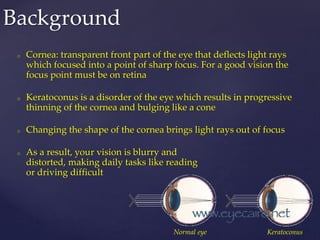
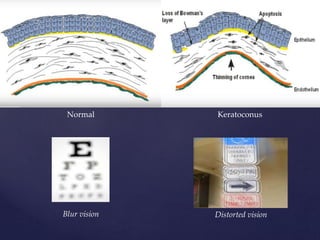
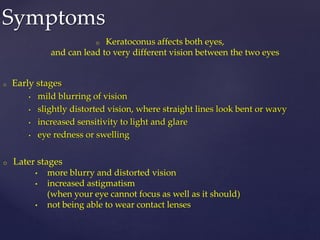
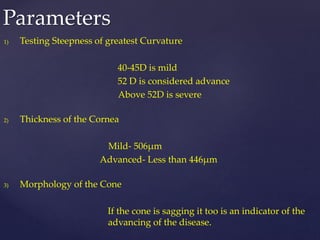
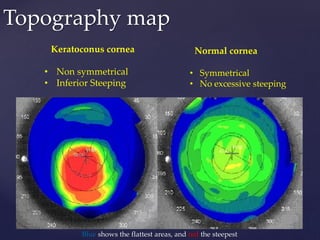
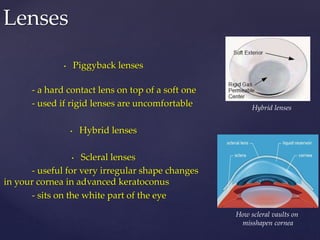
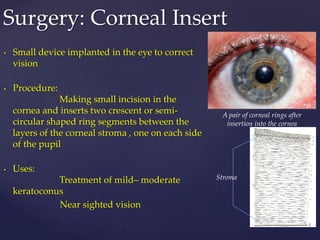
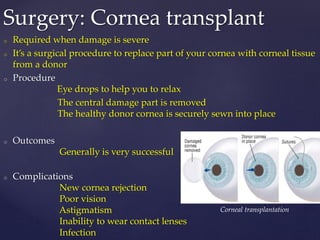
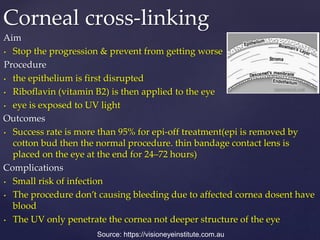
Keratoconus is a progressive disorder that causes thinning and distortion of the cornea, resulting in blurry and distorted vision, often affecting both eyes differently. Diagnosis involves assessing the curvature, thickness, and cone morphology of the cornea, with treatment options ranging from corrective lenses to surgical procedures like corneal inserts and transplants. Collagen cross-linking is a promising procedure aimed at stabilizing the cornea and preventing further progression, with a high success rate but some associated risks.