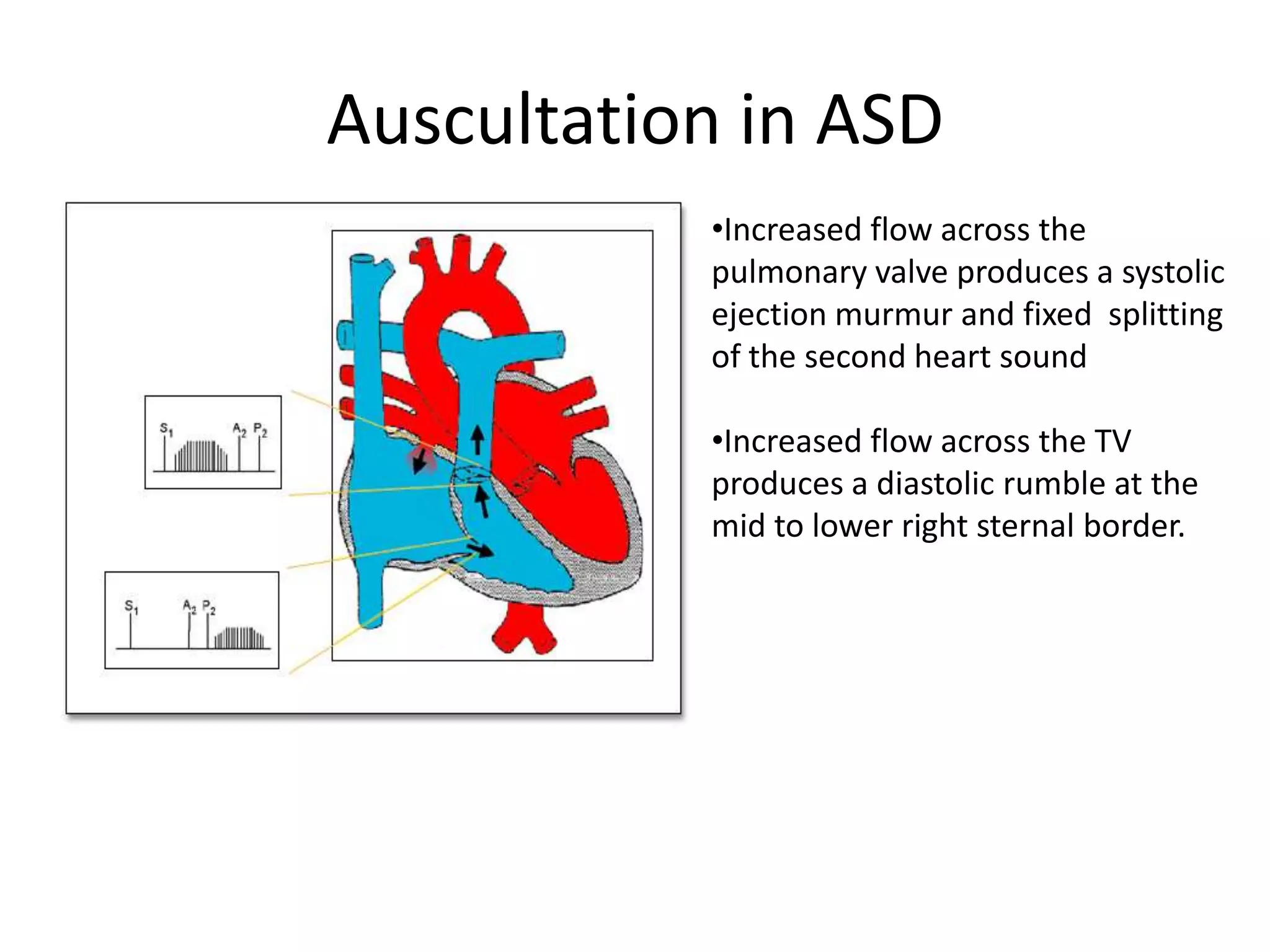
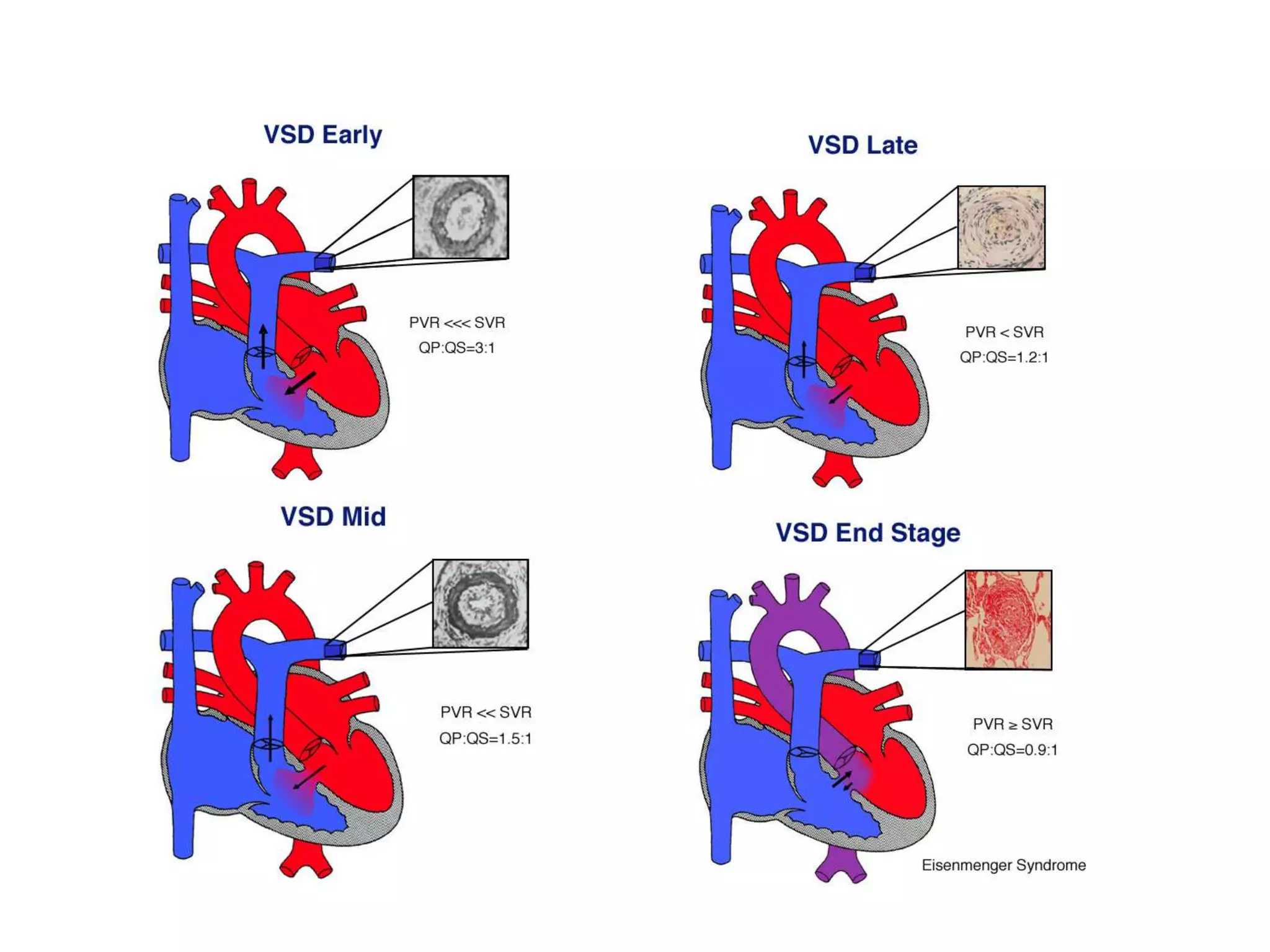
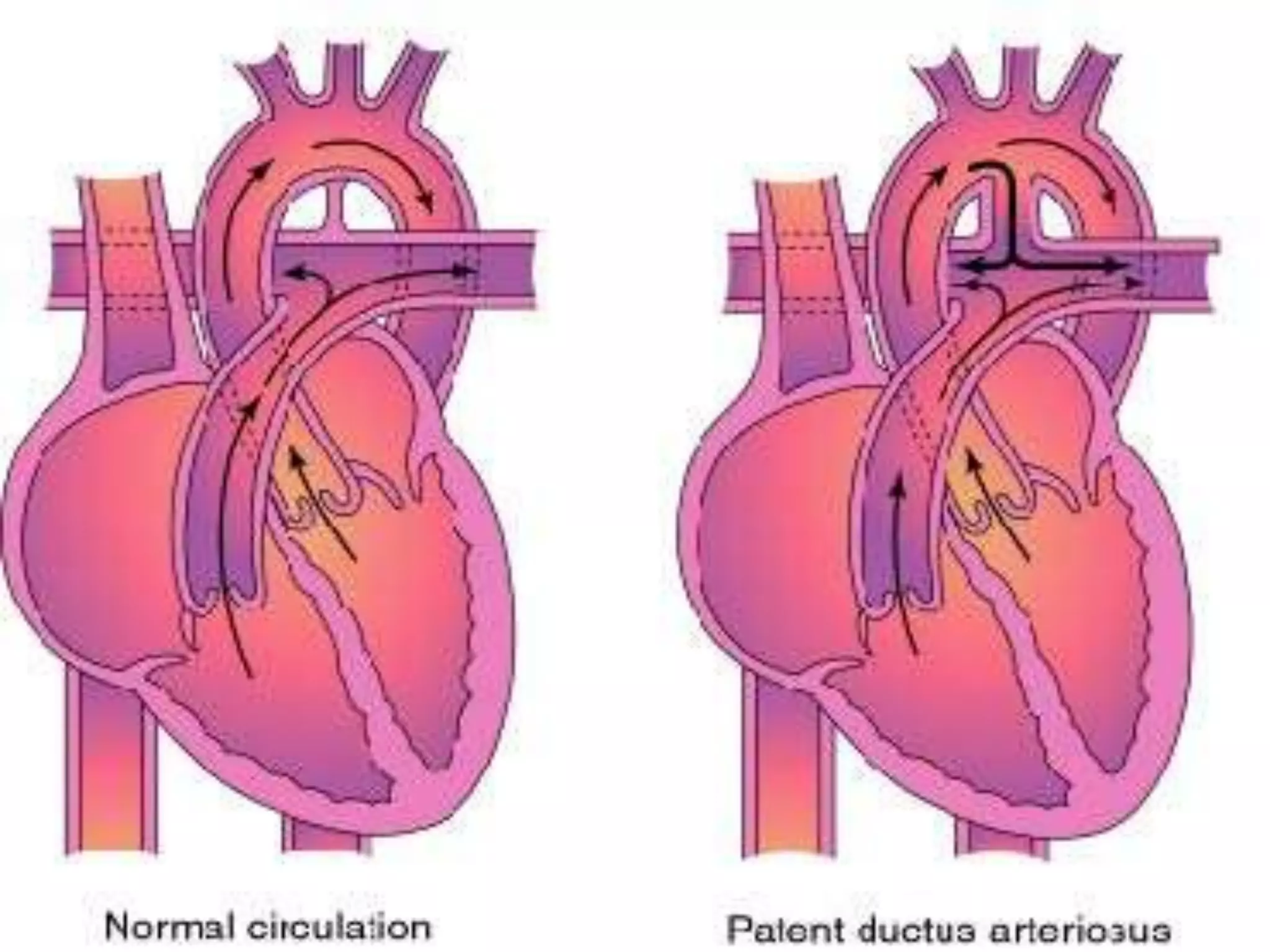
