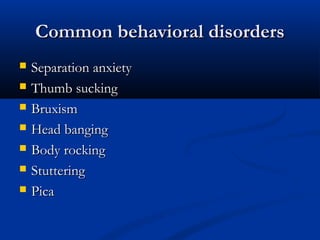
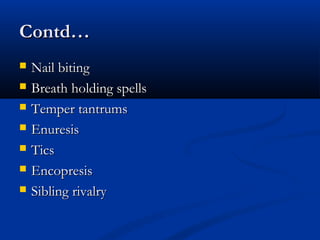
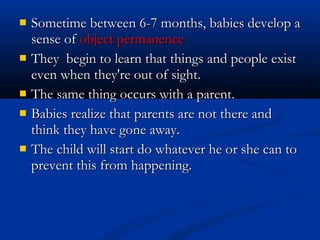
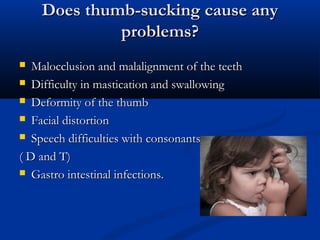
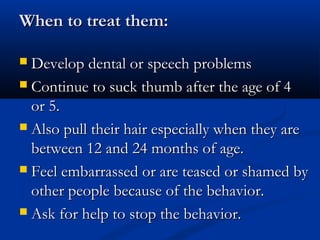
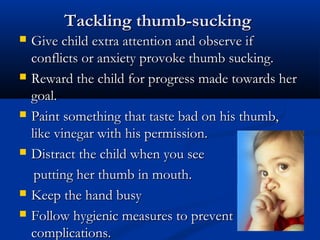
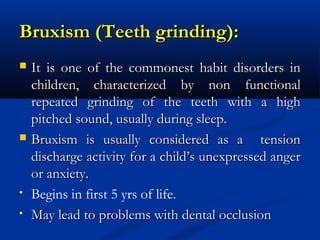
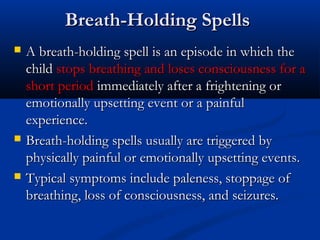
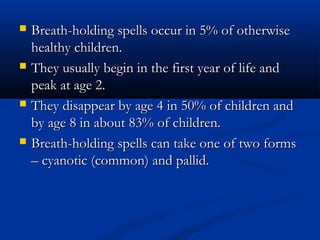
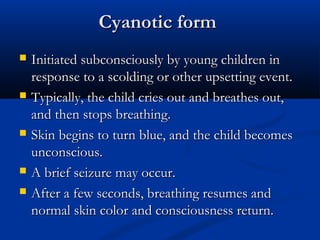
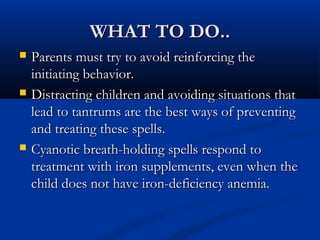
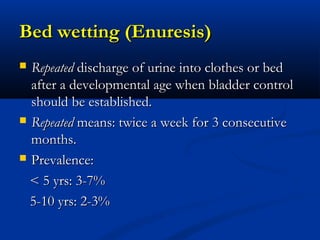
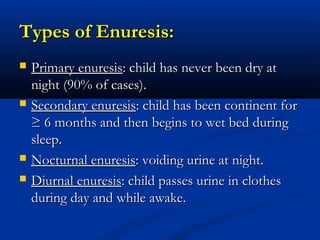
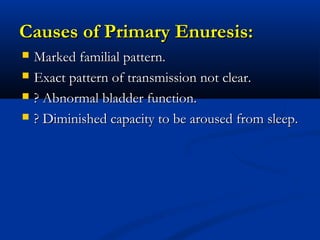
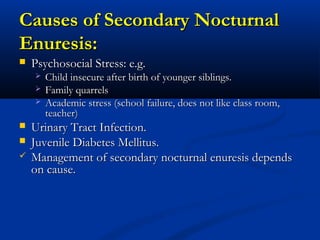
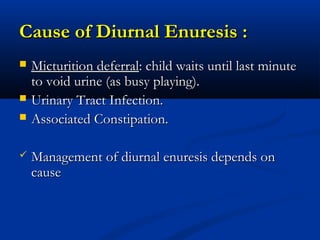
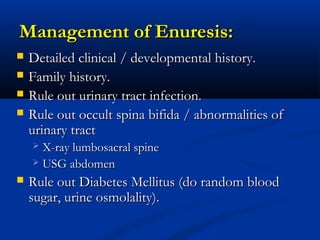
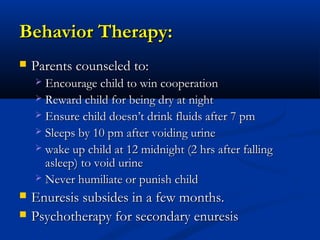
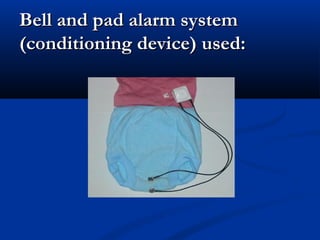
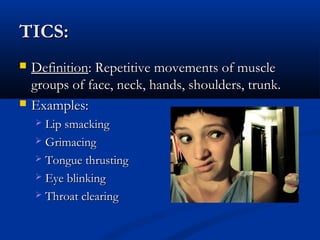
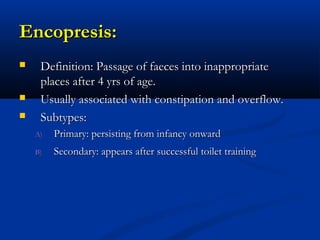
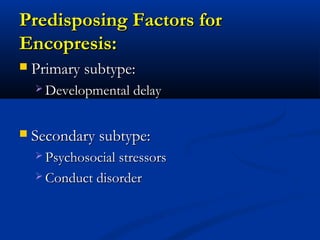
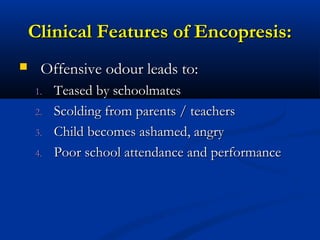
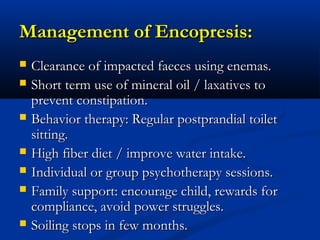
This document discusses various behavioral disorders commonly seen in children, including definitions, causes, and management strategies. Some of the behavioral disorders covered include separation anxiety, thumb sucking, bruxism, head banging, stuttering, pica, nail biting, breath holding spells, temper tantrums, enuresis, and tics. The document provides details on each disorder such as typical symptoms, what causes them, and how caregivers can help address them.