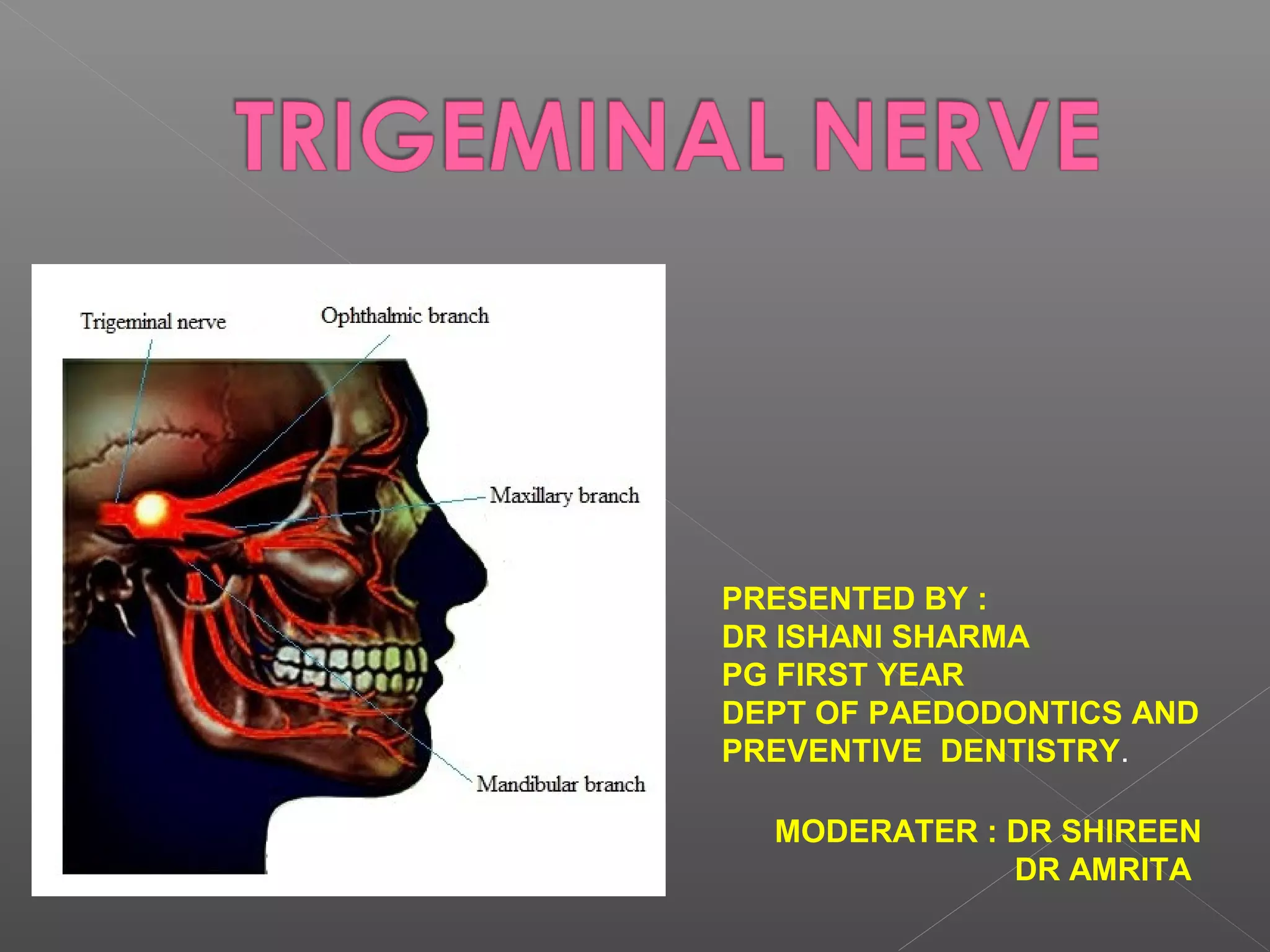
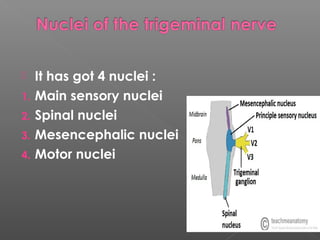
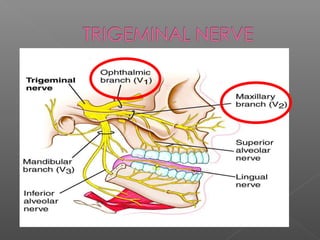
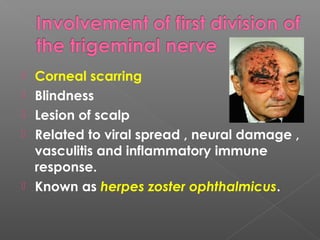
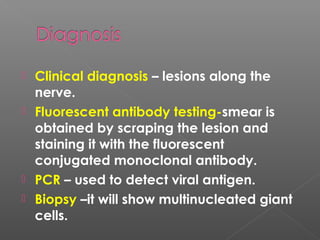
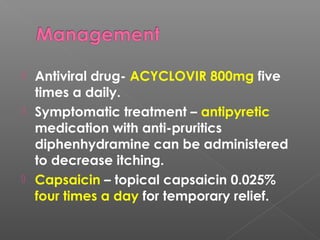
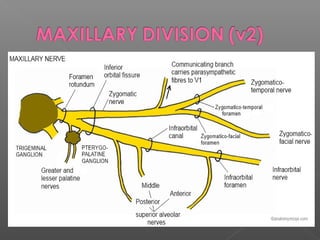
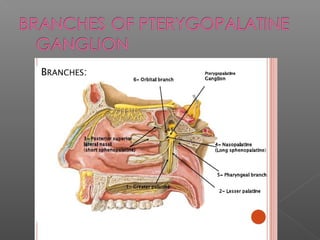
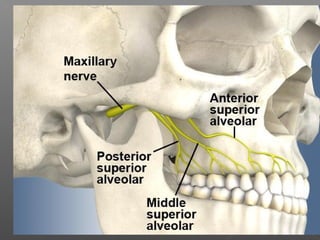
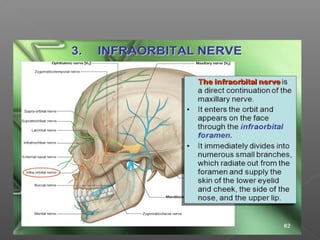
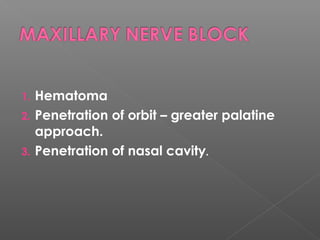
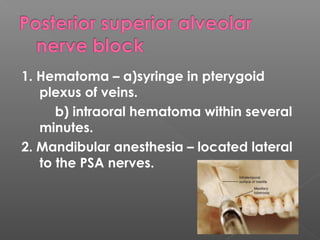
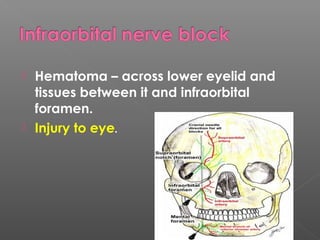
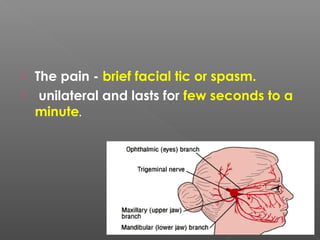
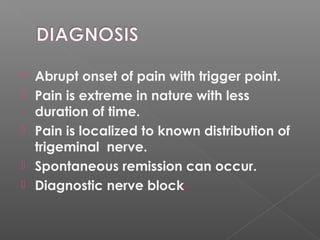
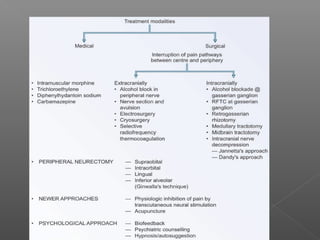
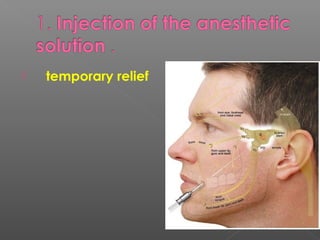
The document summarizes a presentation on the trigeminal nerve. It begins with an introduction and overview of topics to be covered, including the embryology, nuclei, ganglion, branches, and complications of nerve blocks of the trigeminal nerve. The presentation then discusses the anatomy and clinical features of trigeminal neuralgia, including symptoms, risk factors, diagnosis, and treatment options like medications and nerve blocks. The summary concludes by noting the applied anatomy of the trigeminal nerve and complications that can arise from nerve blocks.