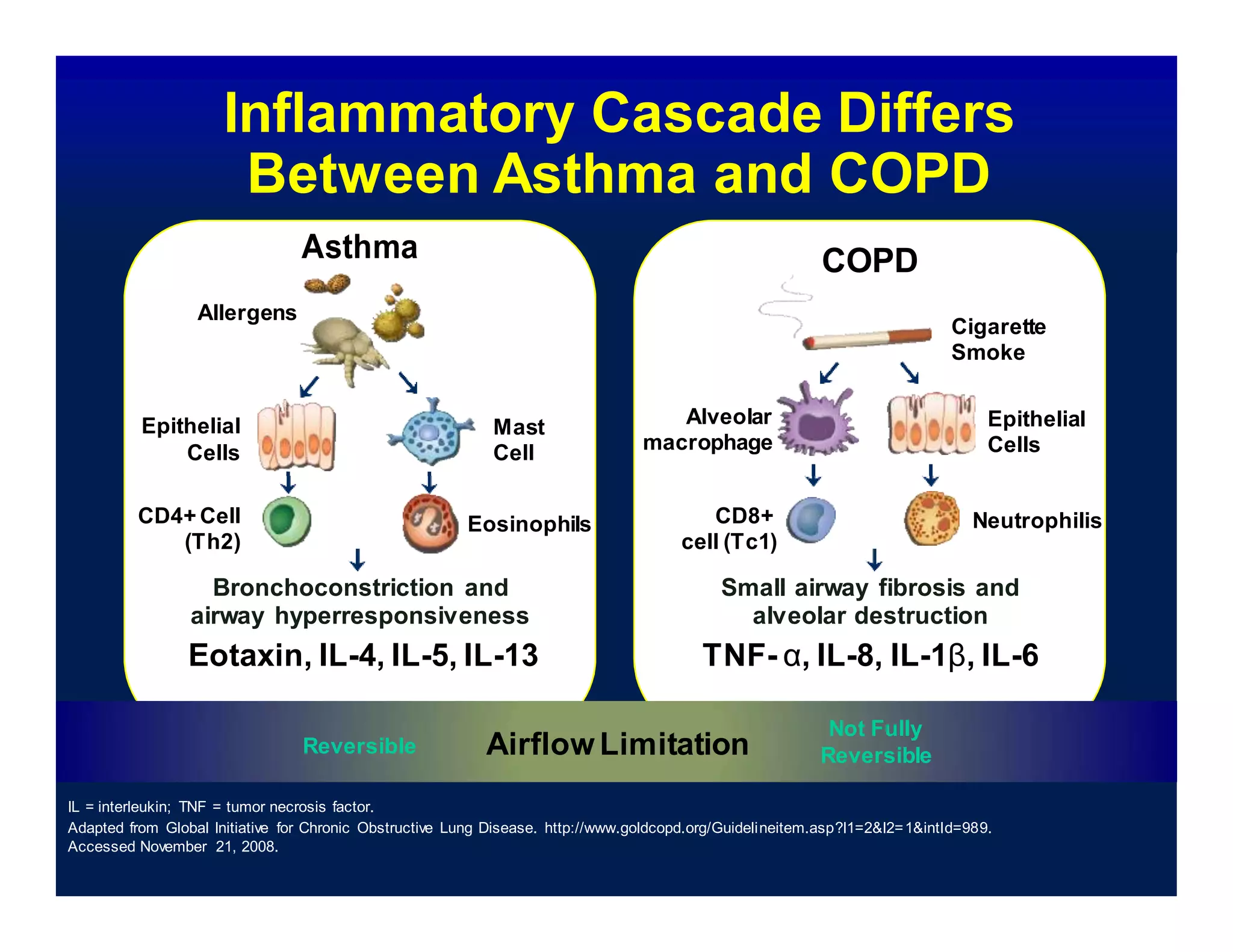
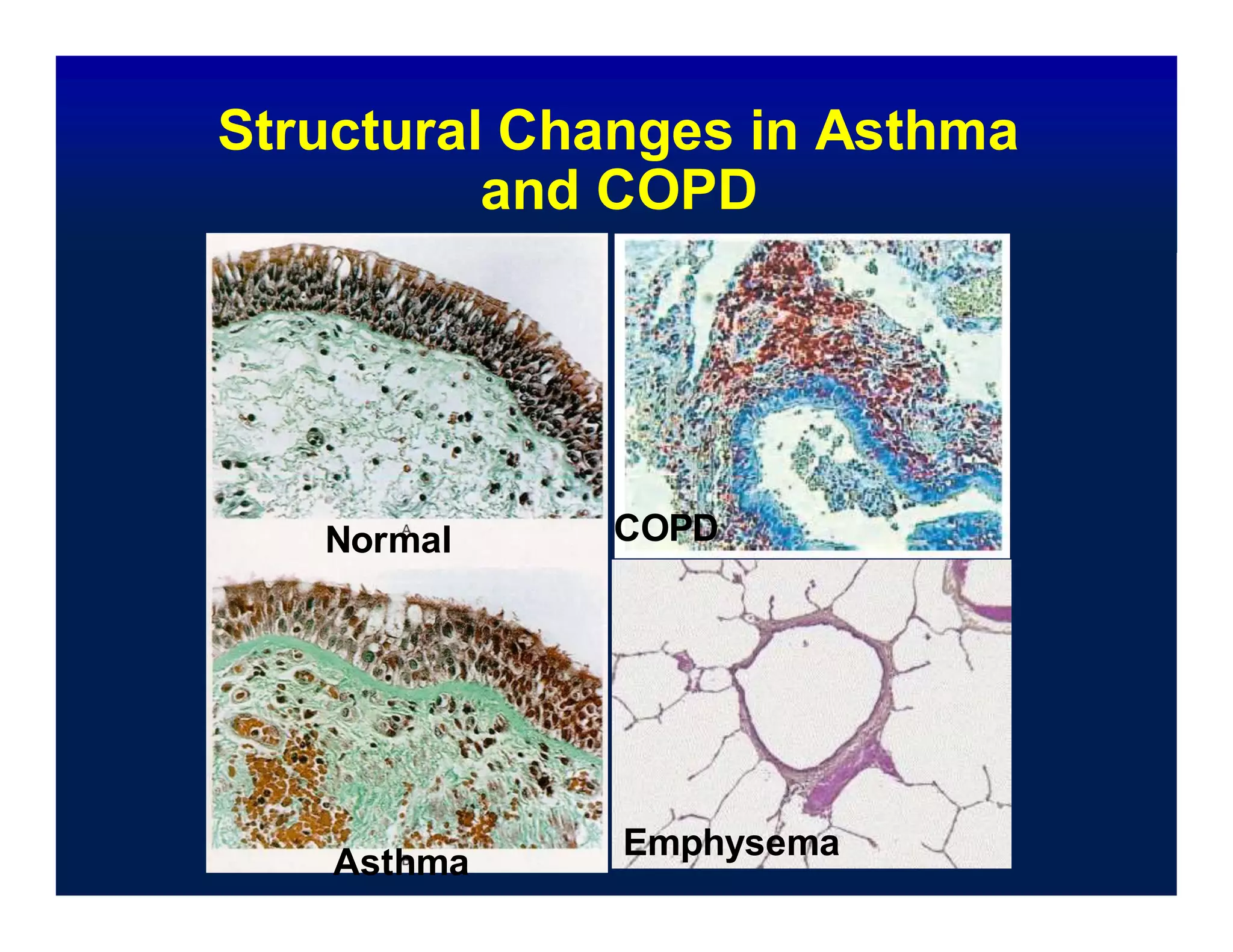
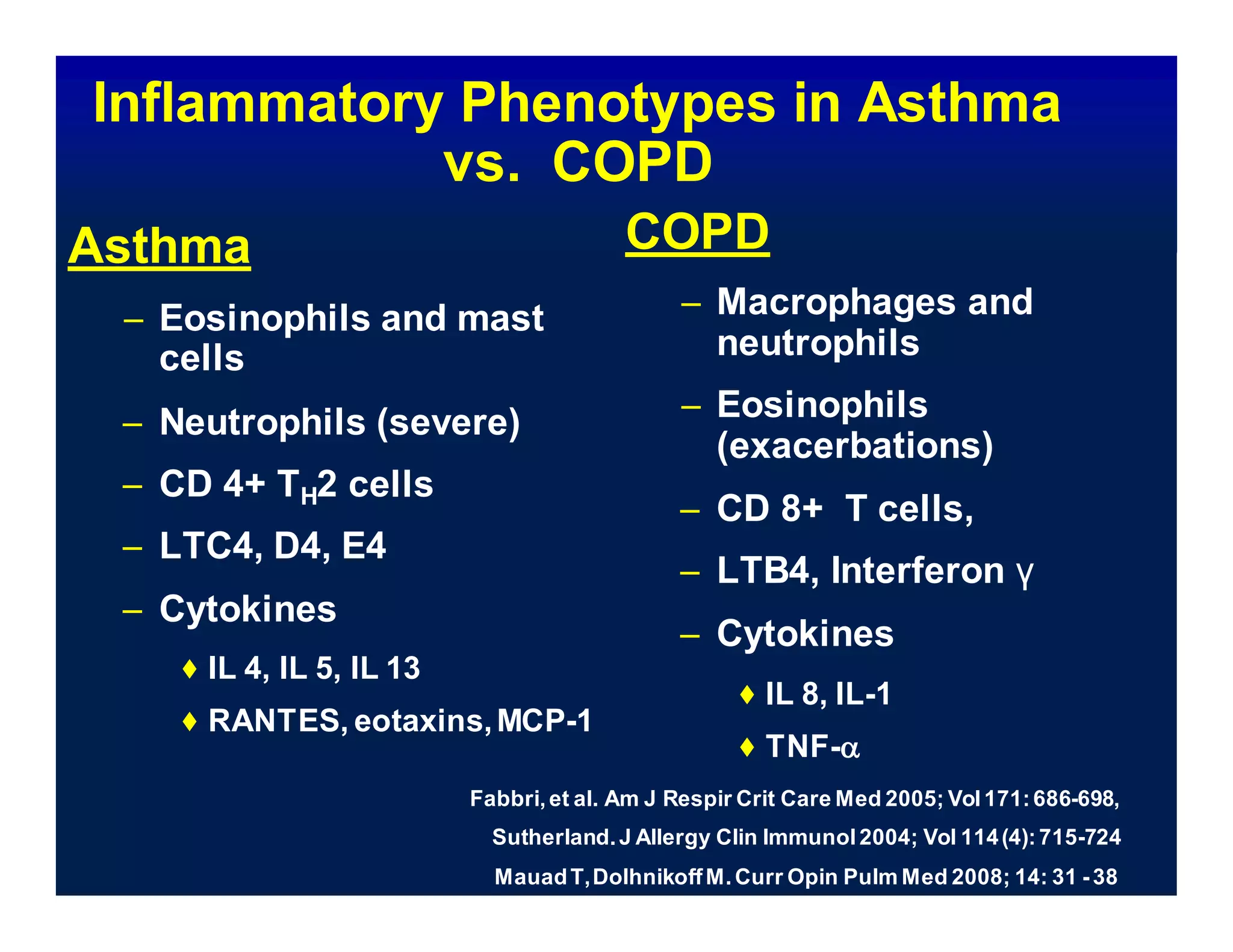
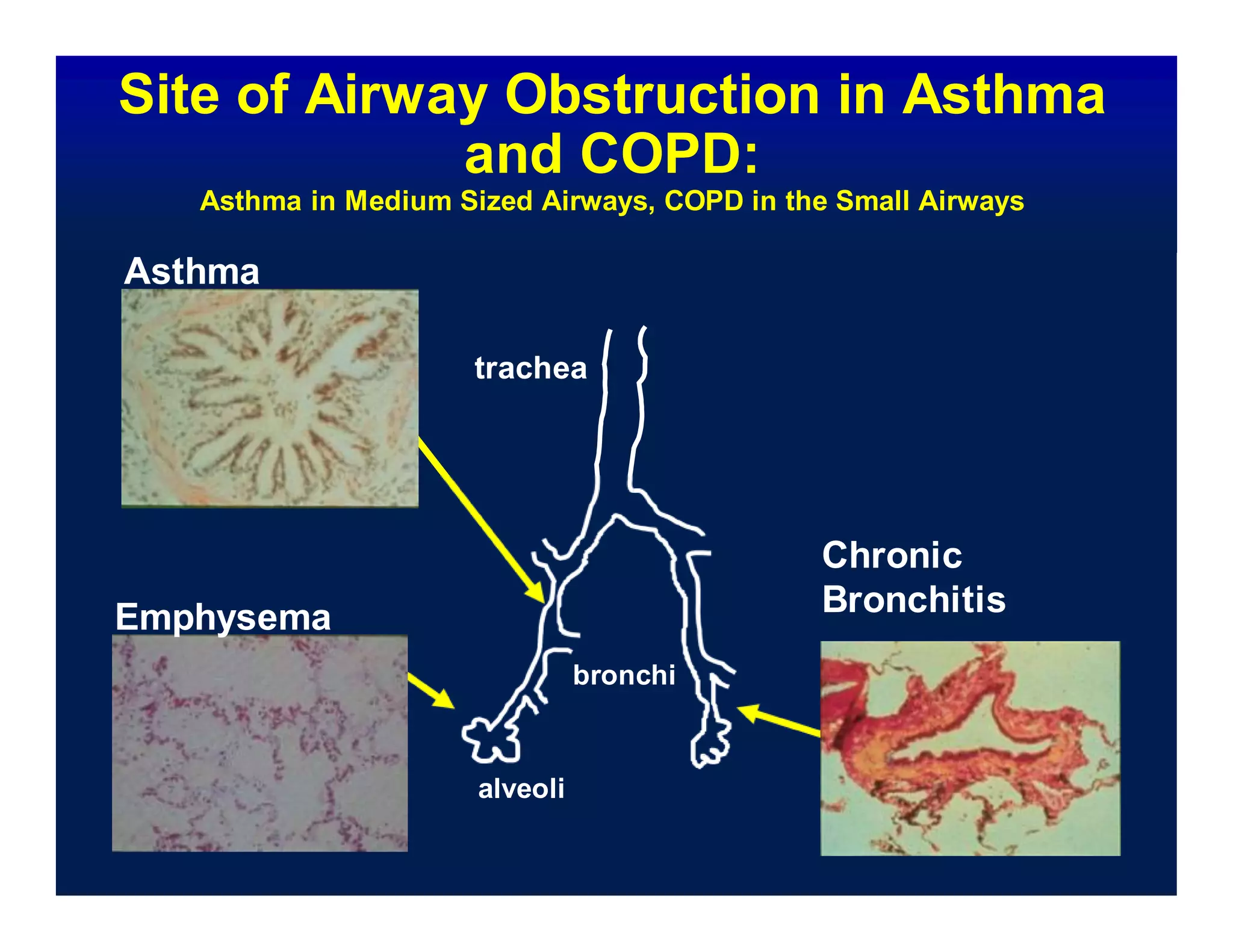
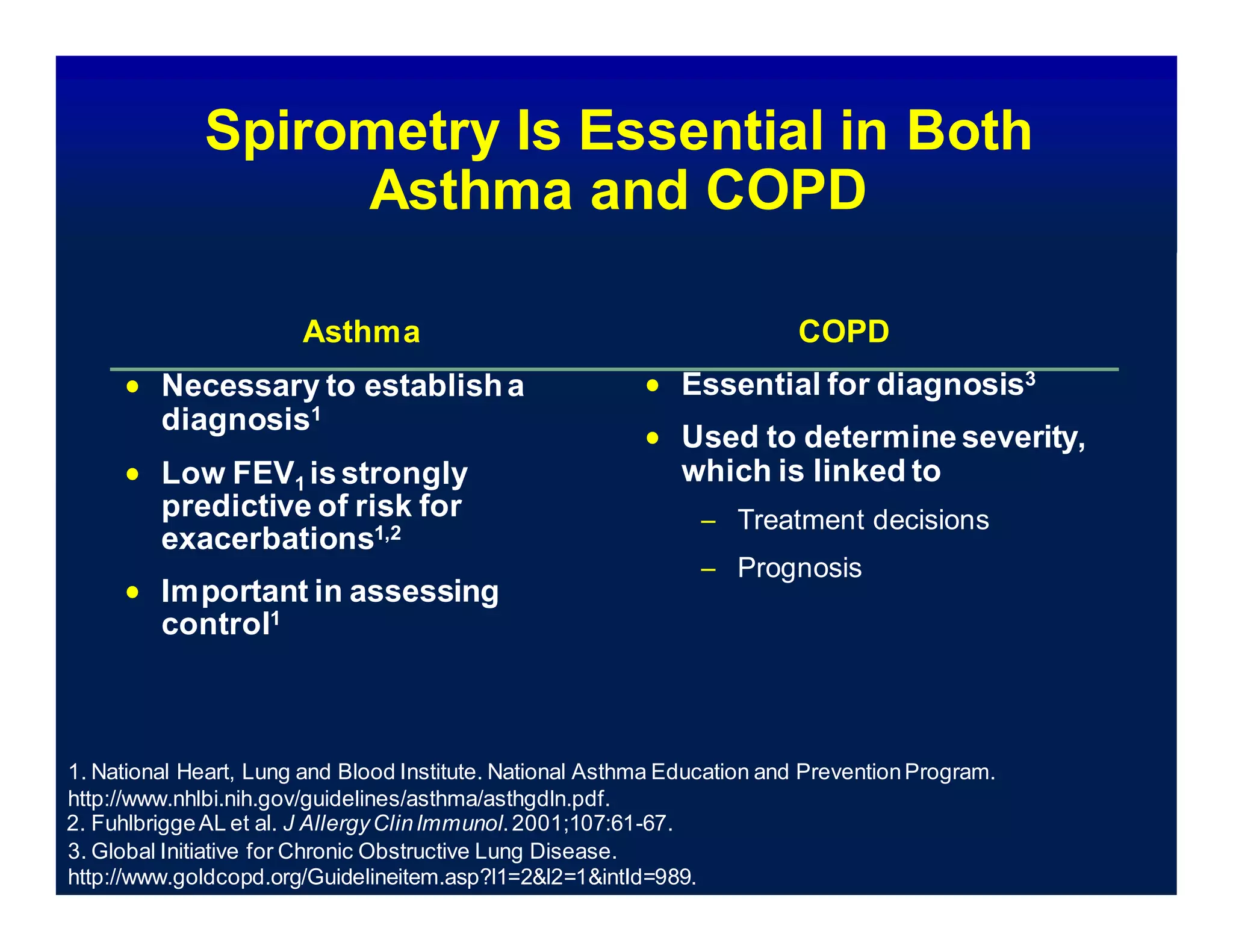
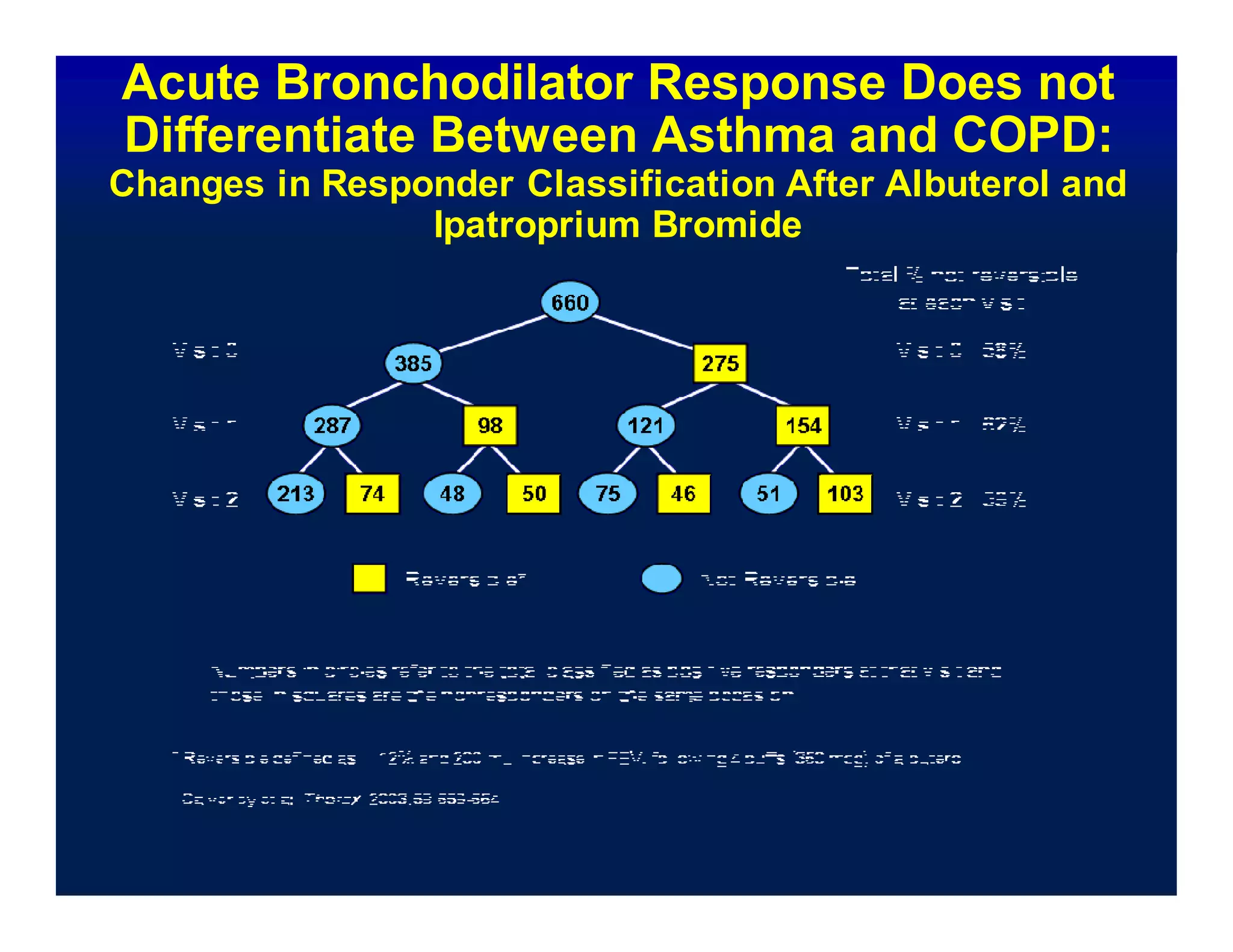
