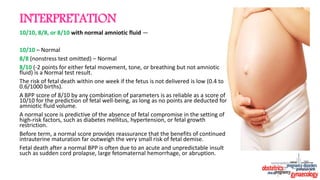
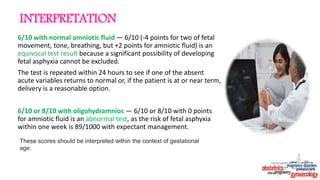
The document discusses the fetal biophysical profile (BPP), a noninvasive antepartum test that evaluates fetal well-being through ultrasound assessment of five parameters. A total BPP score of ≥8 indicates normal fetal health, while scores ≤4 suggest fetal compromise, prompting potential intervention. Various testing protocols, interpretation of scores, and factors affecting test results are outlined, demonstrating the BPP's role in antenatal care, particularly for high-risk pregnancies.




![DETERMINING THE BIOPHYSICAL PROFILE SCORE
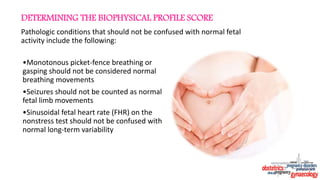
Assigning points — The composite BPP score is derived from five fetal parameters:
four acute parameters (heart rate accelerations in response to movement
[nonstress test], breathing movement, body and limb movement, tone) and one
chronic parameter (amniotic fluid volume).
Each of these five parameters has been evaluated independently with the
normal characteristic defined.
The scoring method used for each parameter is binary (ie, the parameter is
either normal or abnormal; gradations of abnormality are not used).
A normal parameter is assigned a score of 2 and an abnormal parameter is
assigned a score of 0.
The maximum score is 10/10 and the minimum score is 0/10.](https://image.slidesharecdn.com/biophysicalprofiledr-220801164721-5e682c4f/85/Biophysical-Profile-13-320.jpg)