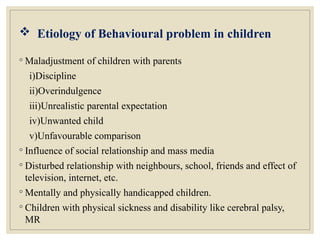
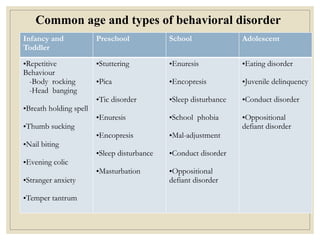
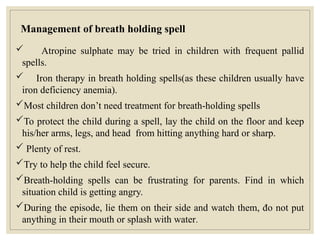
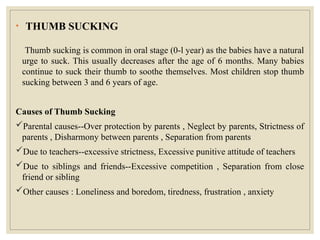
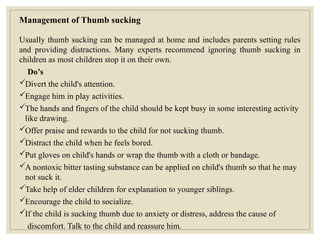
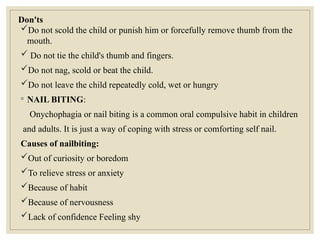
The document discusses behavioral problems in children, outlining their definitions, etiologies, and types. It emphasizes the importance of early identification and intervention for various disorders such as thumb sucking, nail biting, enuresis, and tic disorders. Additionally, it provides insights on management strategies, highlighting the role of parents and various therapeutic approaches to support children's behavioral development.