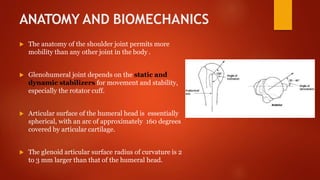
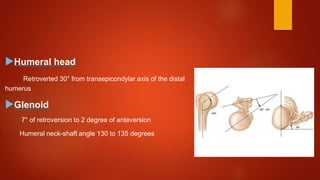
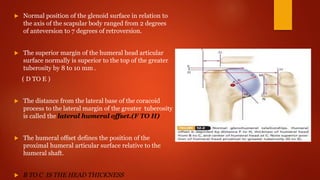
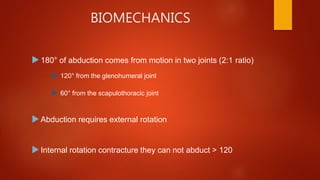
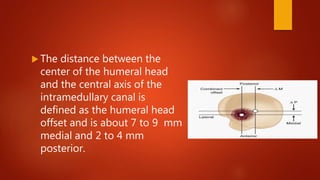
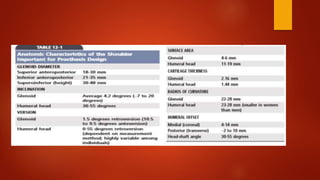
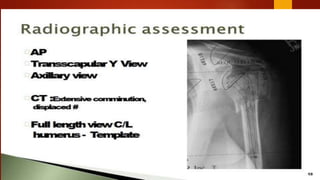
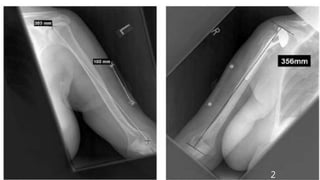
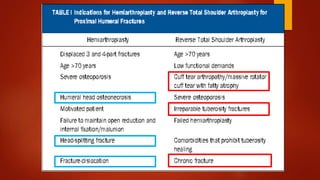
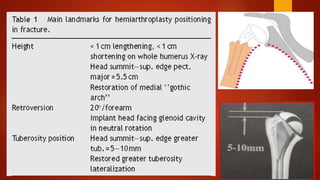
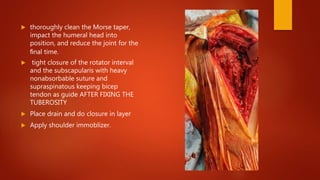
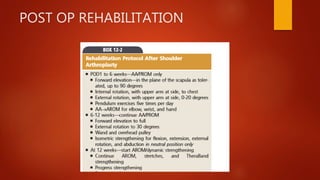
The document discusses the procedure of hemiarthroplasty for the shoulder, including the history, anatomy, surgical approach, indications, and complications. It provides details on prosthesis designs, preoperative planning, surgical steps such as exposure and implantation of the prosthesis, and postoperative management considerations. The objective of hemiarthroplasty is to relieve pain and restore functional range of motion to the shoulder joint.