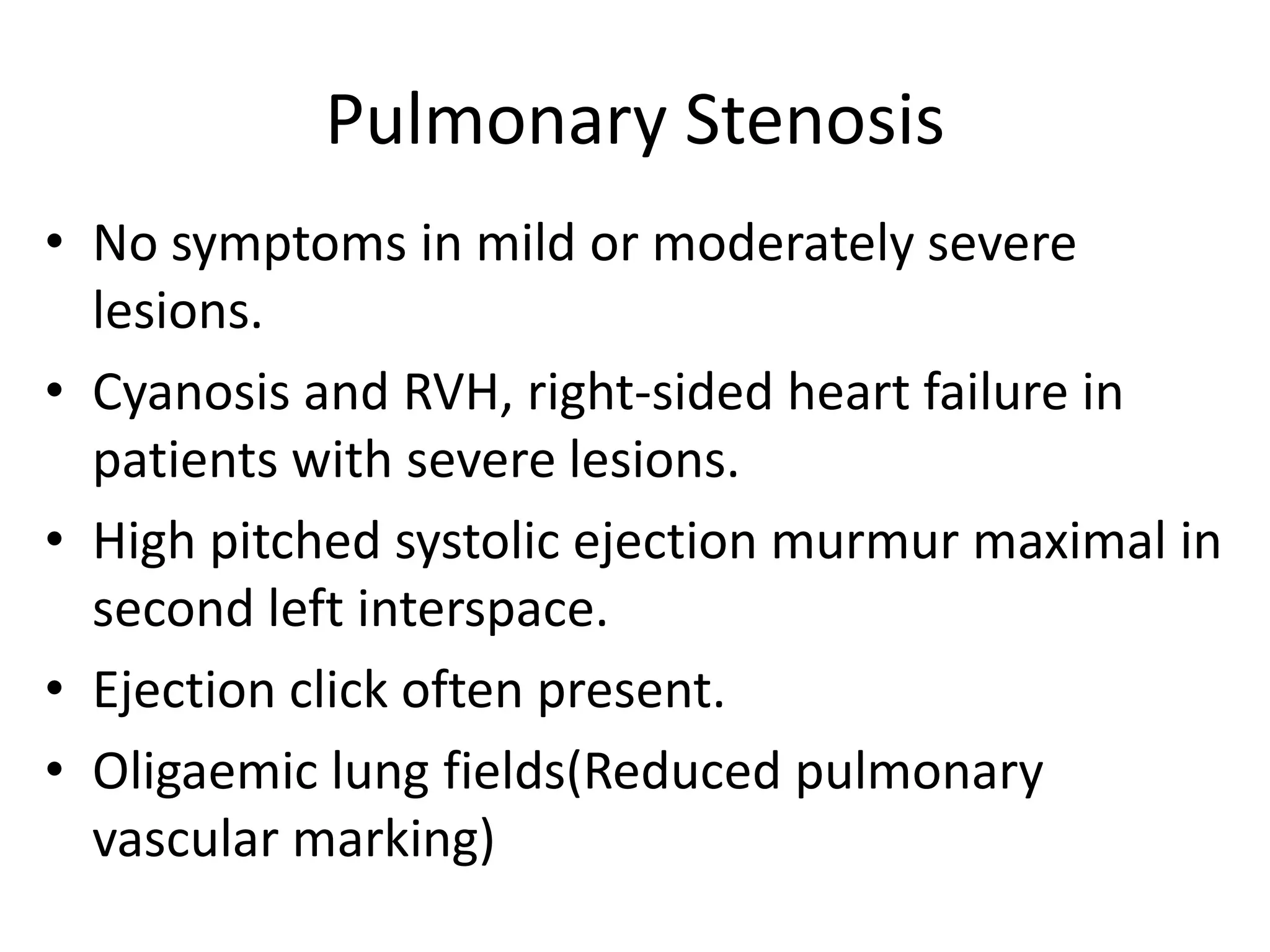
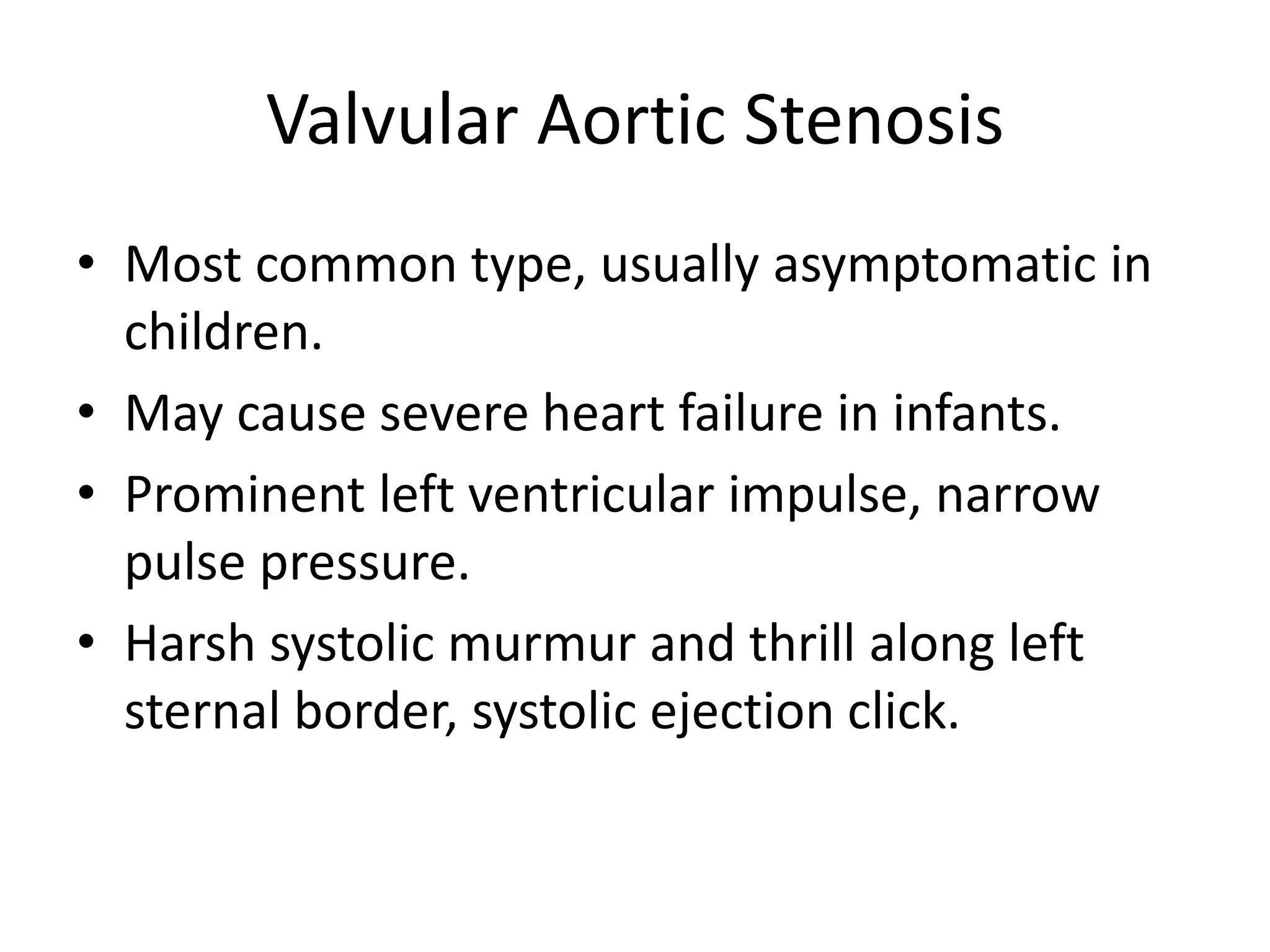
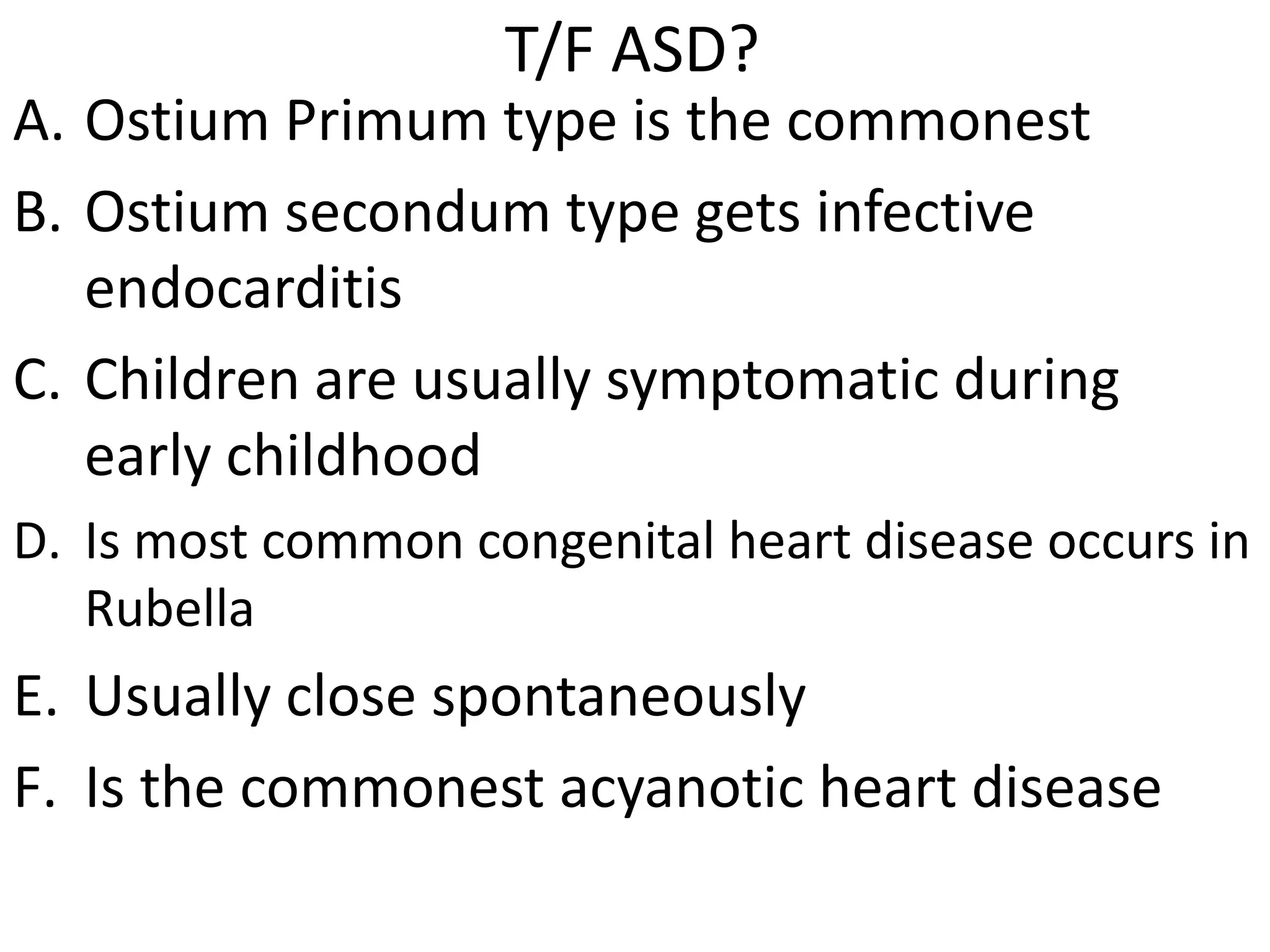
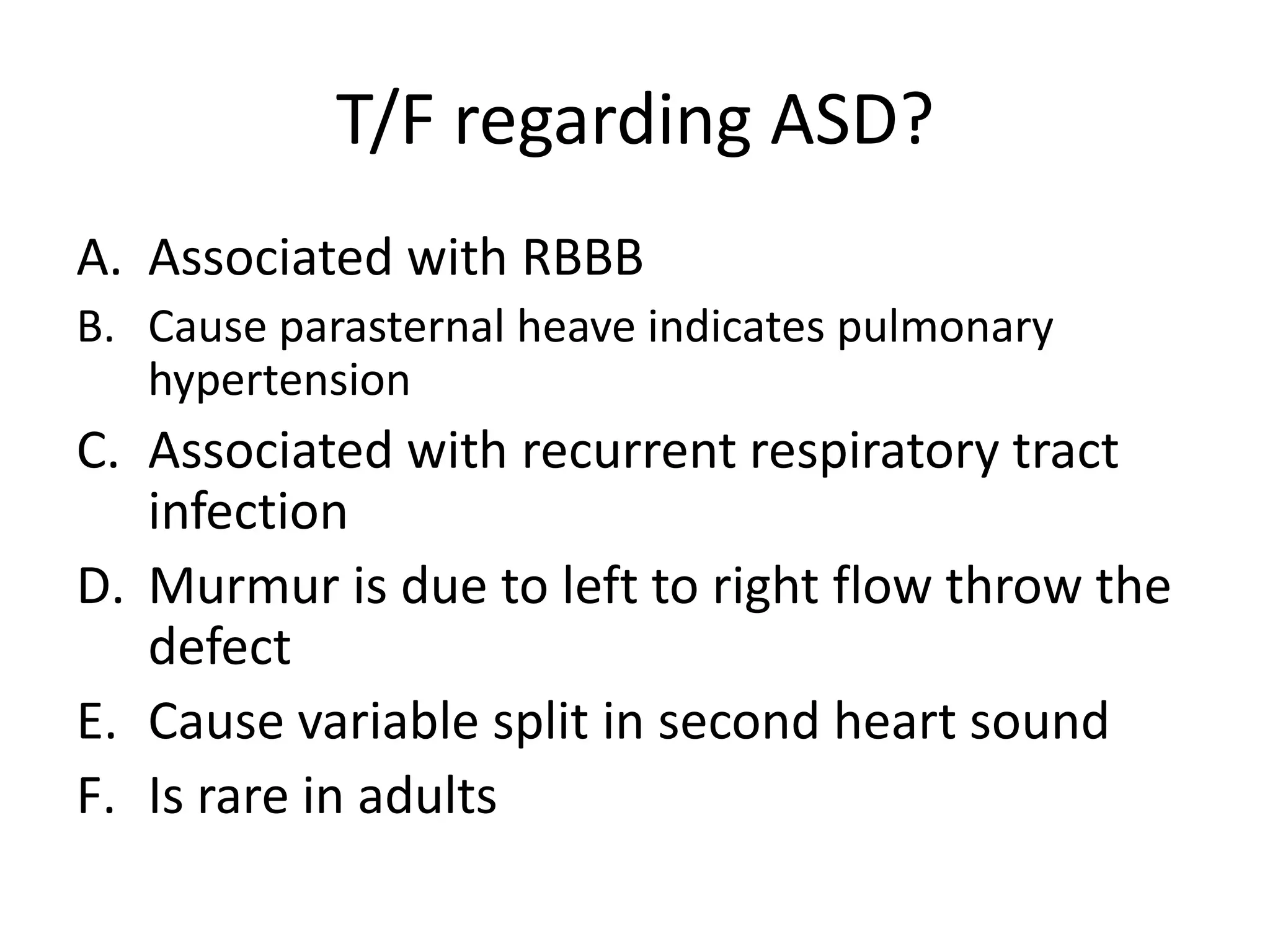
