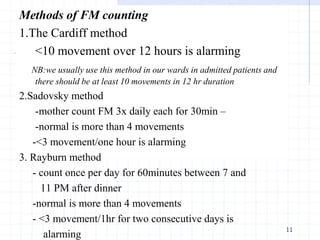
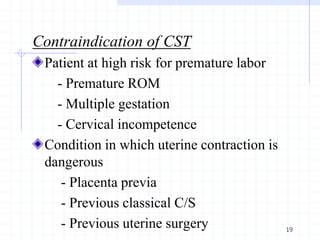
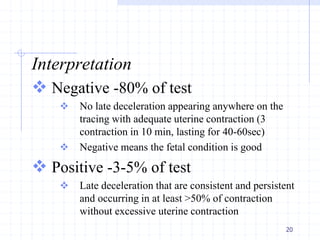
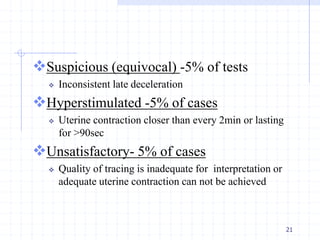
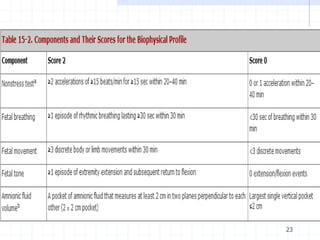
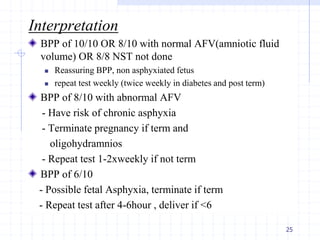
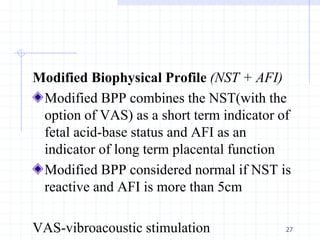
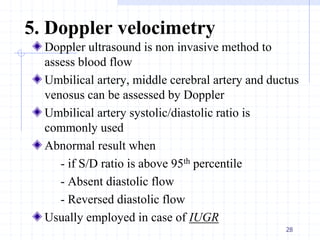
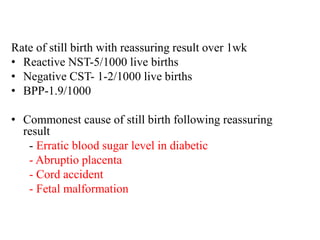
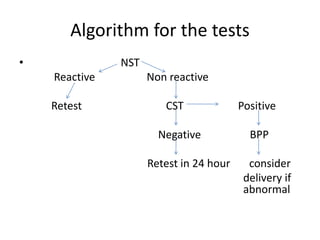
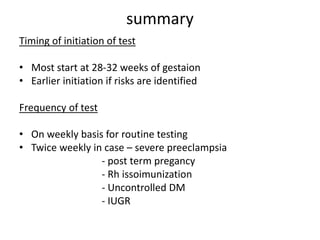
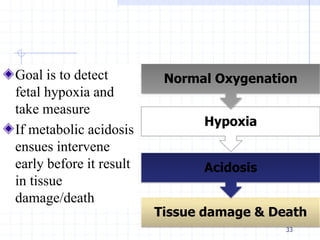
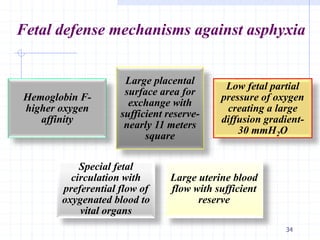
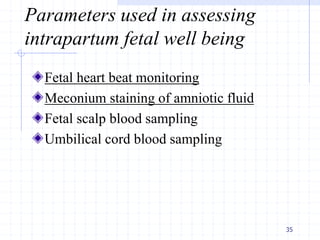
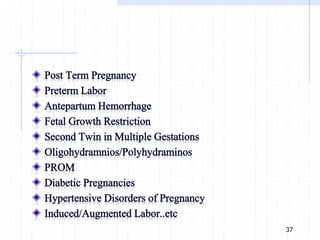
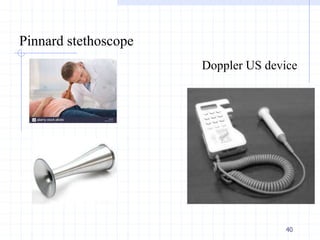
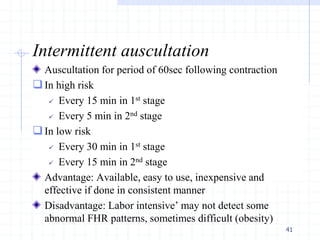
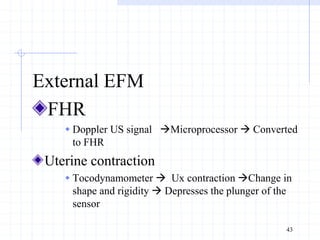
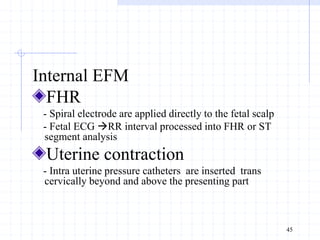
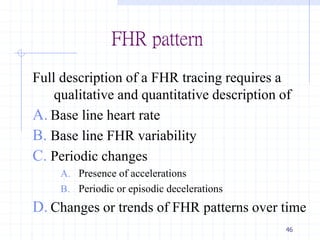
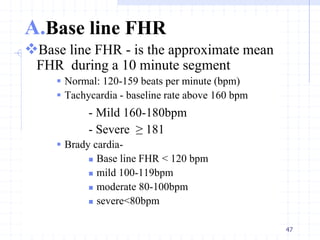
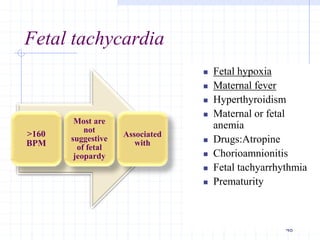
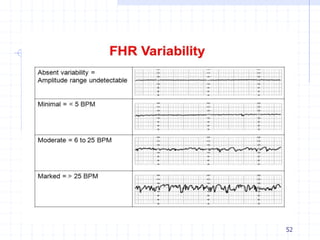
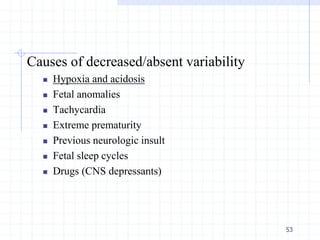
