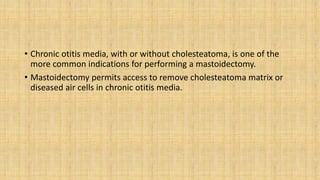
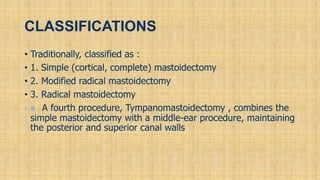
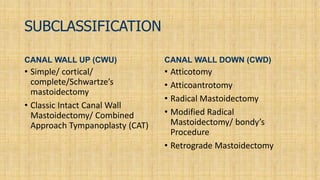
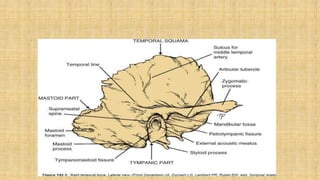
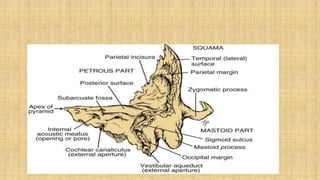
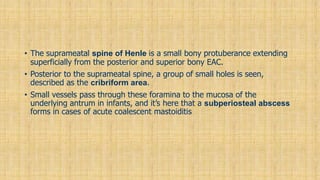
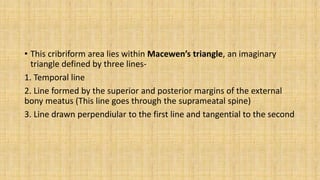
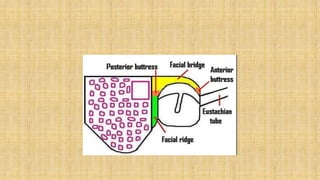
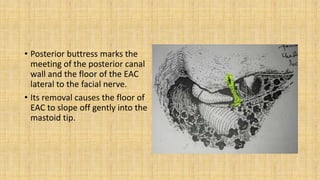
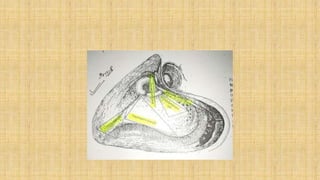
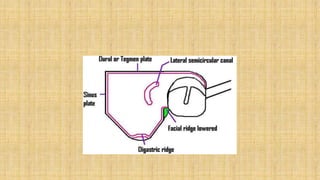
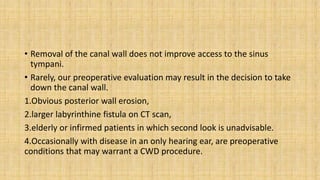
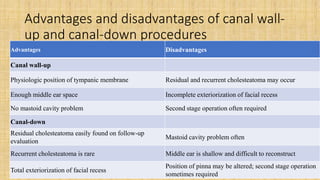
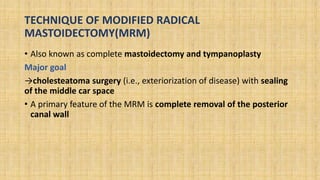
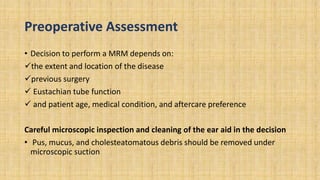
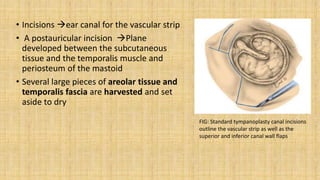
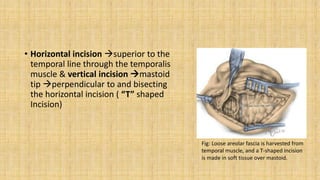
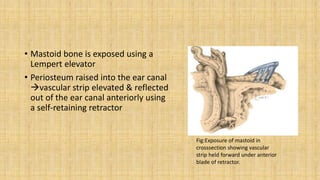
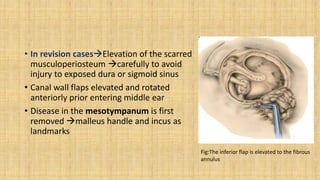
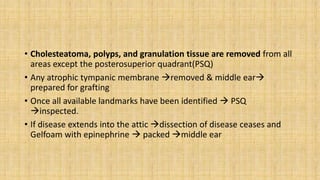
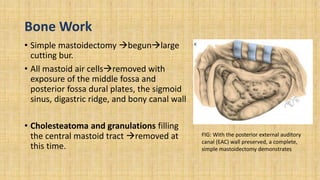
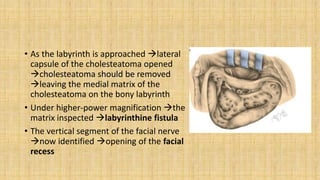
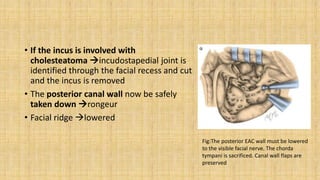
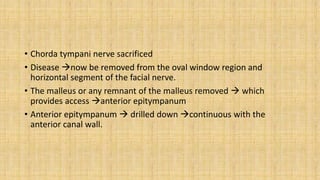
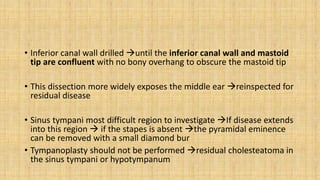
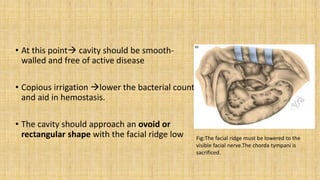
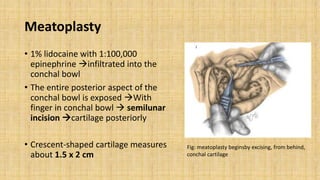
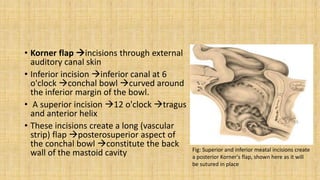
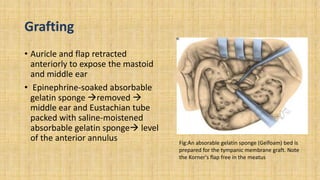
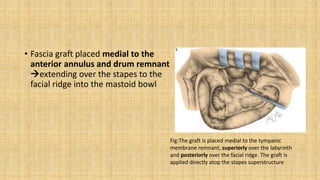
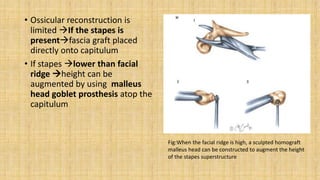
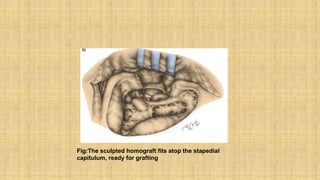
This document provides a history and overview of mastoid surgery. It discusses how mastoid surgery has evolved from simple procedures for acute infection to now focus on hearing preservation with techniques like intact canal wall mastoidectomy. It describes different types of mastoid surgeries including cortical mastoidectomy, radical mastoidectomy, modified radical mastoidectomy, and intact canal wall mastoidectomy. The document outlines the anatomical considerations for mastoid surgery and provides details on the technique for performing a modified radical mastoidectomy.