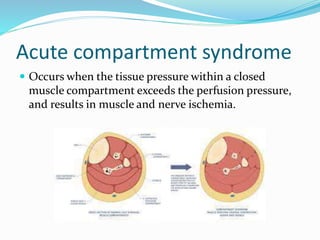
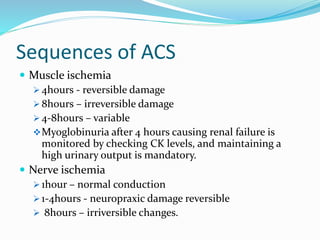
This document discusses acute compartment syndrome, beginning with definitions of acute and chronic types. It then covers the etiology, risk factors, diagnosis, signs and symptoms, management, and timing of fasciotomy for treatment. Key points include that pain disproportionate to injury and with passive stretching is the earliest indicator. Management involves removing external compression, maintaining blood pressure, and performing early fasciotomy to release fascia if compartment syndrome is diagnosed or suspected.