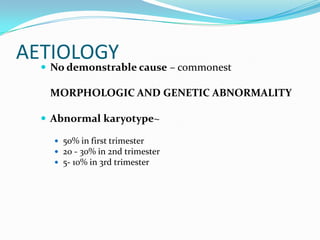
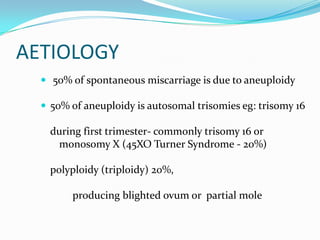
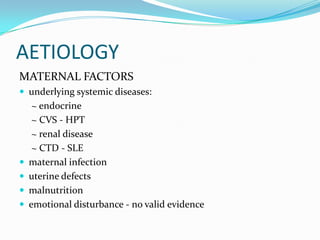
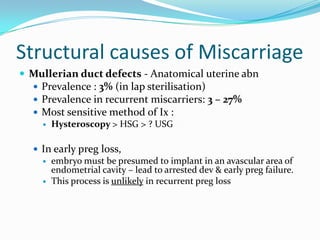
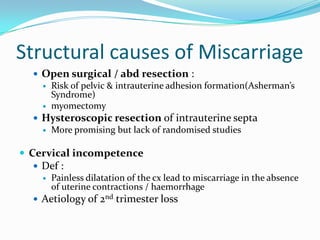
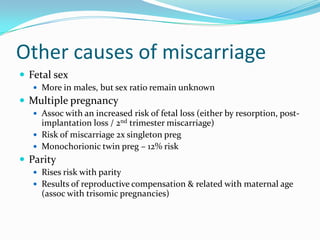
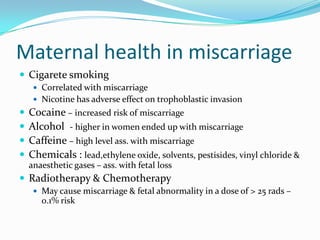
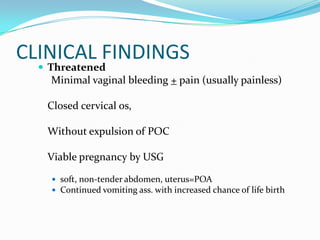
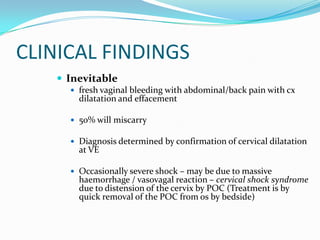
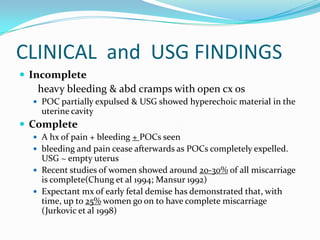
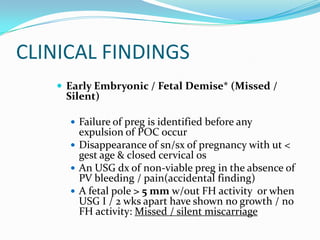
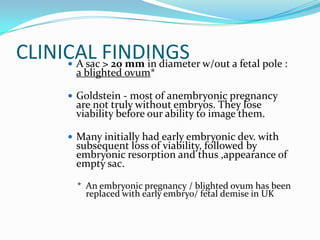
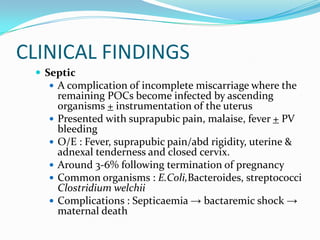
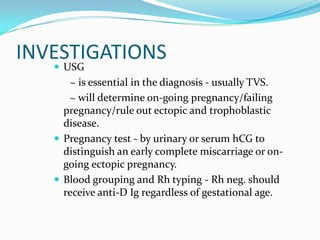
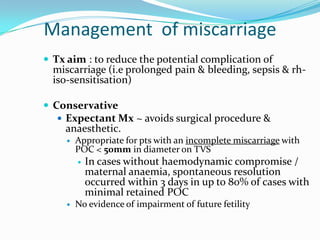
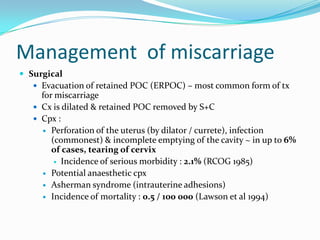
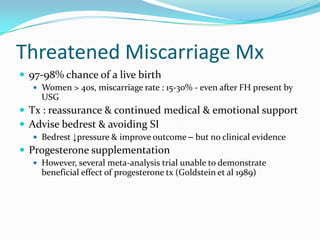
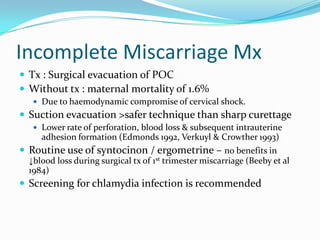
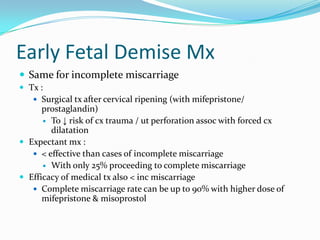
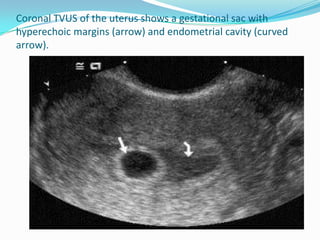
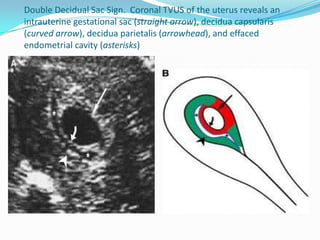
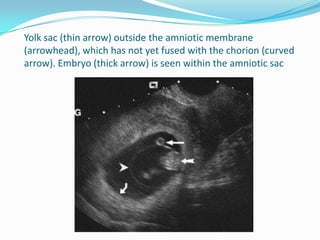
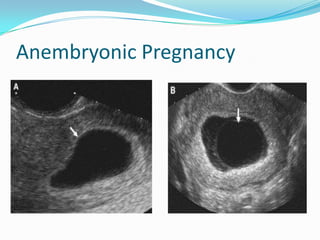
