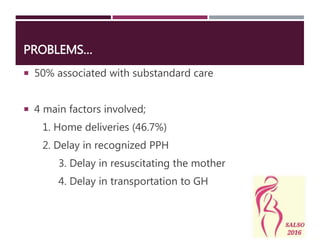
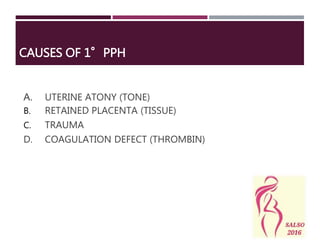
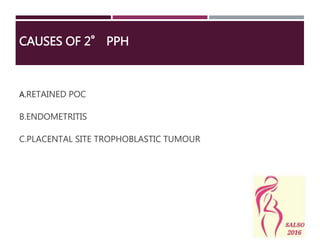
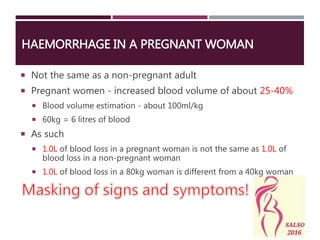
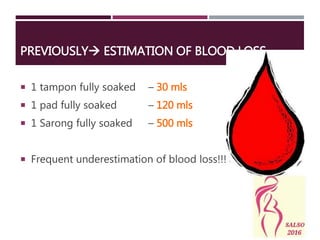
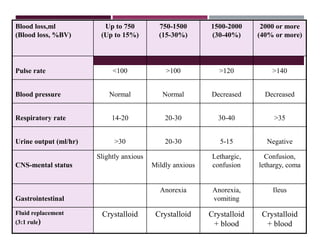
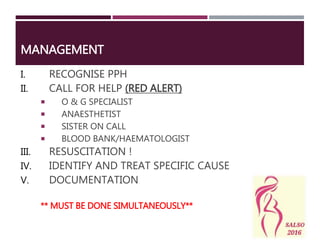
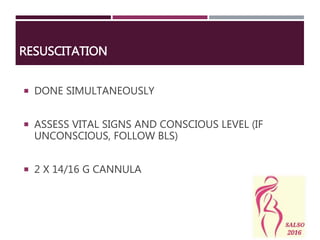
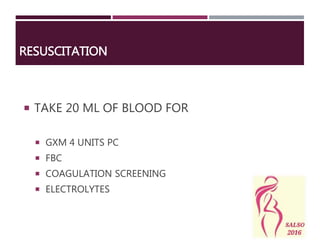
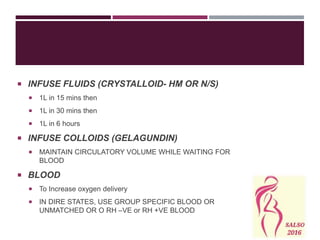
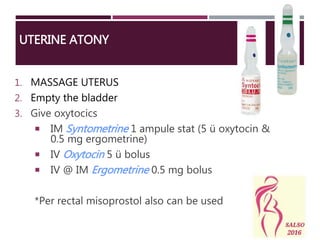
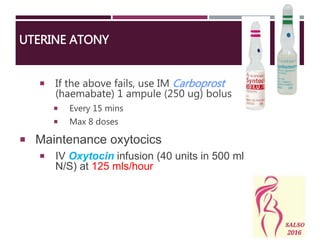
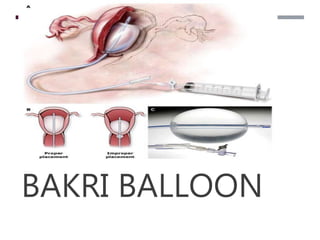
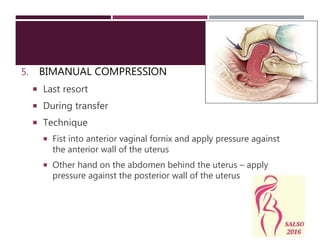
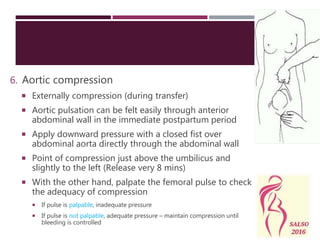
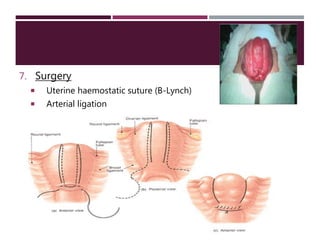
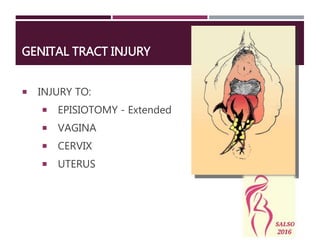
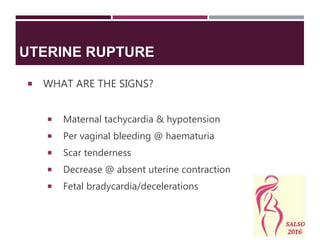
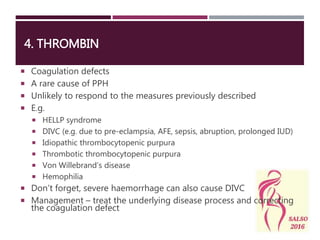
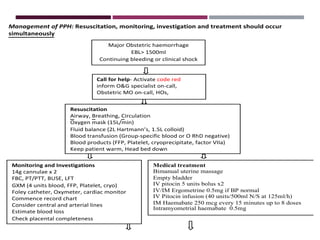
