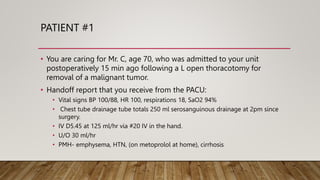
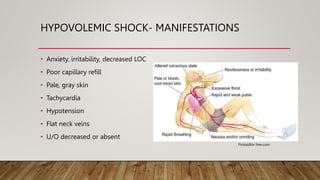
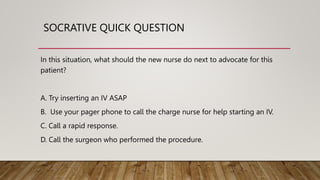
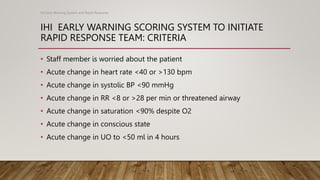
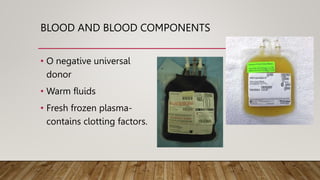
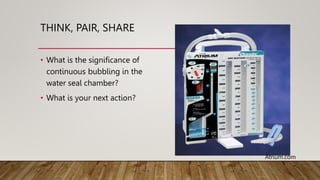
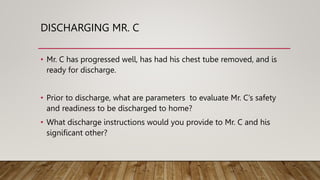
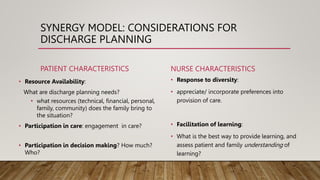
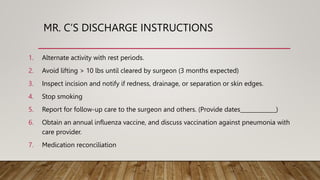
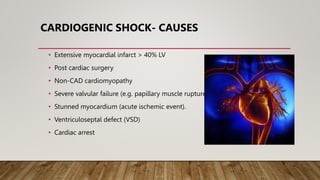
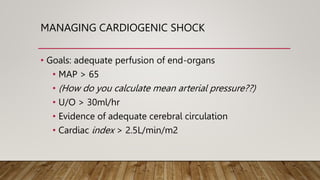
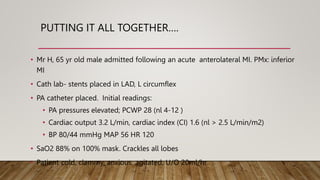
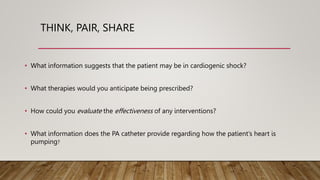
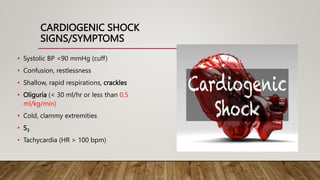
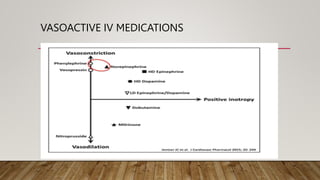
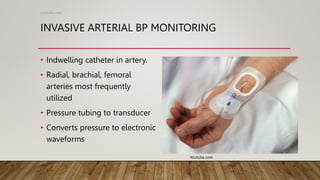
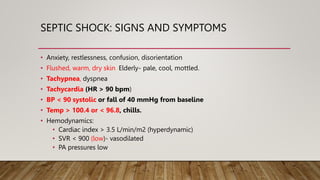
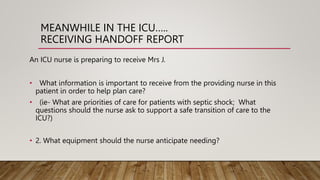
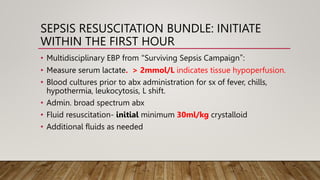
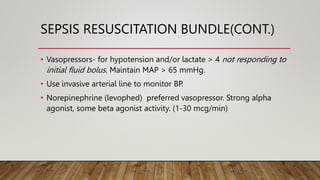
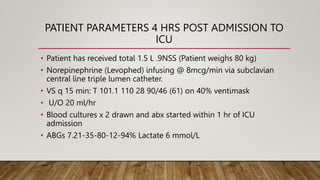
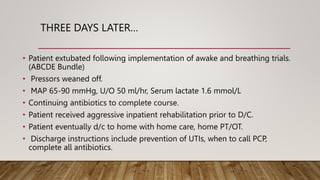
The document provides 3 case studies on different types of shock: hypovolemic shock from blood loss after surgery, cardiogenic shock following a heart attack, and septic shock from an untreated urinary tract infection. Each case study outlines the patient's presentation, relevant medical history, assessments, diagnostic findings, and shock management including fluid resuscitation and vasoactive medications. The goal is for students to apply their knowledge of shock pathophysiology and management using a case study approach.