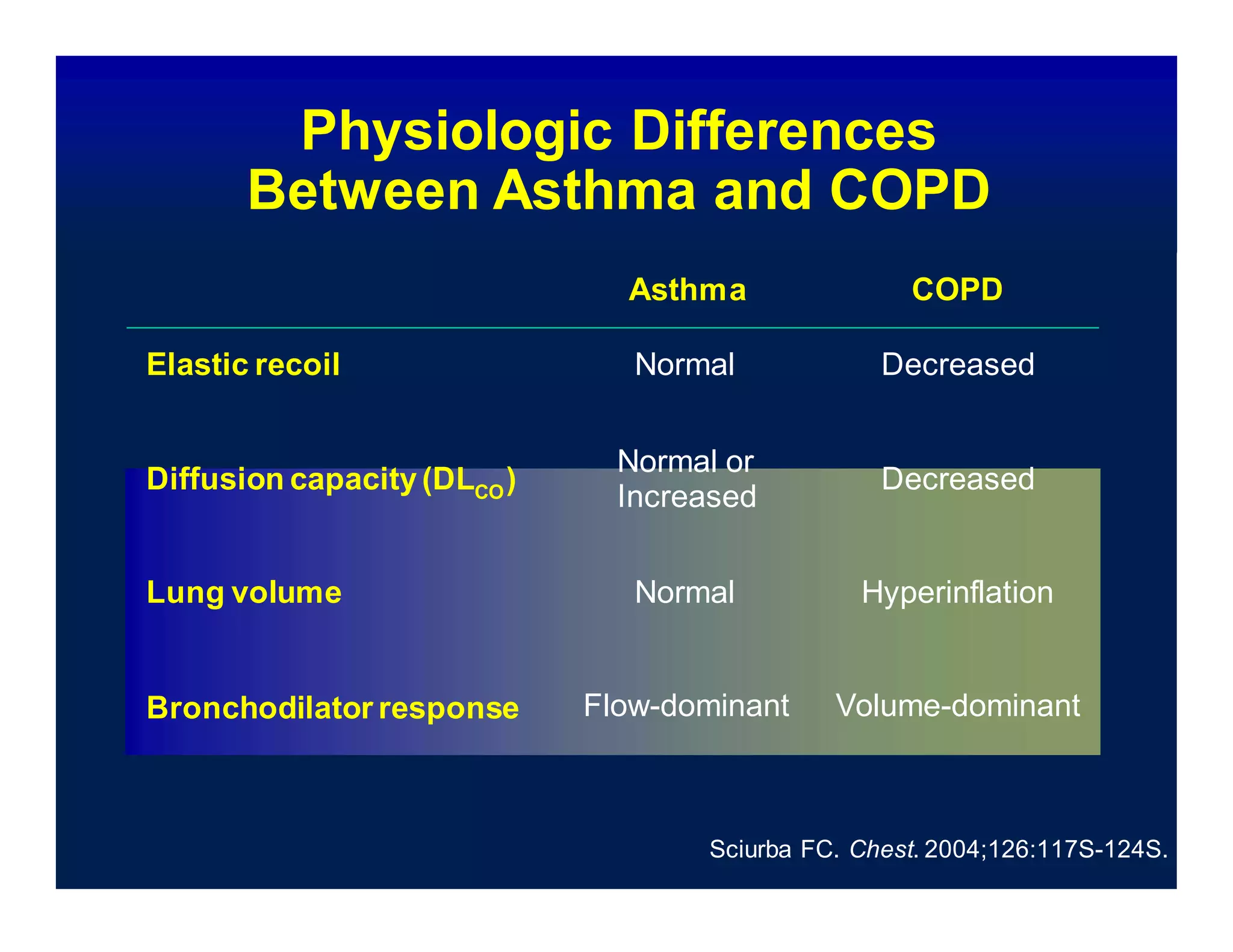
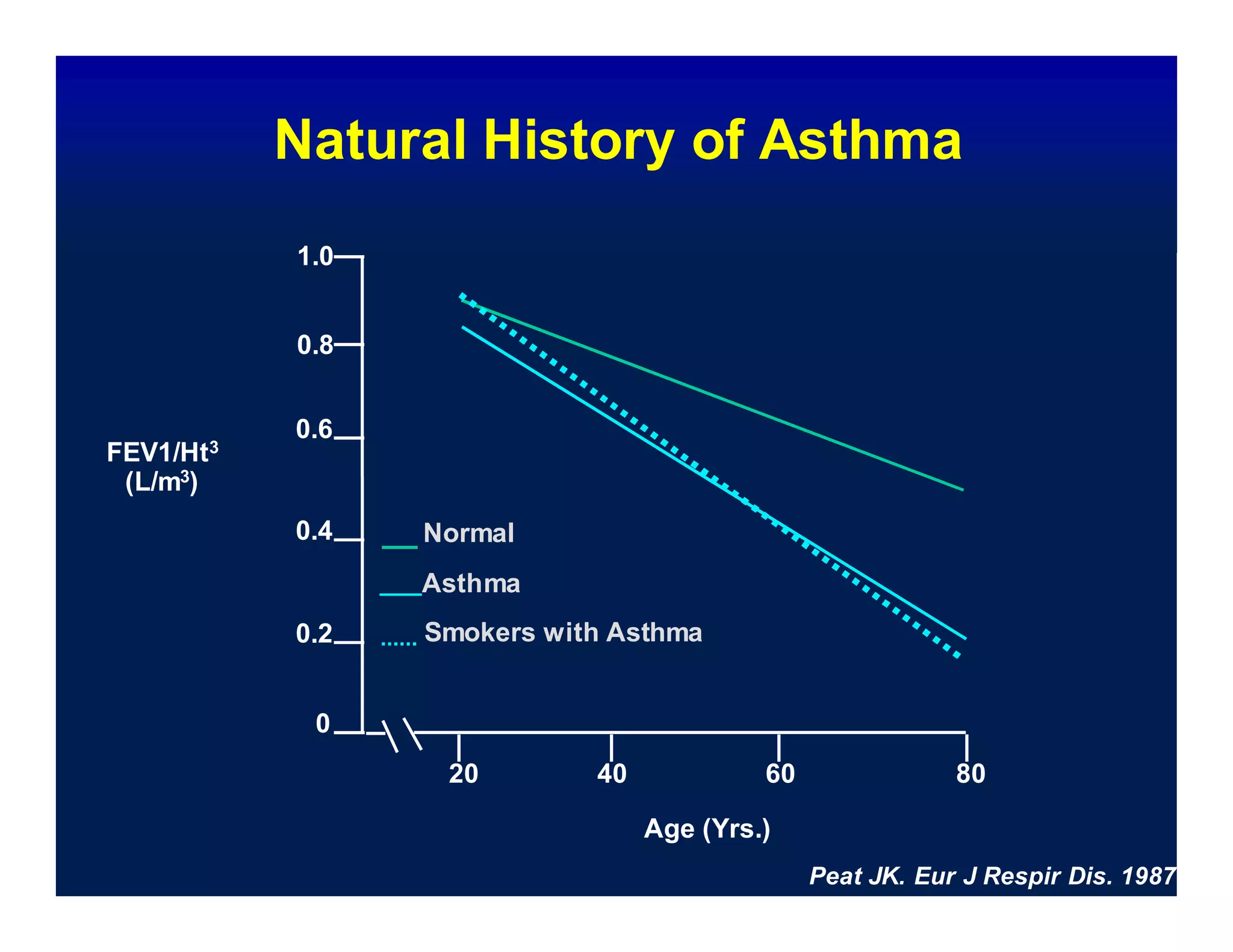
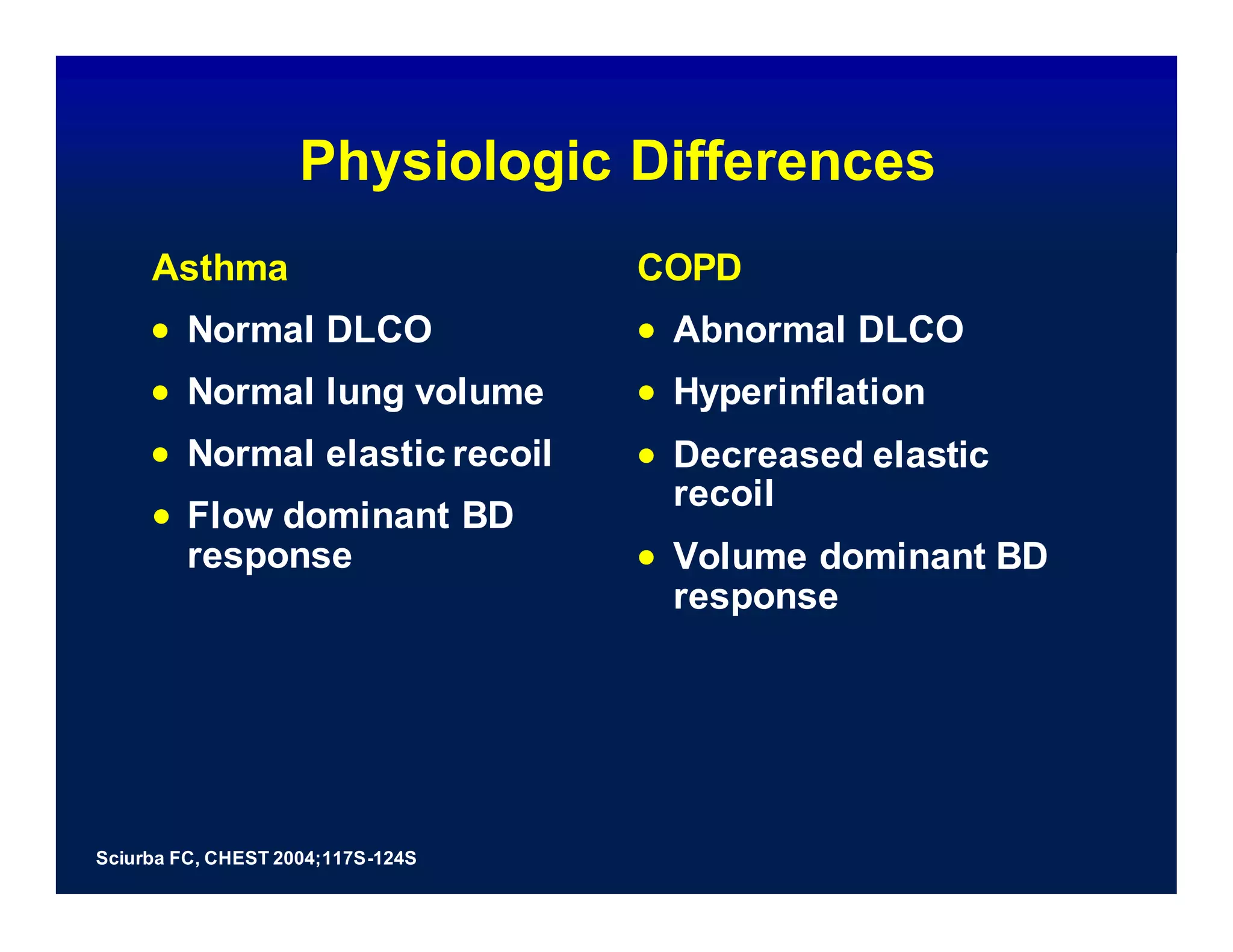
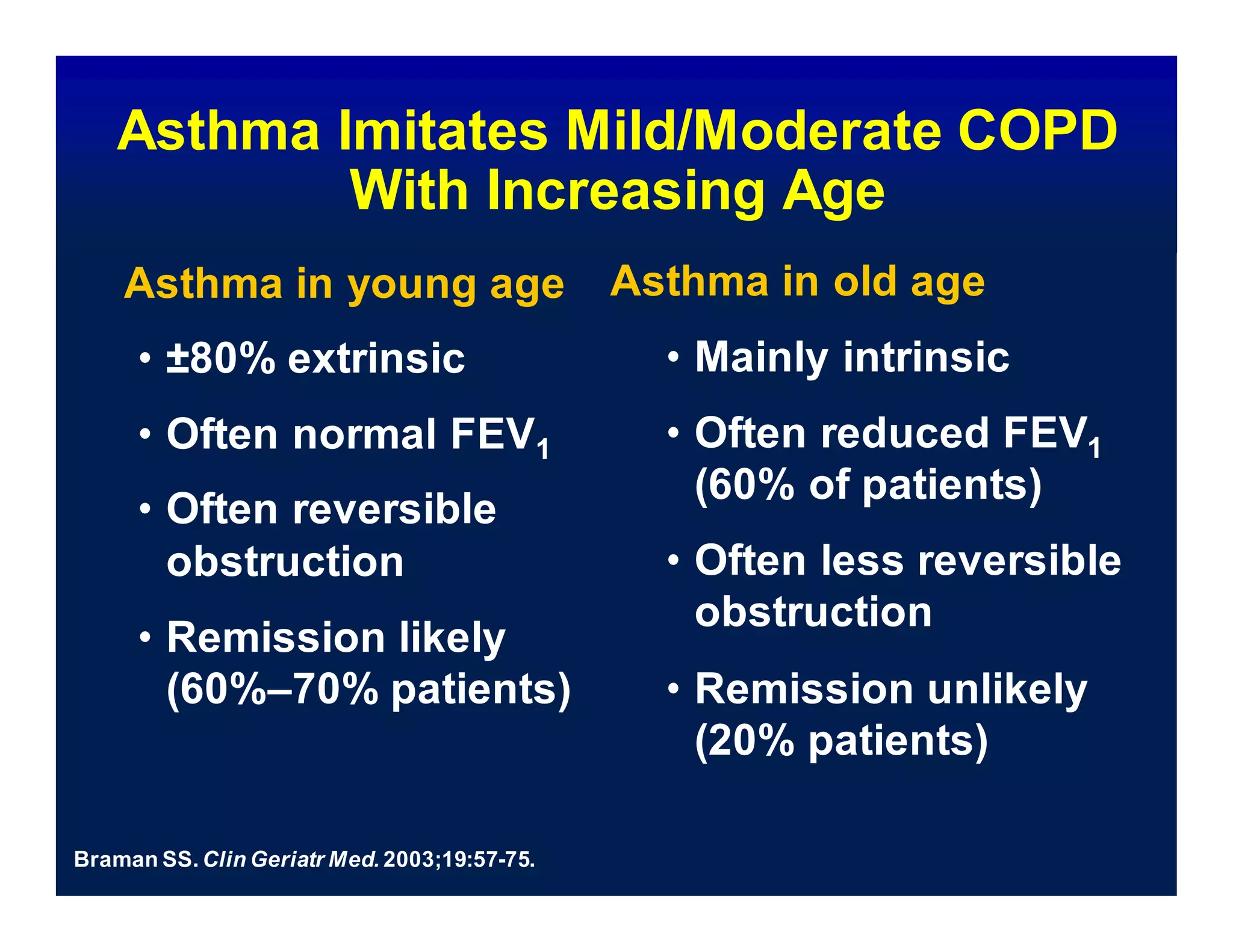
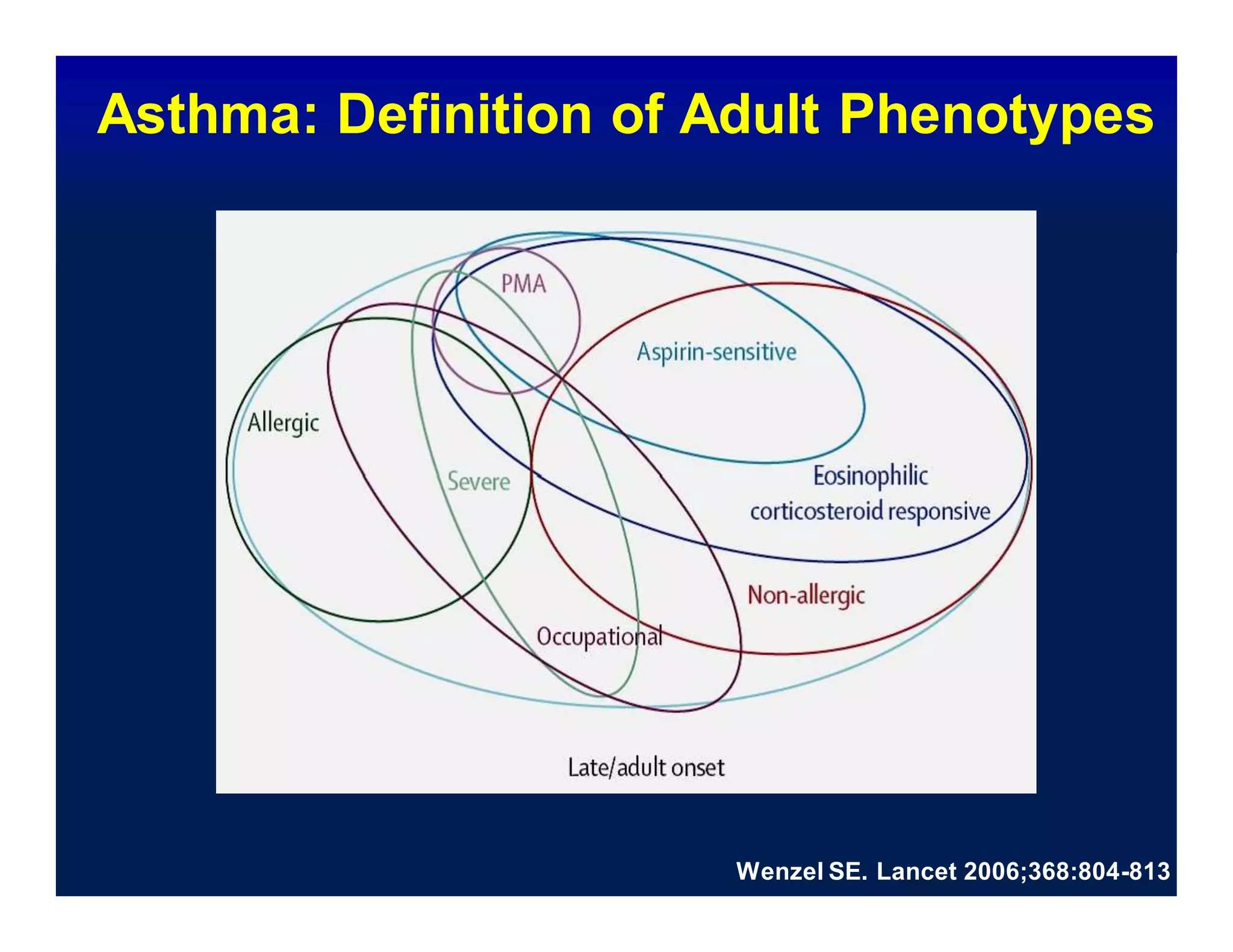
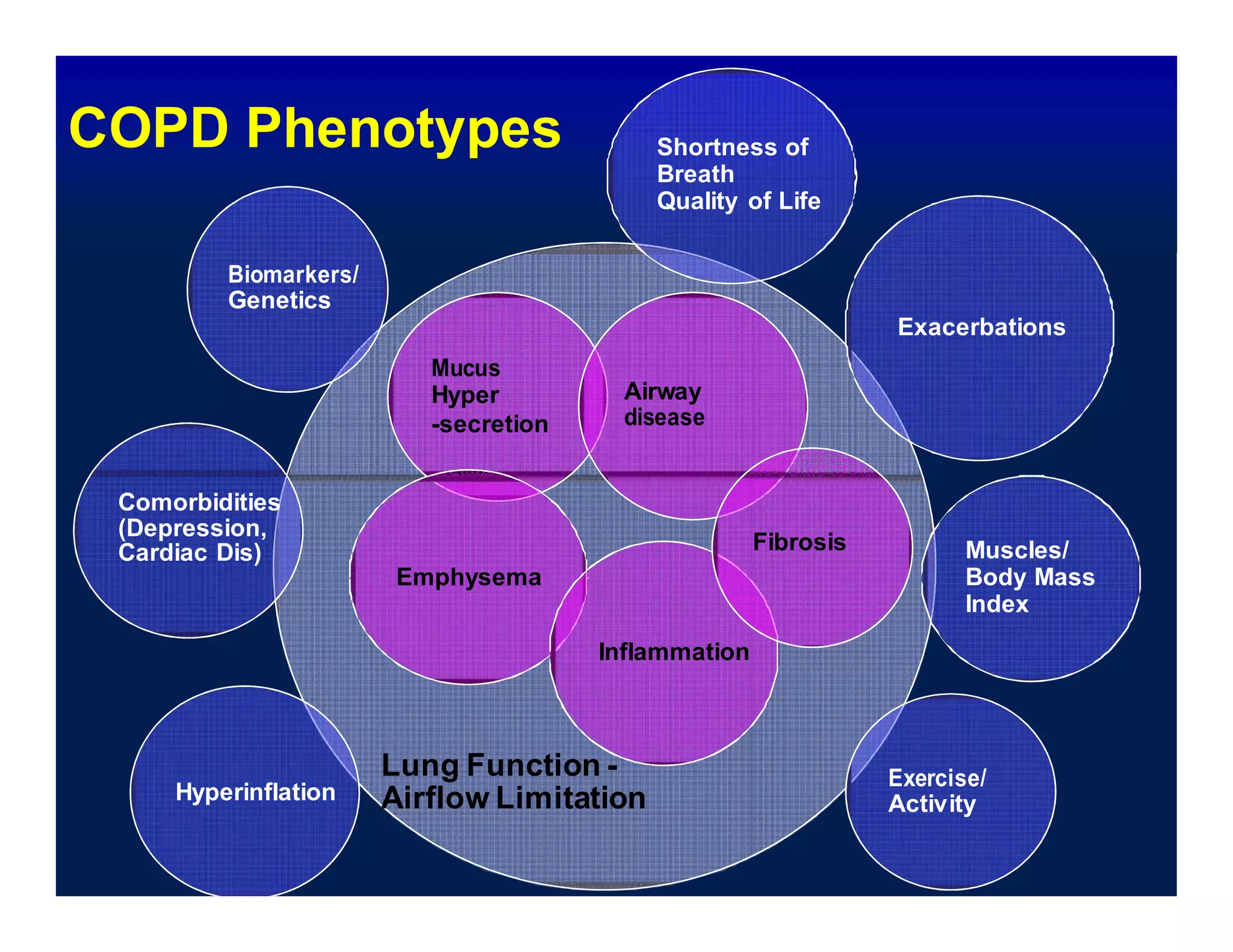
