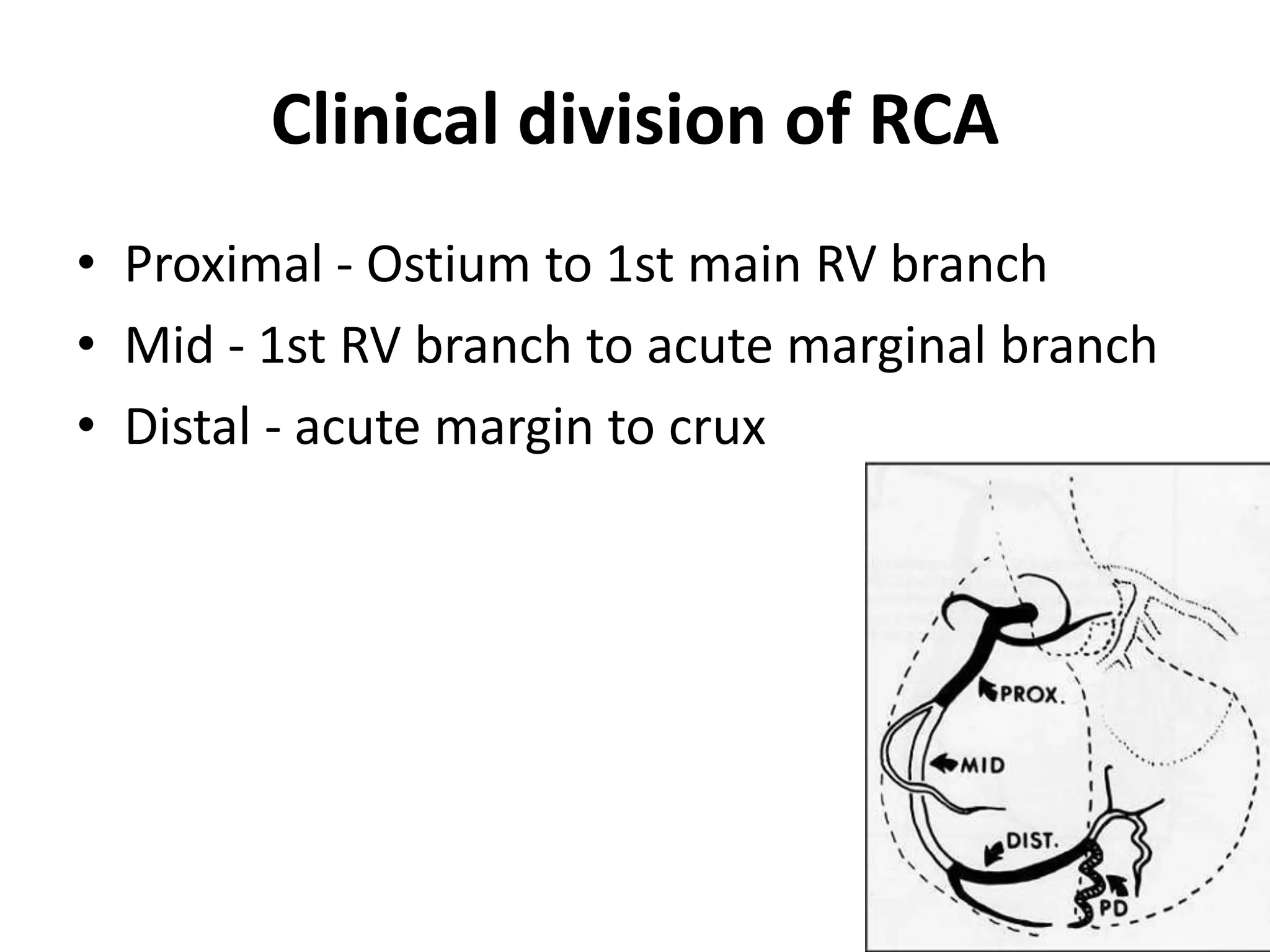
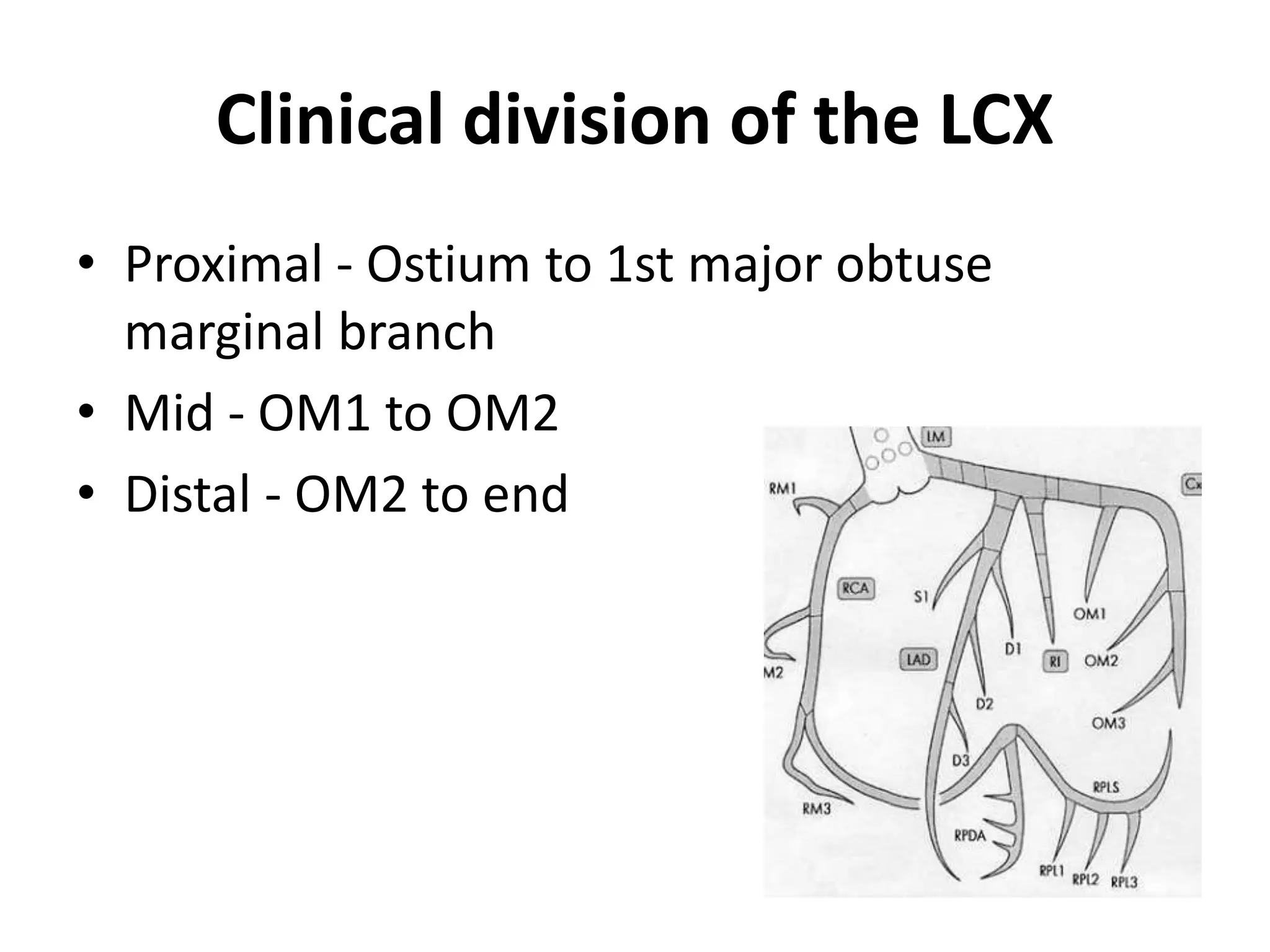
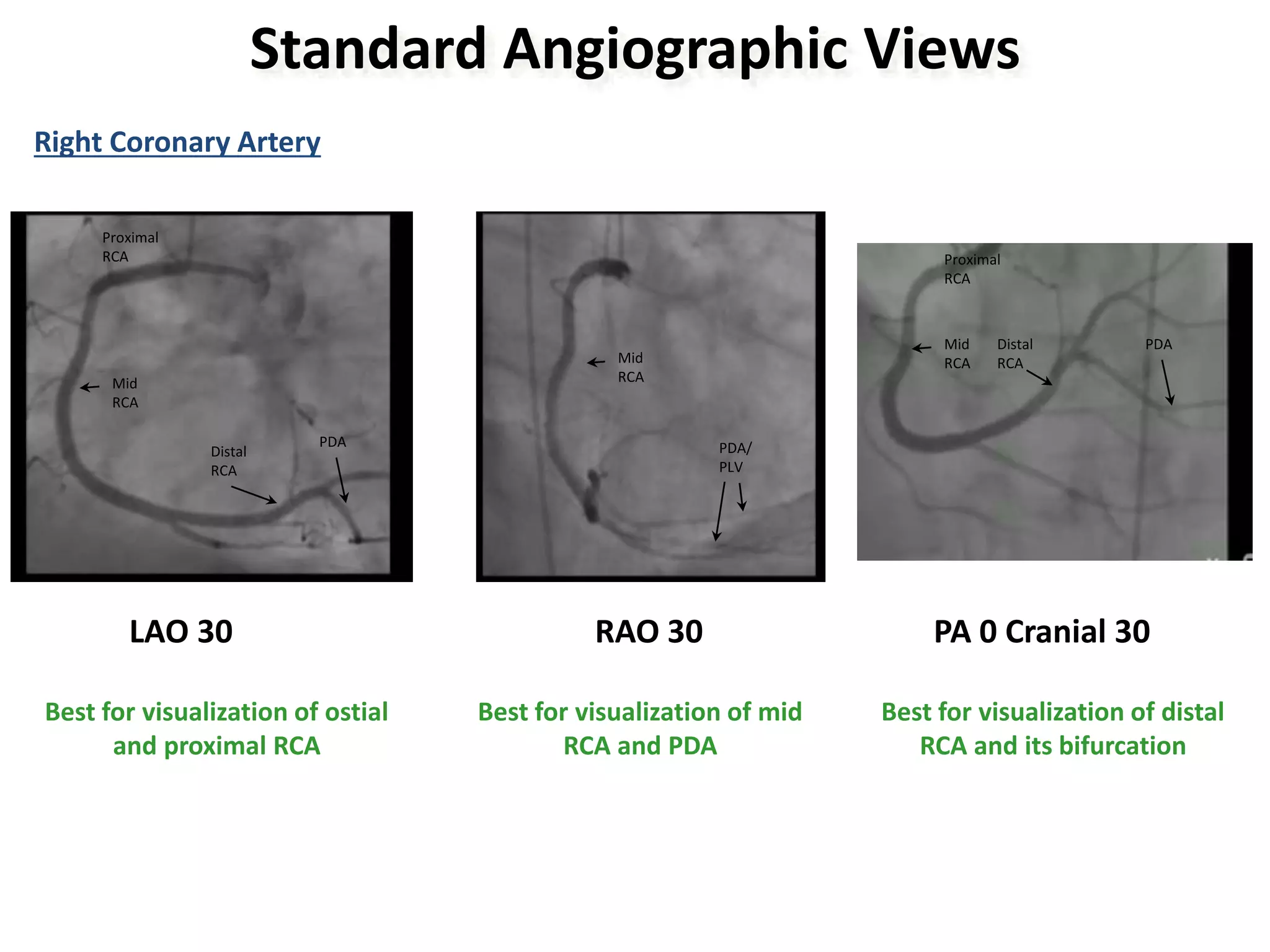
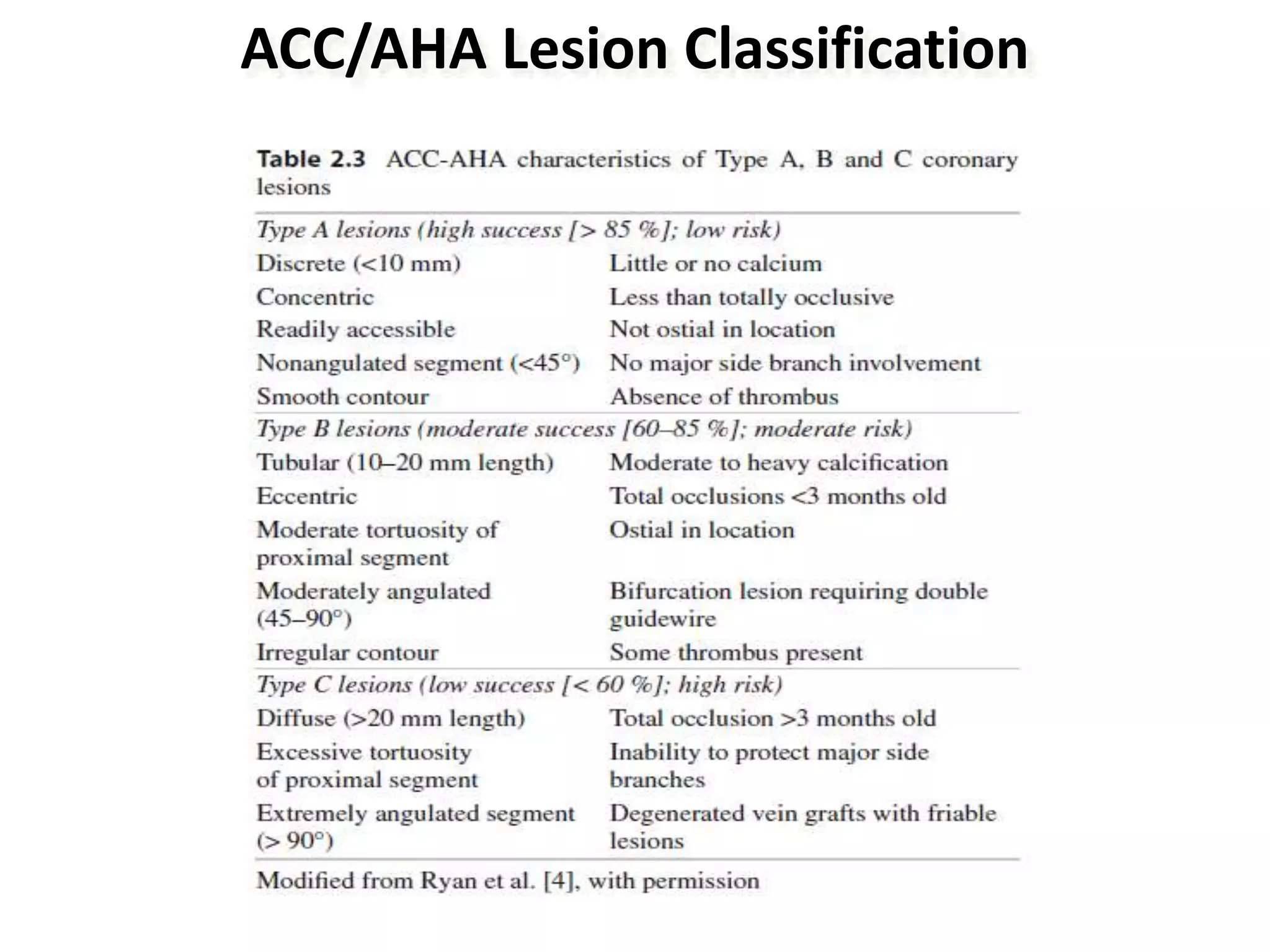
This document provides information on coronary angiography views and angiographic anatomy. It discusses the clinical divisions of the major coronary arteries and defines what constitutes significant coronary artery disease. Standard angiographic views are described for visualizing different segments of the left and right coronary arteries. Lesion classification systems and other angiogram interpretation elements like TIMI frame count are also summarized.