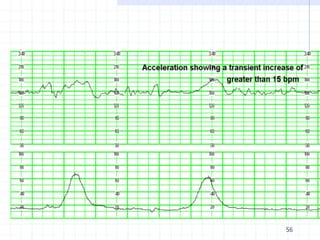
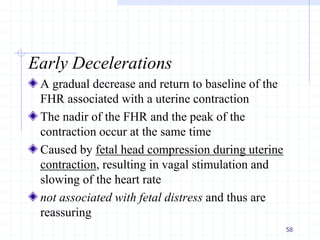
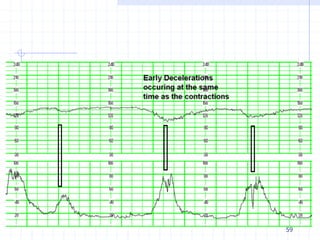
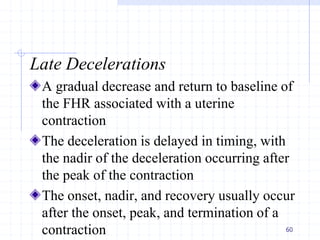
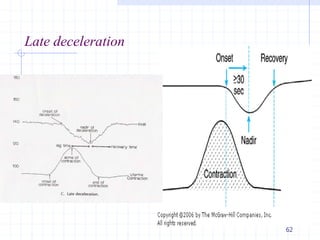
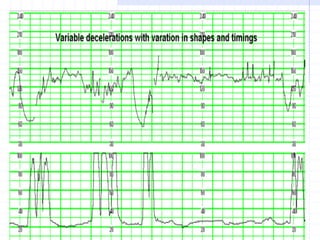
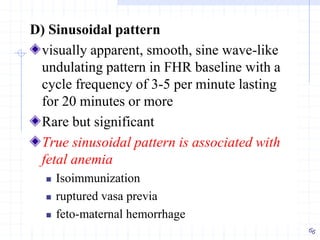
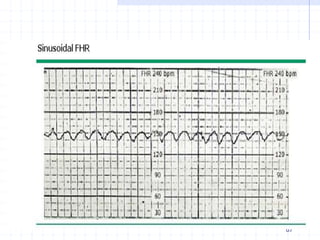
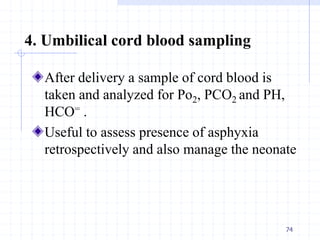
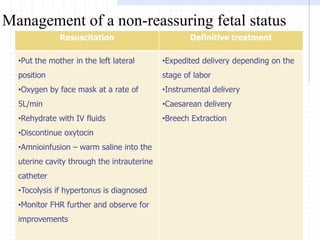
This document provides information on antepartum and intrapartum fetal surveillance. It discusses various testing modalities used in antepartum surveillance such as fetal movement counting, non-stress testing, biophysical profile, and Doppler velocimetry. It also describes parameters assessed in intrapartum surveillance including fetal heart rate monitoring patterns such as baseline rate, variability, accelerations, and decelerations. The goal of both antepartum and intrapartum surveillance is to detect fetal hypoxia and intervene early to prevent injury or death.