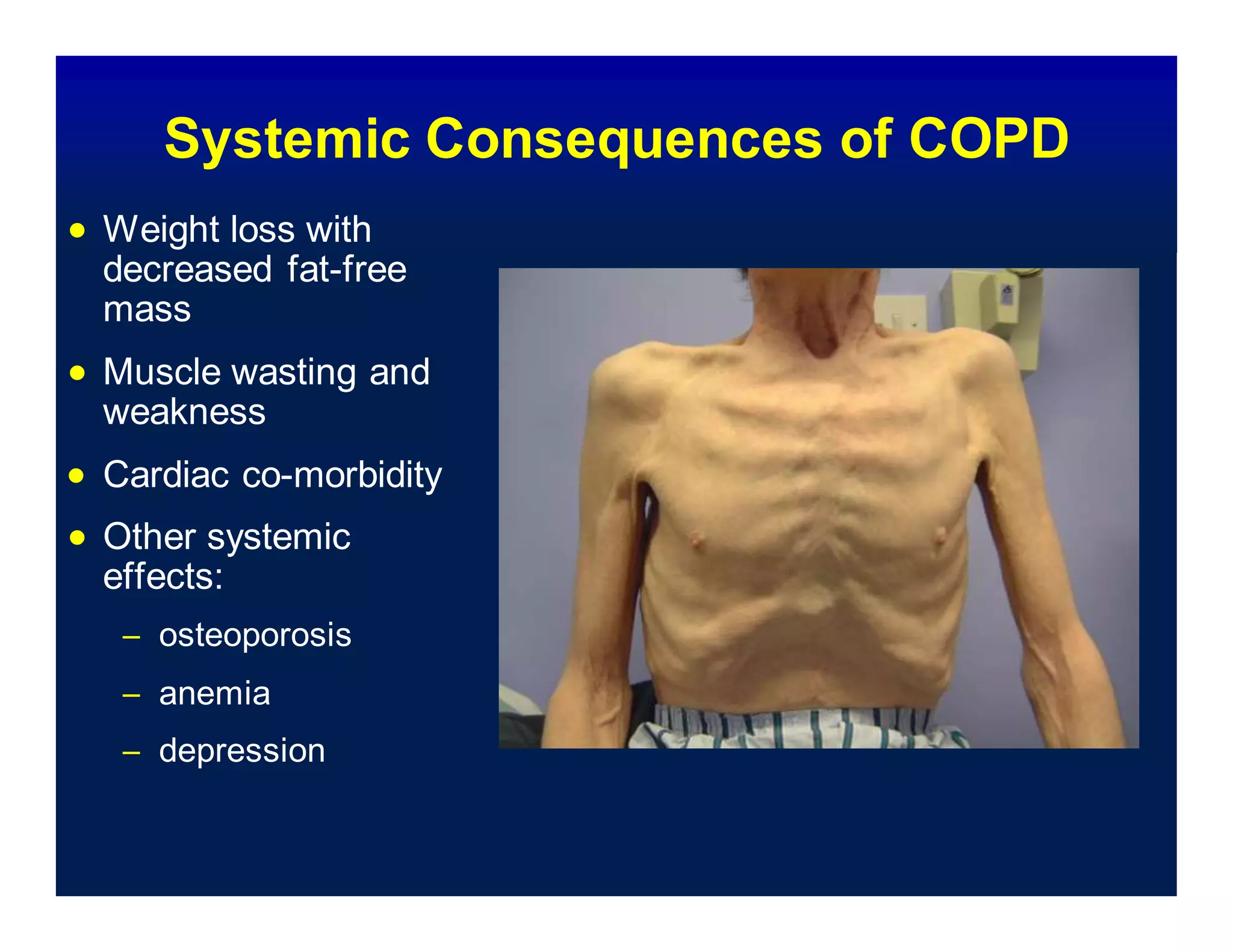
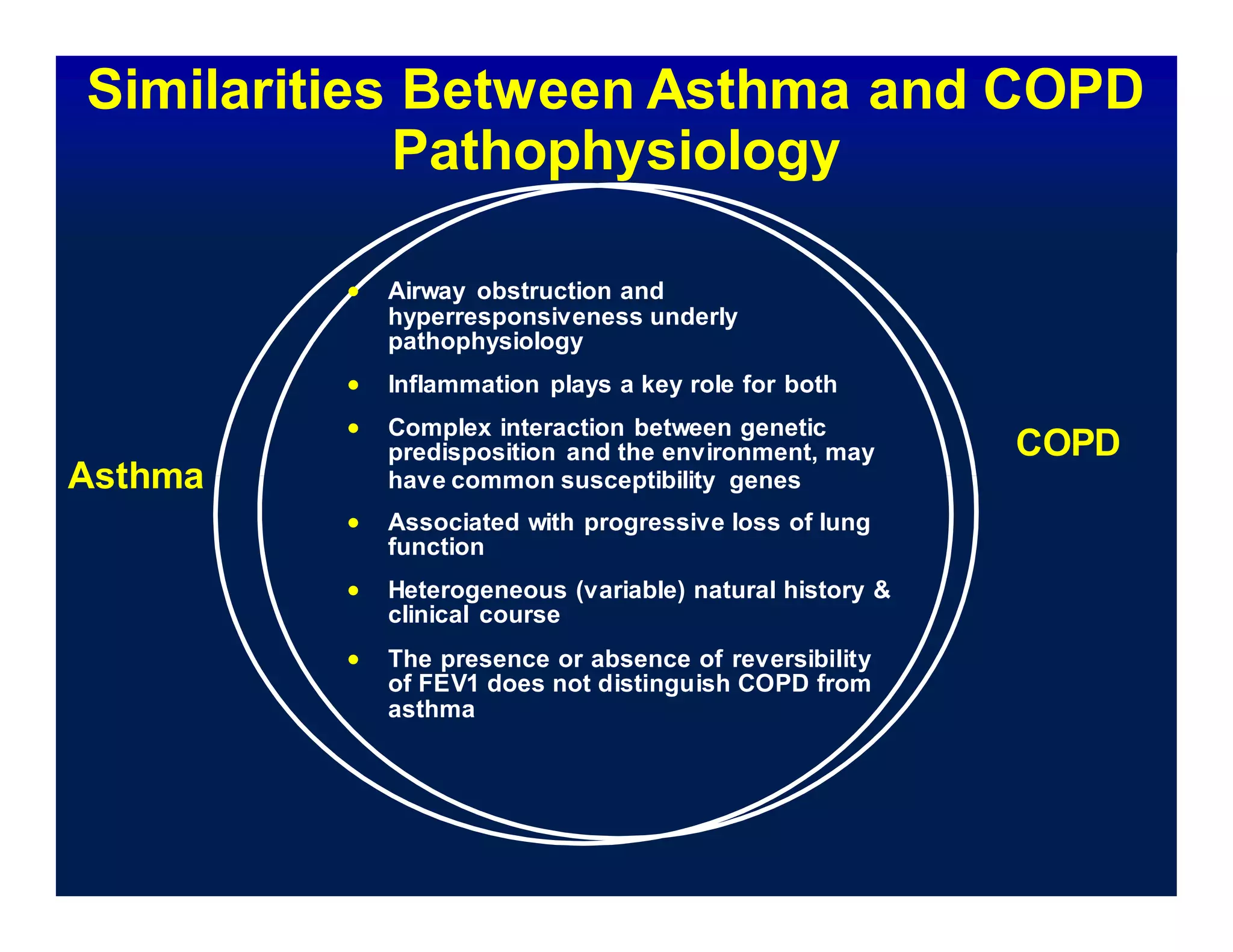
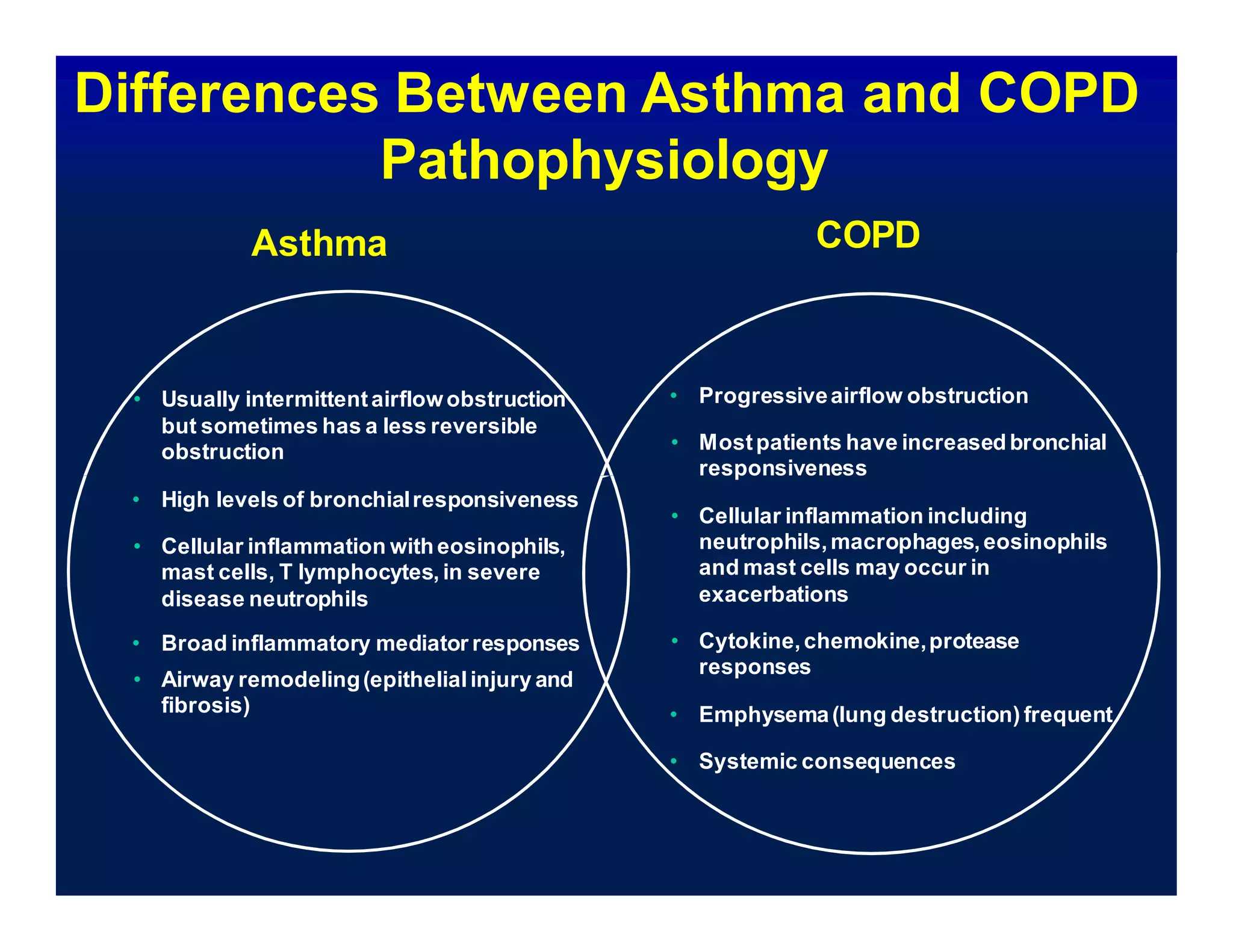
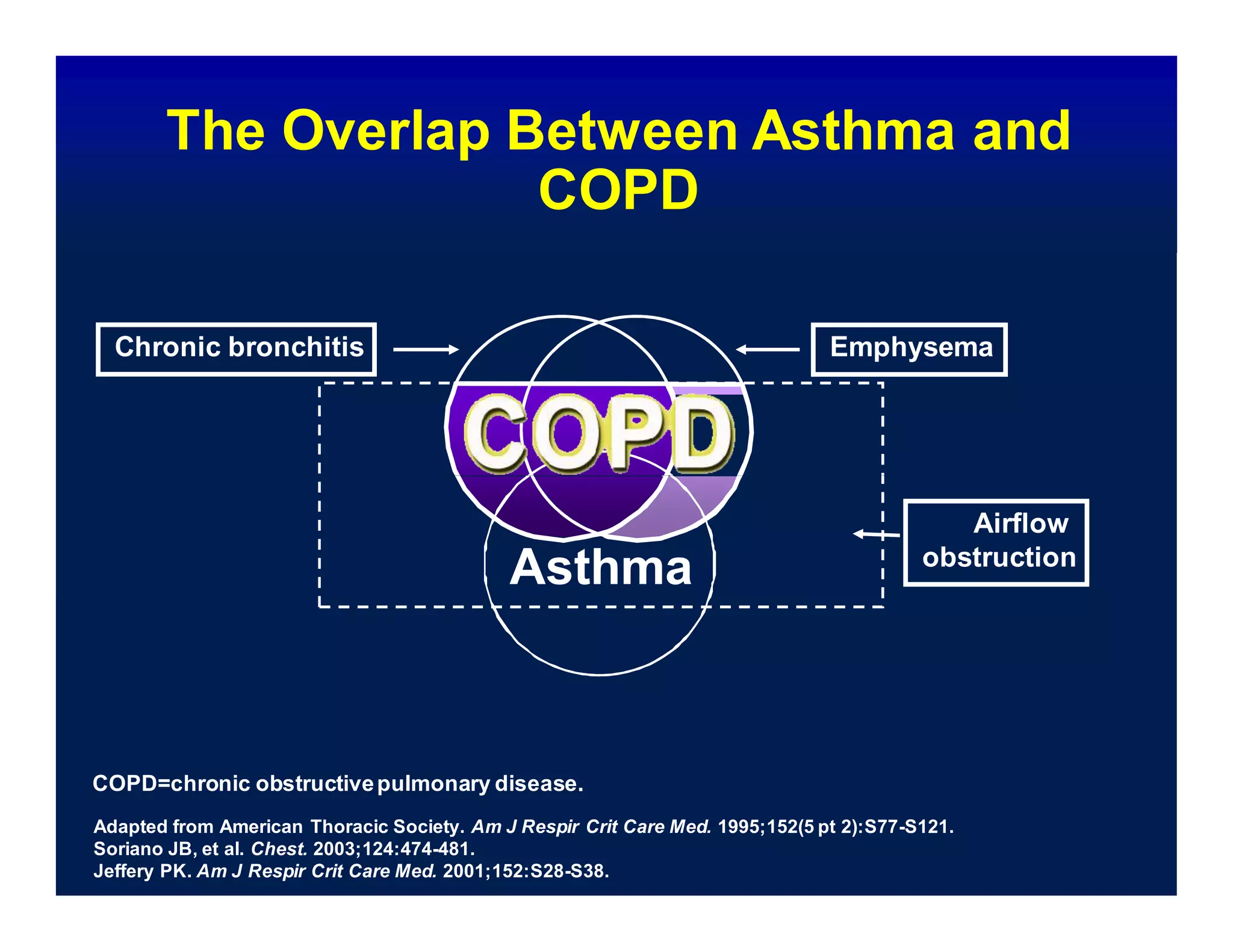
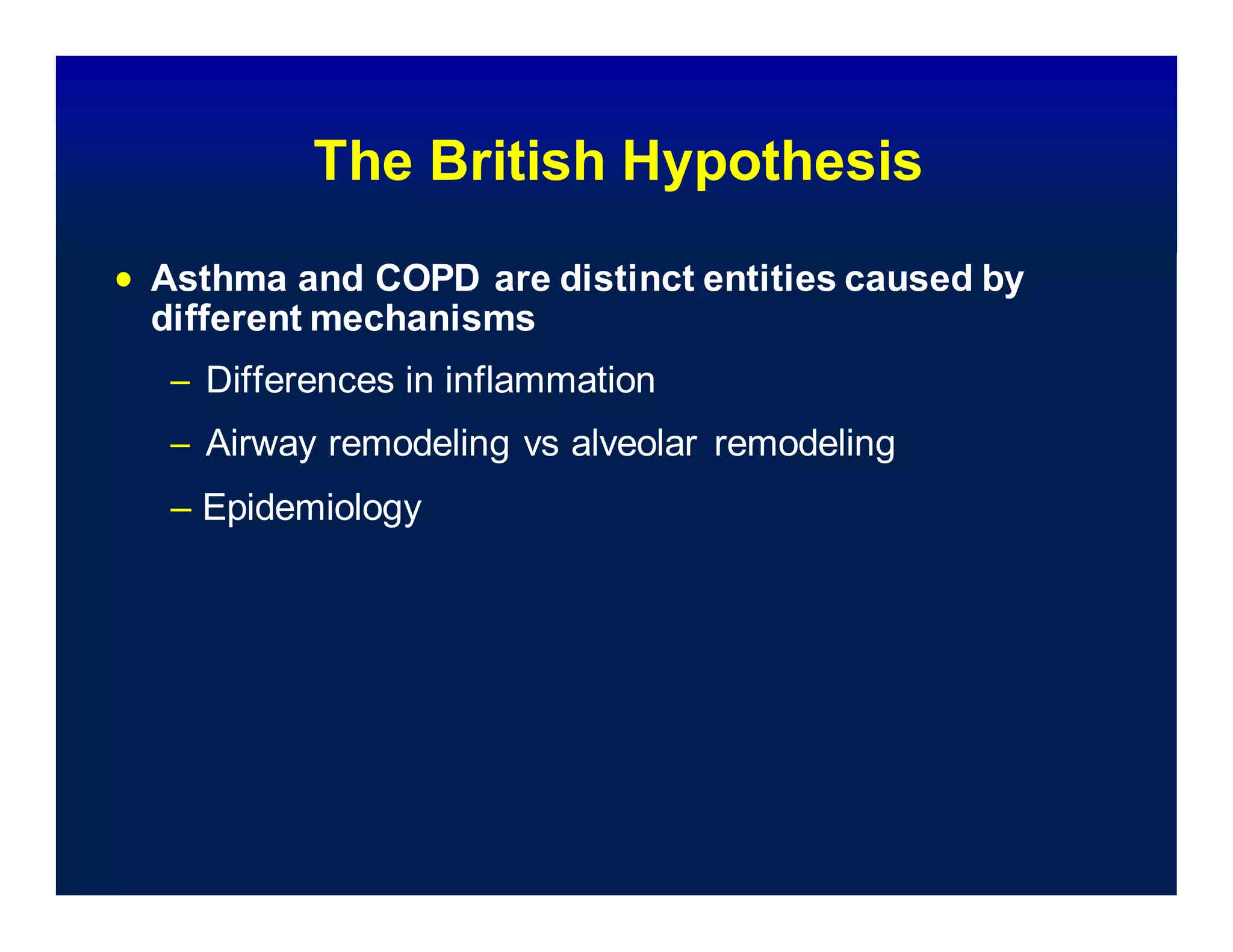
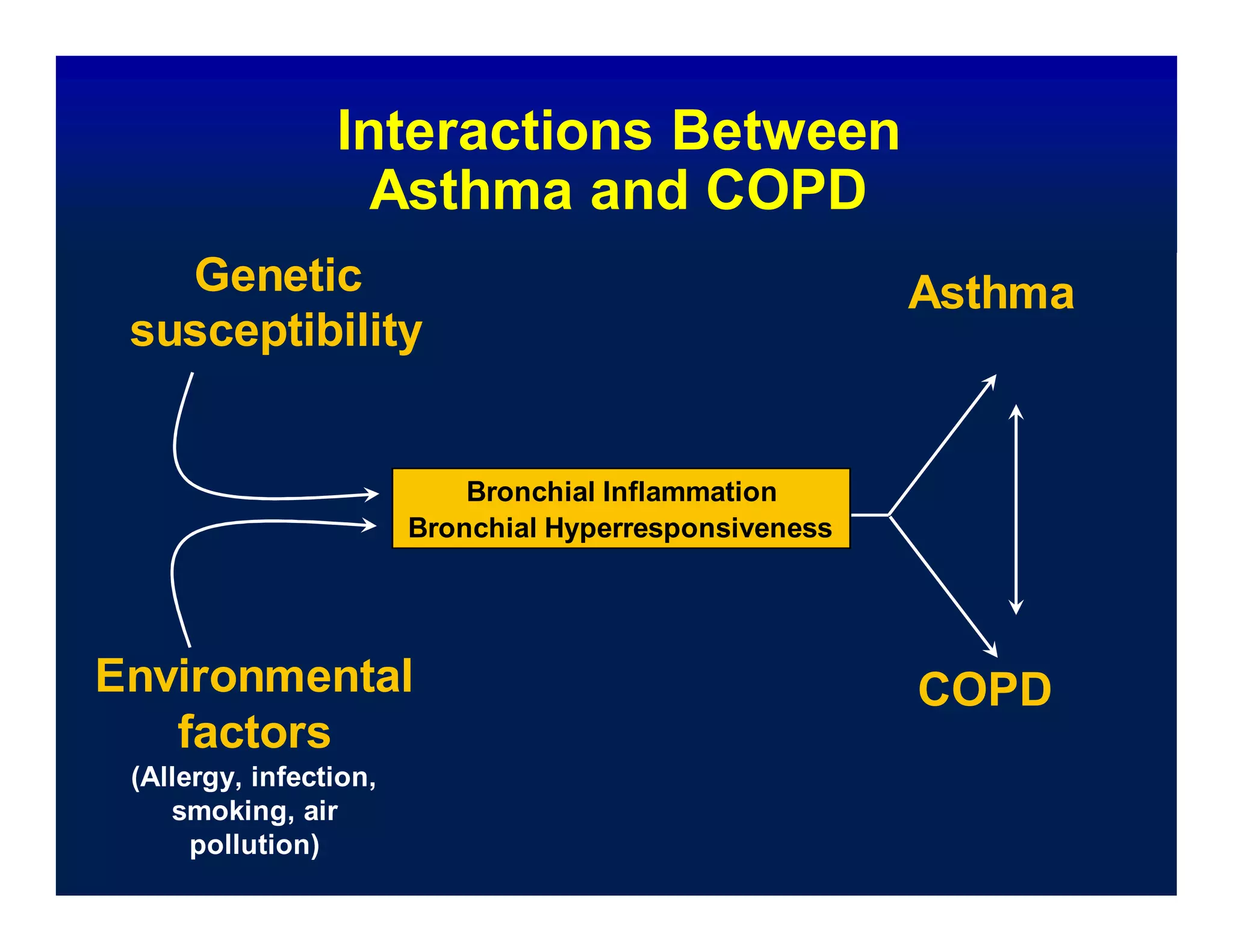
