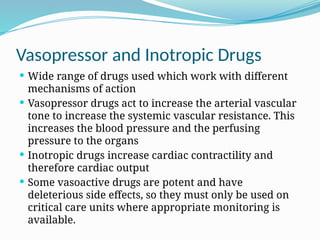
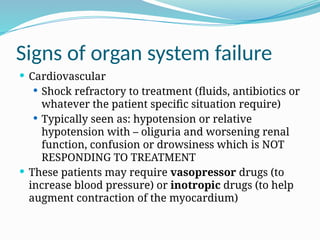
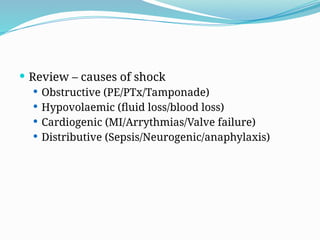
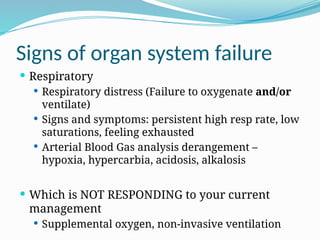
The document outlines the structure and functions of critical care units, including intensive care units (ICUs) and high dependency units (HDUs), focusing on their roles in monitoring and supporting patients with severe health issues. It discusses the multidisciplinary teams involved, indications for admission, and various organ support methods employed in intensive care. Additionally, it highlights the importance of early referral for patients with potentially recoverable conditions and reviews specific signs of organ system failure.


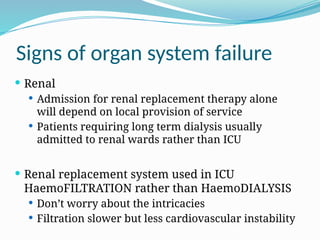
![ No Absolute indications for Haemofiltration but
potential indications include:
Hyperkalaemia [K+
] >6.5 mmol/l or rapidly rising
[K+
]
Suspected uraemic organ involvement
(pericarditis/encephalopathy/neuropathy/myopath
y
Urea >30mmol/L
Gross fluid overload
Clinically significant organ oedema (especially
lung)](https://image.slidesharecdn.com/criticalcareintroduction-250105125141-9aa21741/85/Critical-care-introduction-anesthesiology-15-320.jpg)