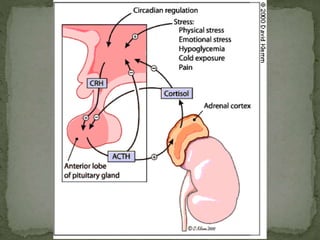
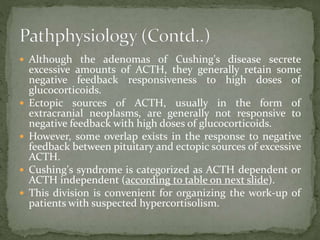
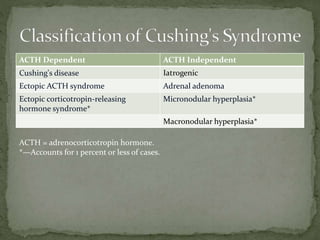
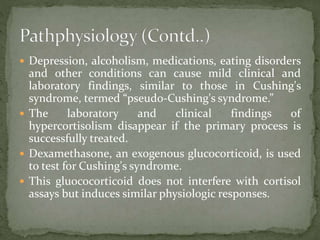
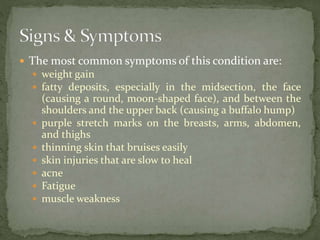
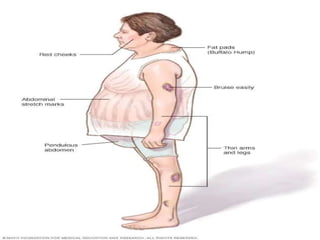
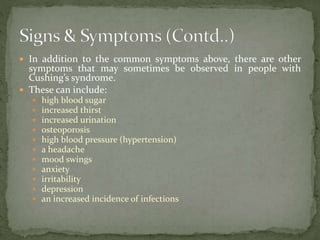
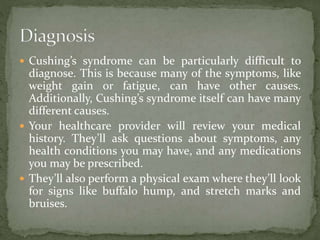
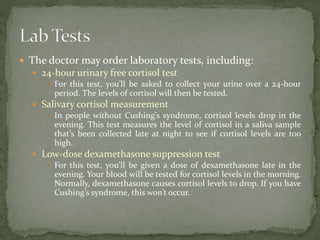
Cushing syndrome arises from excessive cortisol production, either due to the body's malfunction or prolonged use of corticosteroids, leading to symptoms like weight gain, high blood pressure, and bone loss. Diagnosis involves reviewing medical history, physical exams, and various lab tests, while treatment may include tapering off medications, surgery, or medications like mifepristone for non-surgical patients. Dietary changes can help manage symptoms but are not a cure, highlighting the complexity of diagnosing and treating this condition.