Asthma and COPD share some similarities in their pathophysiology such as airway obstruction, inflammation, and progressive loss of lung function. However, they also have key differences. Asthma typically causes intermittent airflow obstruction that is often reversible, along with eosinophilic inflammation and airway remodeling. COPD usually results in progressive and irreversible airflow limitation due to emphysema and chronic bronchitis involving neutrophilic inflammation and systemic consequences. While the presence of reversibility does not distinguish the two, their underlying inflammatory processes and structural lung changes differ substantially.

![Genetic Associations that Suggest
a Common Origin in COPD &
Asthma
IgE
BHR IL-13
Rate of FEV1 decline
Airway thickness ADAM33
van der Pouw Kraan TC.GenesImmun1999;61–65 Howard TD. Am J Respir
Cell MolBiol 2001;377–384 van der Pouw Kraan TC.GenesImmun 2002;436–439
Ohar JA [abstract].Eur Respir J 2001;P3588 Simpson A. Am J Resp Crit Care Med 2005;55-60
Holgate ST.Thorax2005;466-69 van Diemen CC. Am J Resp Crit Care Med 2005;329-33
JongepierH. Clin Exp Allergy 2004;757-60](https://image.slidesharecdn.com/copdandasthma-200225021030/75/Copd-and-asthma-7-2048.jpg)