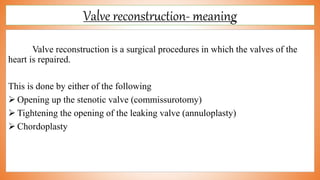
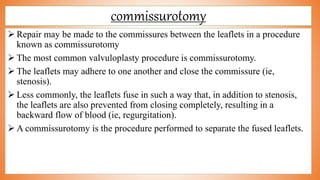
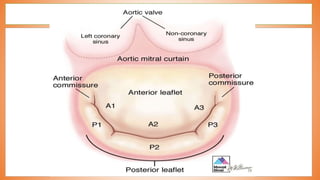
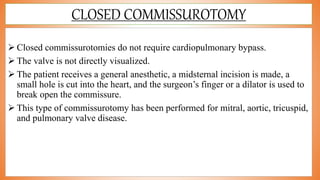
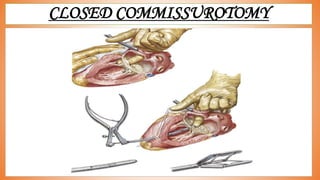
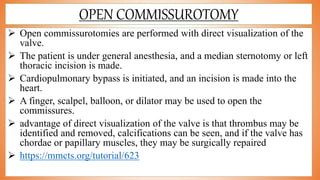
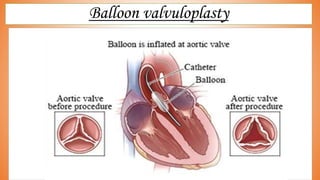
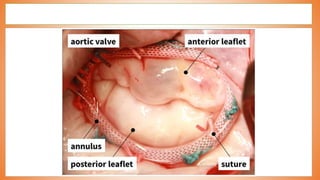
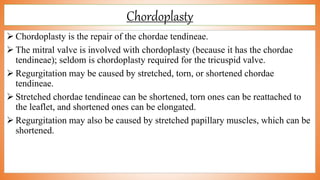
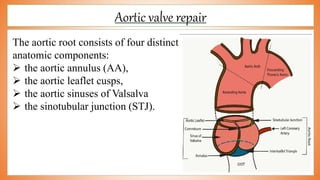
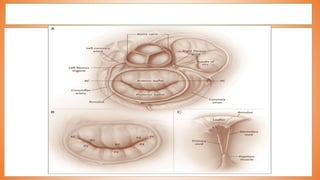
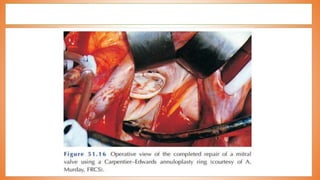
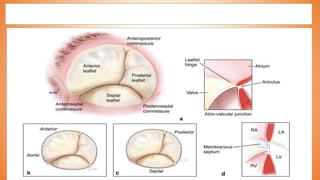
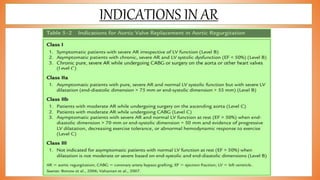
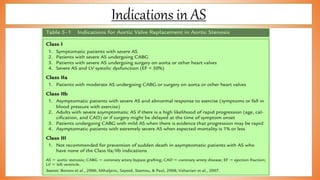
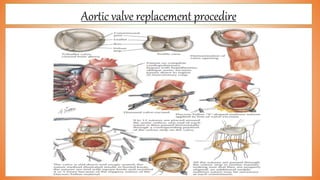
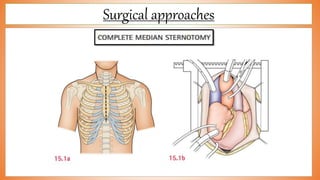
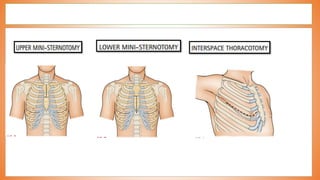
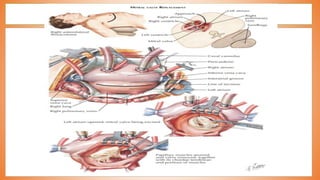
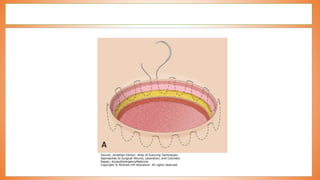
This document discusses valve reconstruction and replacement procedures for the aortic and mitral valves. It begins with an introduction to cardiac valve surgery and relevant anatomy. It then covers the history of valve surgery and discusses techniques for valve reconstruction including commissurotomy, annuloplasty, chordoplasty, and balloon valvuloplasty. Indications and surgical procedures for reconstructing specifically the aortic and mitral valves are described. The document also briefly discusses tricuspid valve anatomy, indications for surgery, and repair techniques. It concludes with a short definition of valve replacement.