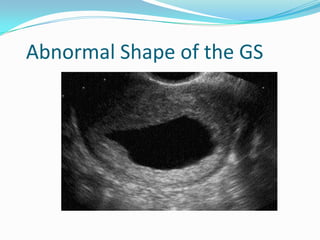
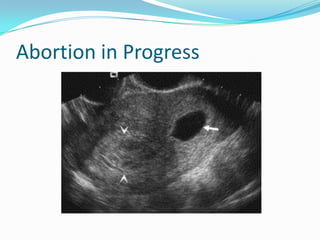
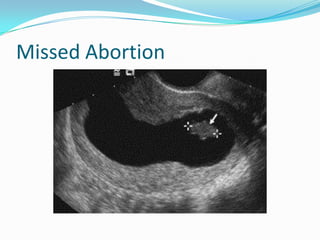
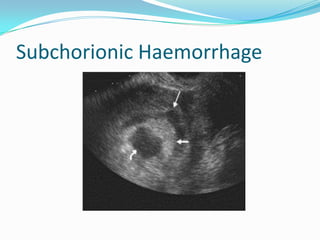
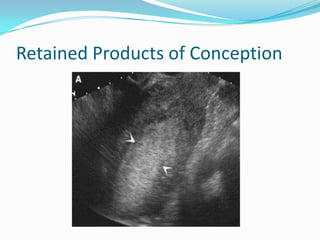
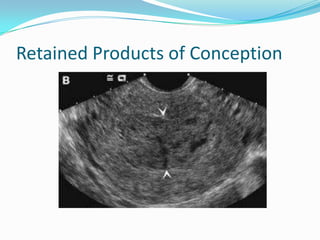
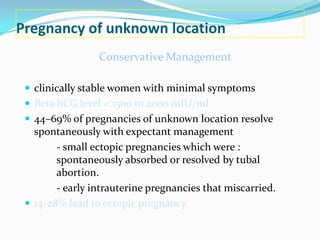
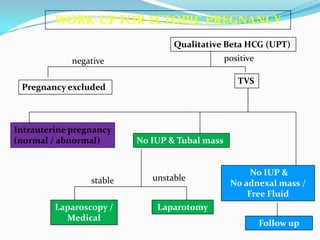
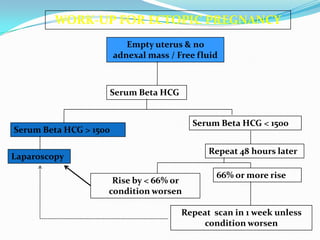
This document discusses miscarriage and related topics in obstetrics and gynecology. It defines different types of miscarriage such as threatened, inevitable, incomplete, and missed/silent miscarriage. It covers etiologies, risk factors, clinical presentations, investigations and management approaches for miscarriage. Key points include that 50% of spontaneous miscarriages are due to chromosomal abnormalities, infection is an unclear cause of recurrent miscarriage, and management involves either conservative expectant monitoring or surgical evacuation of retained products of conception.