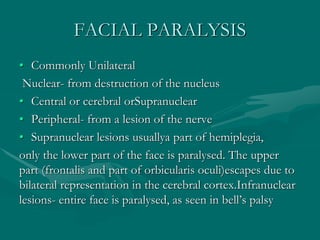
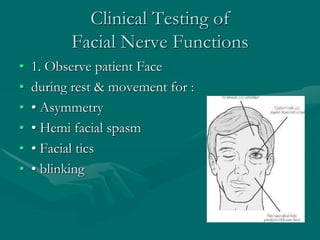
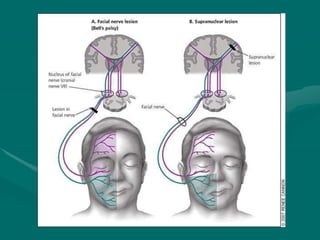
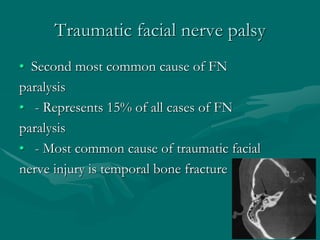
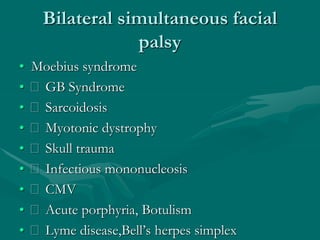
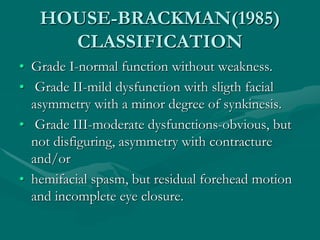
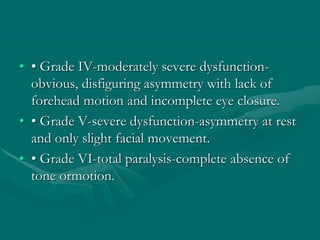
Facial palsy, or facial paralysis, can be caused by lesions of the facial nerve that disrupt motor function on one side of the face. It is commonly unilateral and can result from various etiologies like Bell's palsy, tumors, trauma, or infections. Clinical features include weakness or paralysis of facial muscles on the affected side leading to issues like eyelid drooping, inability to fully close the eye, and drooping of the mouth corner. Treatment involves facial exercises and in severe cases, surgery or implants may help restore more natural movement. Prognosis is generally good with many cases recovering normal function, but some are left with minor to severe long-term weakness or contractures.