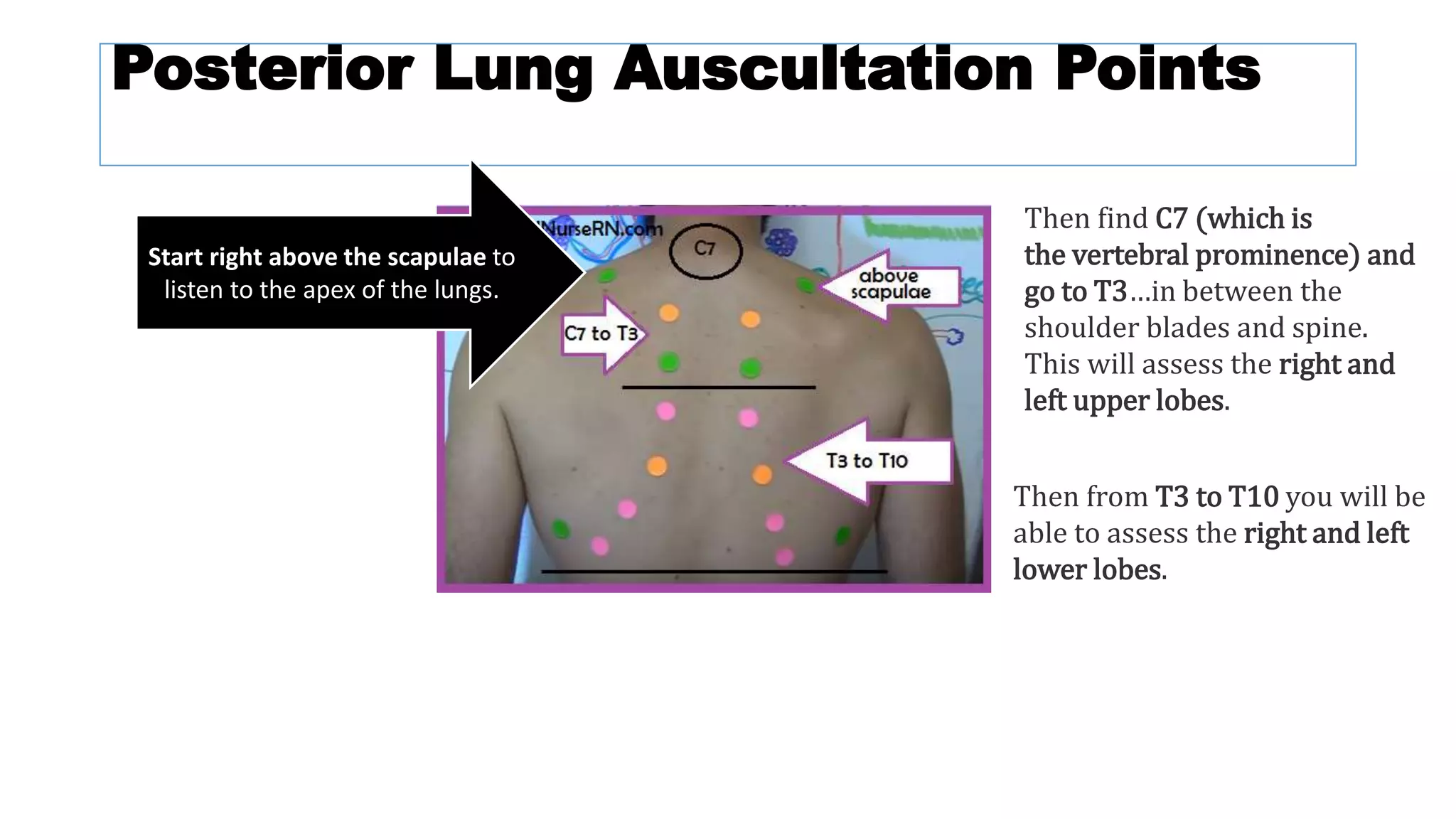
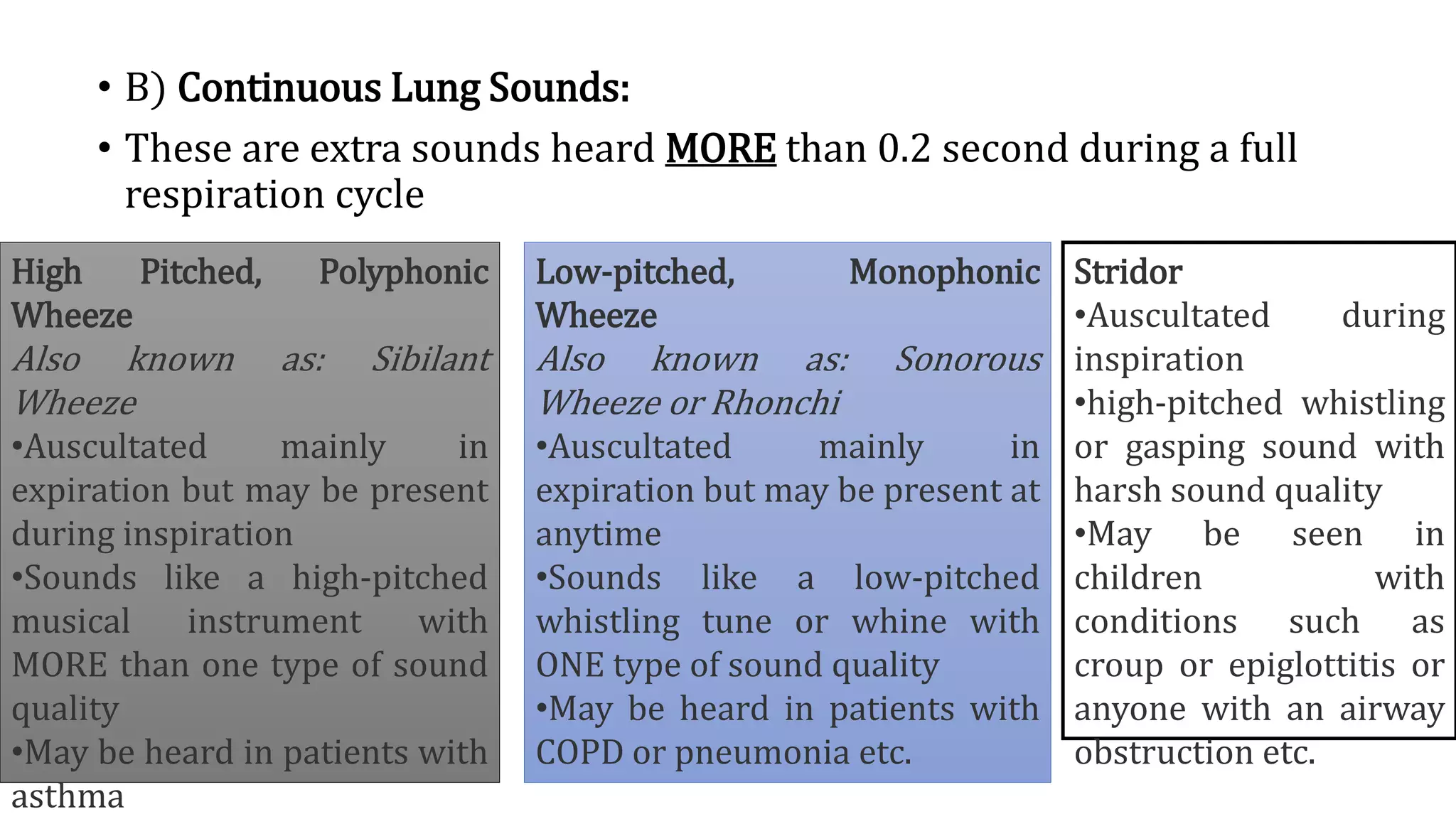
The document provides an overview of auscultation techniques for lung and heart examination using a stethoscope. It details the anatomy of lungs, common lung sounds and their identification, as well as heart sounds and their auscultation points. The document also describes adventitious sounds, heart murmurs, and basic principles for performing these assessments effectively.