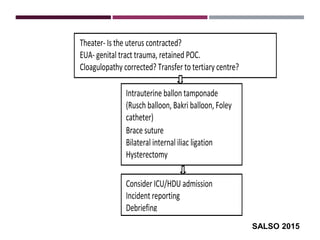
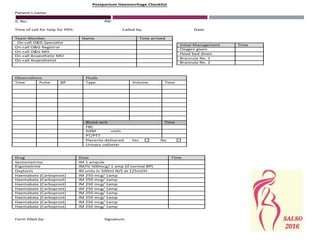
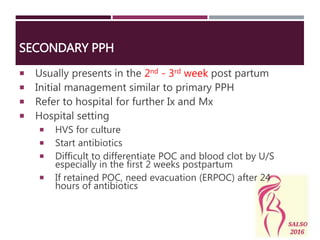
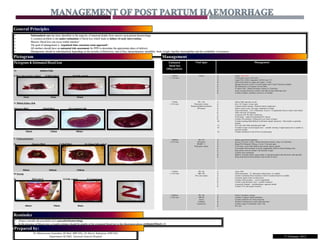
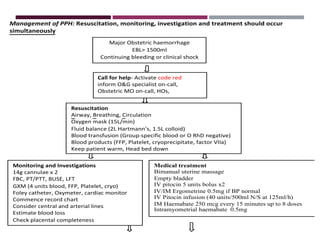
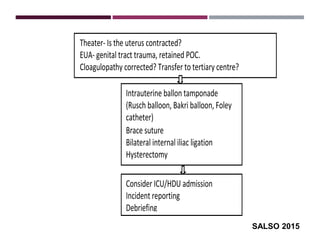
The document discusses postpartum haemorrhage (PPH), defining it as blood loss exceeding 500ml within 24 hours of delivery (primary PPH) or excessive bleeding from 24 hours to 6 weeks postpartum (secondary PPH). PPH is a leading cause of maternal death. Management involves simultaneous resuscitation, identification of cause such as uterine atony or trauma, and treatment including uterotonic drugs, balloon tamponade, or surgery. Early recognition, teamwork, and avoiding delays in care are essential to prevent mortality from massive PPH.