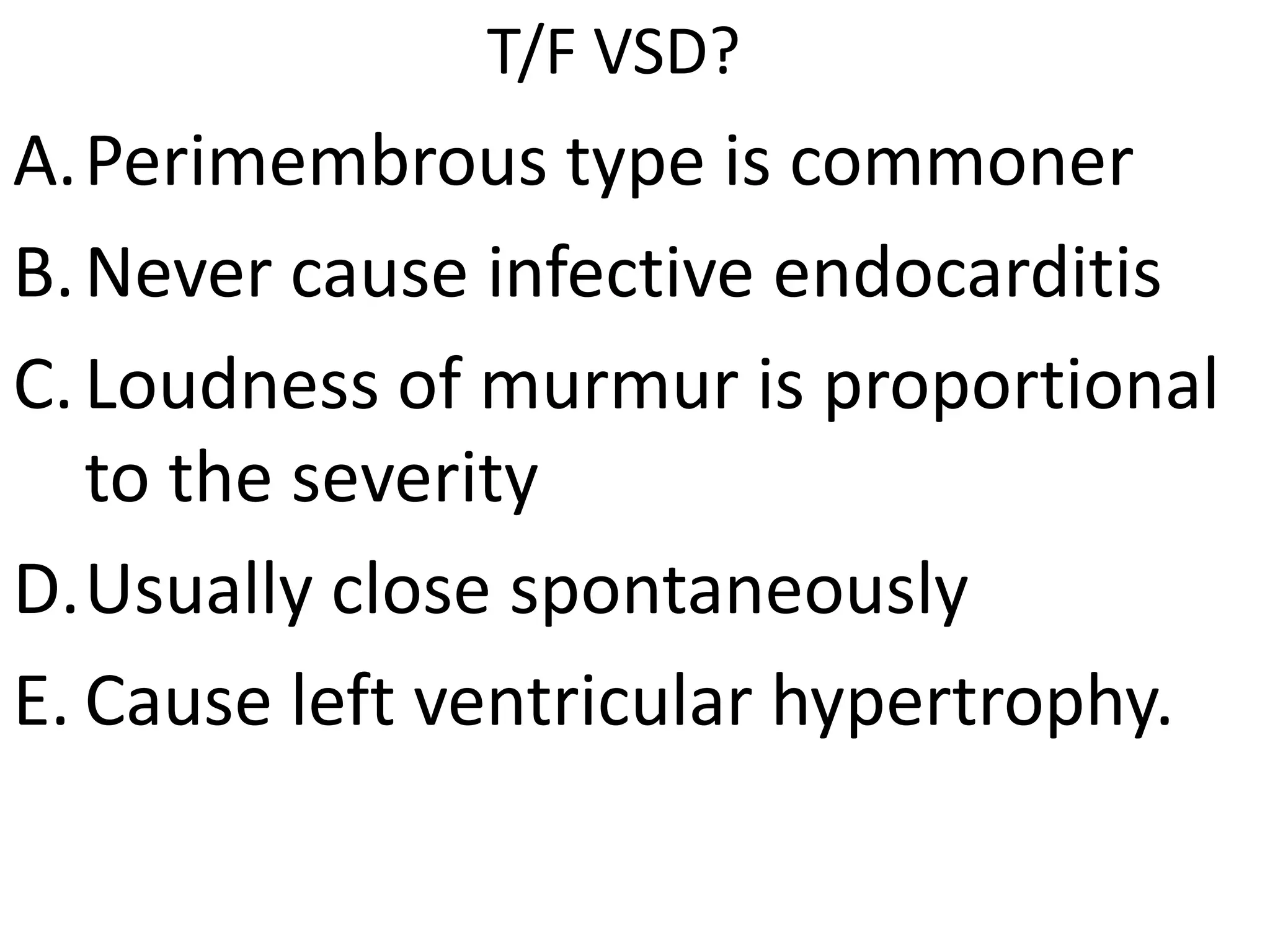
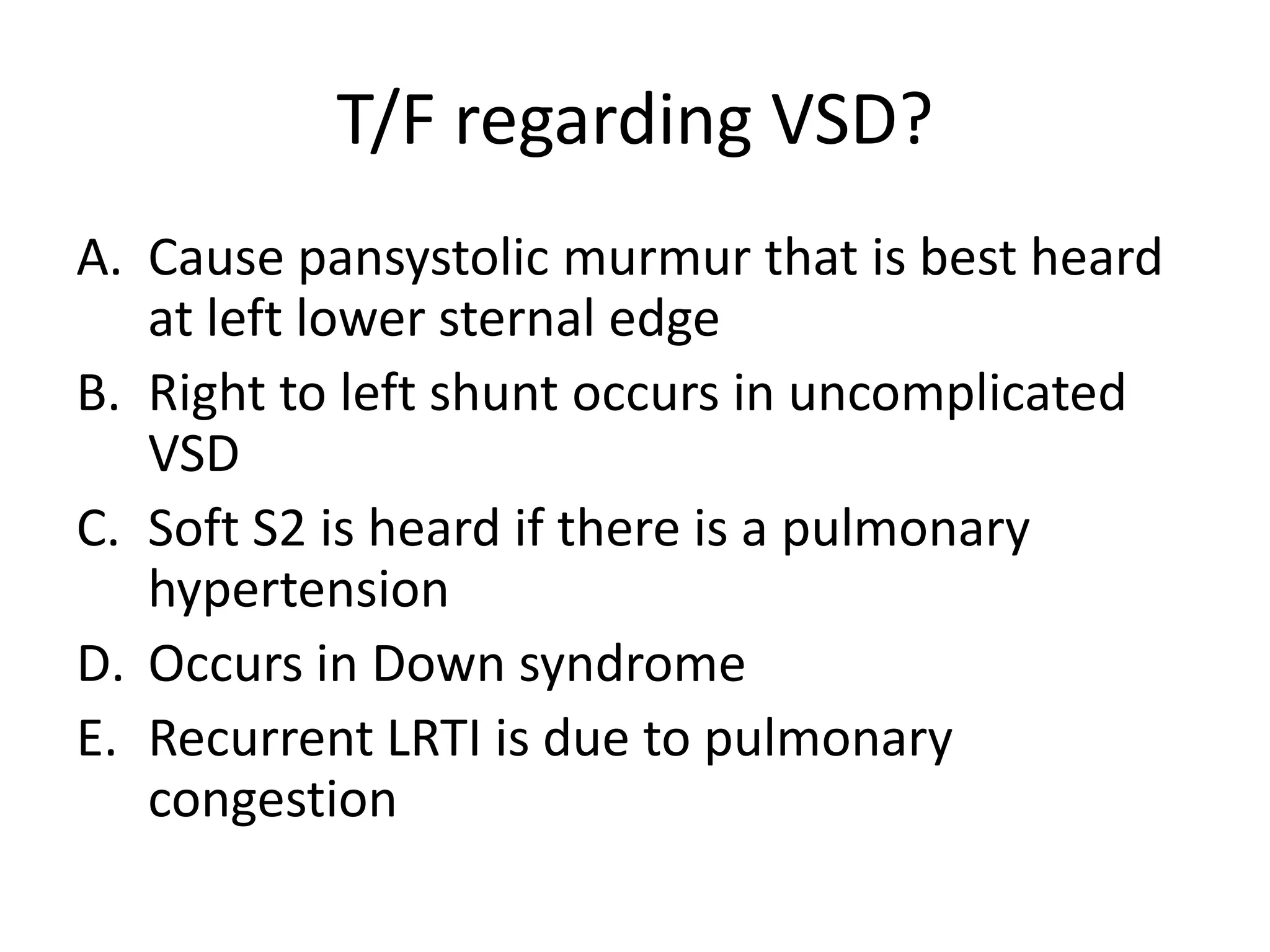
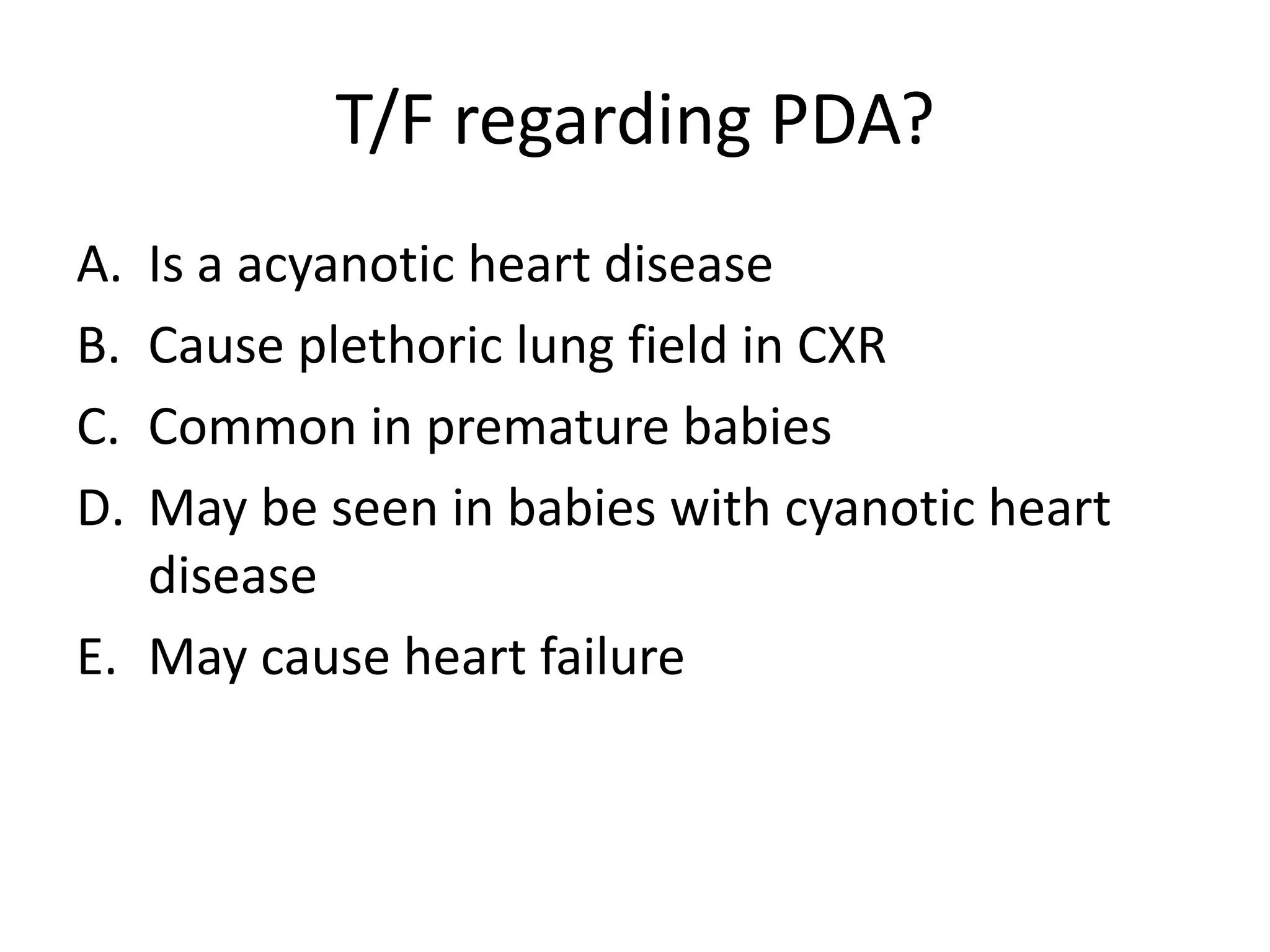
