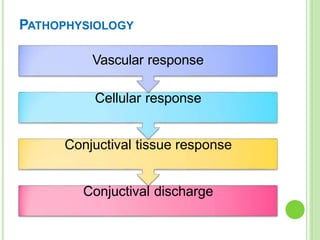
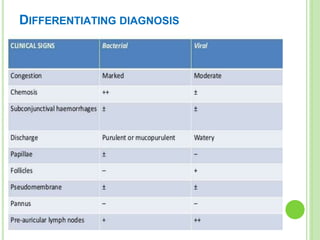
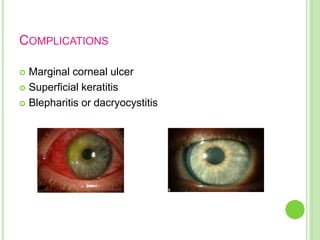
This document discusses bacterial conjunctivitis, including its classification, causes, symptoms, and treatment. It notes that bacterial conjunctivitis is a common type of pink eye caused by bacterial infection of the eye. The bacteria can spread through contact with an infected individual or exposure to contaminated surfaces. There are different clinical types of bacterial conjunctivitis, including acute, hyperacute, chronic, and angular, each with their own characteristic symptoms and causative agents. Treatment involves topical antibiotics, irrigation, and managing symptoms and complications.