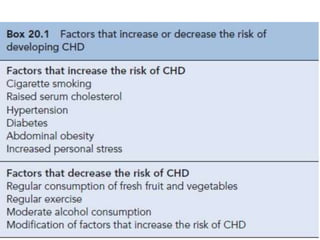
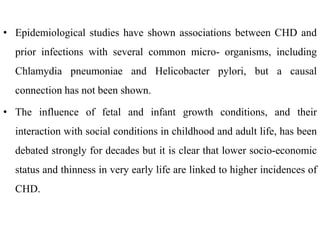
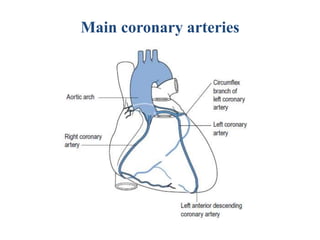
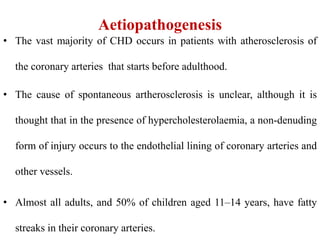
Coronary heart disease (CHD), also known as coronary artery disease (CAD), is characterized by impaired blood supply to the heart due to various factors, leading to myocardial ischemia and potentially heart muscle cell death. Epidemiologically, it is a leading cause of death in developed countries, particularly affecting certain demographics, with significant implications for public health. Risk factors for CHD include hypertension, smoking, high cholesterol, and diabetes, while the underlying pathological process involves atherosclerosis characterized by plaque formation in coronary arteries.



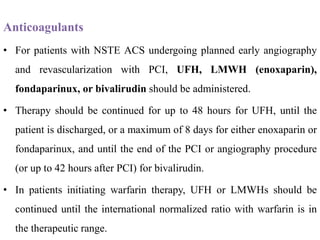
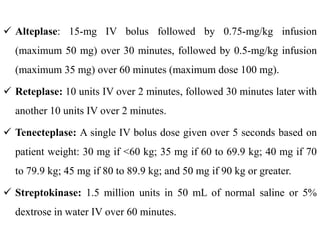
![• Patients with relative contraindications to fibrinolytics may receive
therapy if the perceived risk of death from MI is higher than the risk
of major hemorrhage.
• These situations include:
1) Severe, uncontrolled hypertension (blood pressure [BP] greater than
180/110 mm hg);
2) History of prior ischemic stroke longer than 3 months prior,
dementia, or known intracranial pathology not considered an absolute
contraindication;
3) Current anticoagulant use;](https://image.slidesharecdn.com/4myocardialinfraction-211001170935/85/4-myocardial-infraction-64-320.jpg)
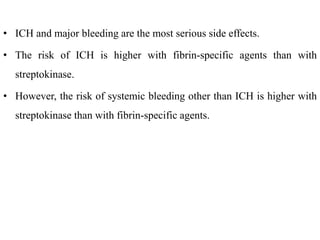


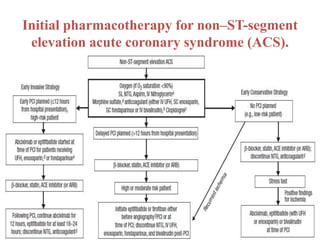
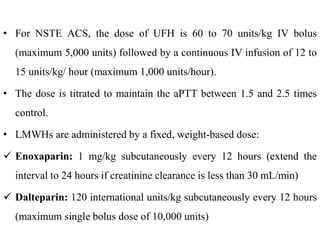
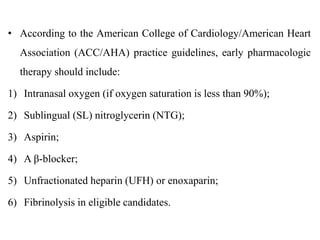
![• According to ACC/AHA practice guidelines, early pharmacotherapy
should include:
1) Intranasal oxygen (if oxygen saturation is <90%);
2) SL NTG (IV therapy for selected patients);
3) Aspirin
4) An oral β-blocker (IV therapy optional);
5) An anticoagulant (UFH, LMWH [enoxaparin], fondaparinux, or
bivalirudin).
• Morphine is also administered to patients with refractory angina, as
described previously.
• These agents should be administered early, while the patient is still in
the emergency department.](https://image.slidesharecdn.com/4myocardialinfraction-211001170935/85/4-myocardial-infraction-90-320.jpg)