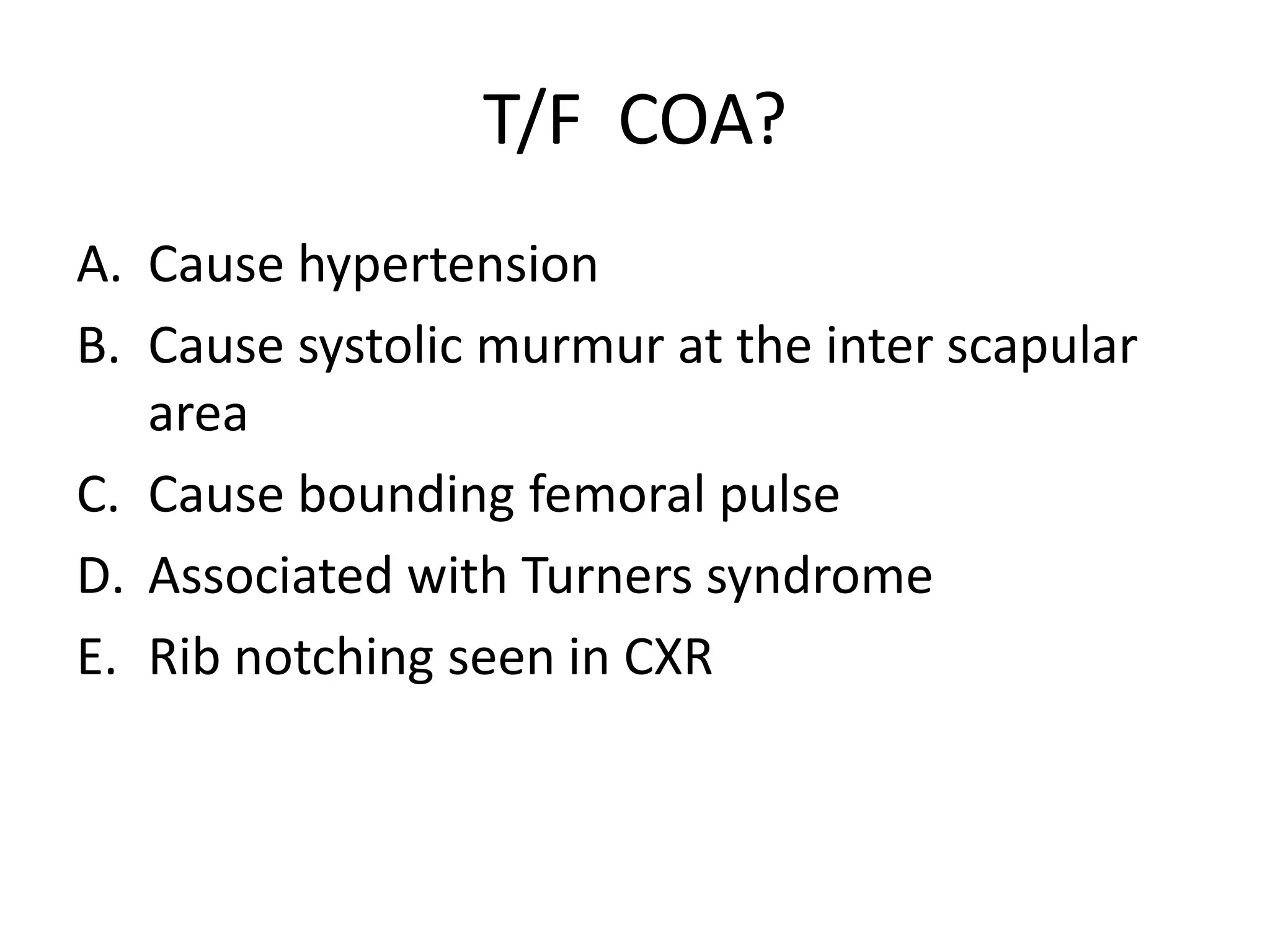
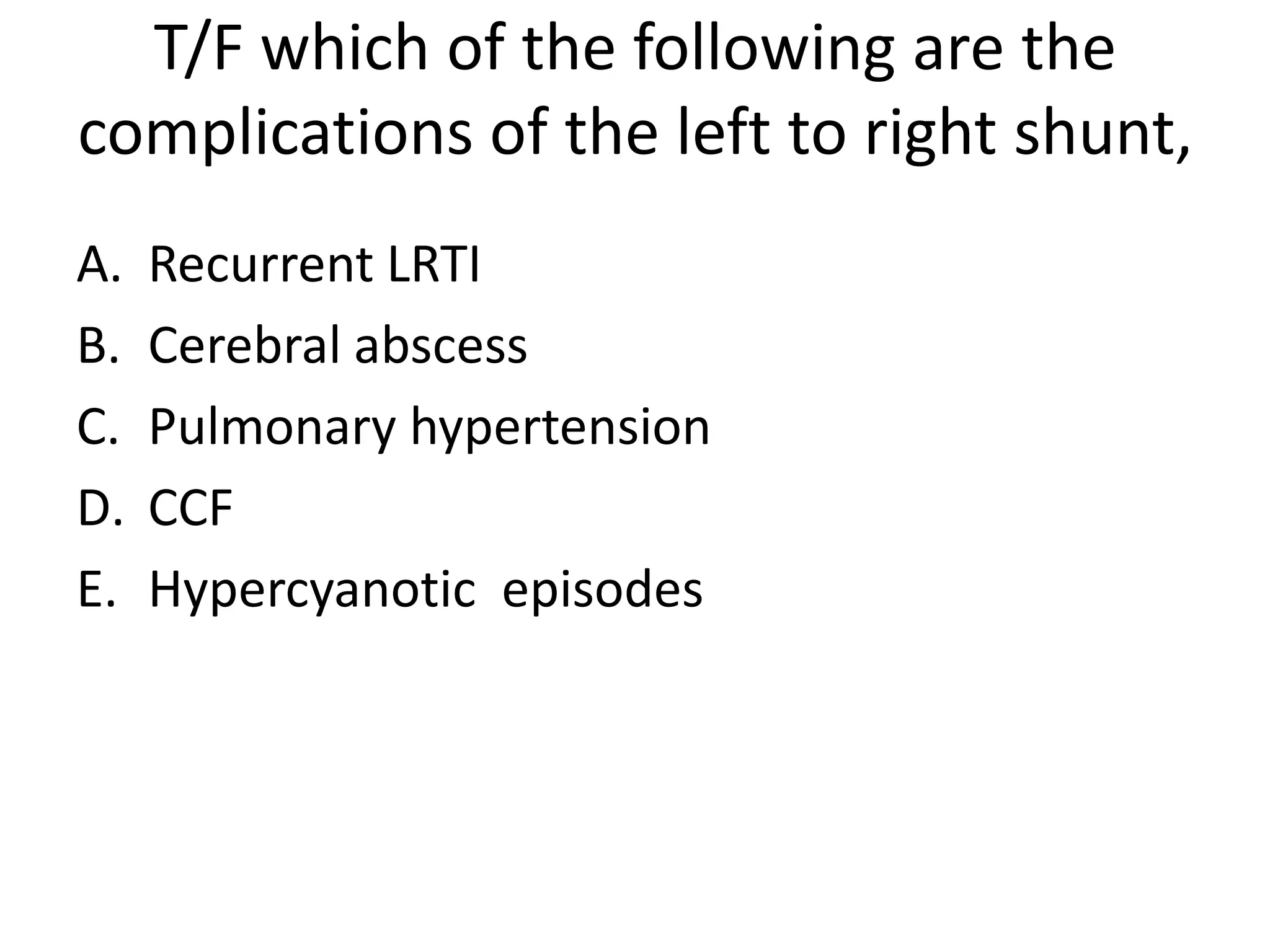
The document discusses various acyanotic heart diseases including atrial septal defect (ASD), ventricular septal defect (VSD), patent ductus arteriosus (PDA), coarctation of aorta, pulmonary stenosis, and aortic stenosis. It provides details on the pathophysiology, clinical features, investigations, and management of each condition. Key points include that ASD is the most common congenital heart disease, VSD has a pansystolic murmur at the lower left sternal edge, PDA causes a continuous murmur and loud P2 with pulmonary hypertension, coarctation causes hypertension and rib notching on CXR, and large defects can lead to pulmonary hypertension and