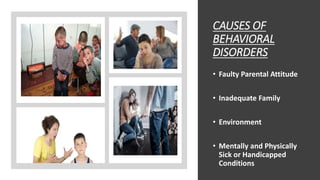
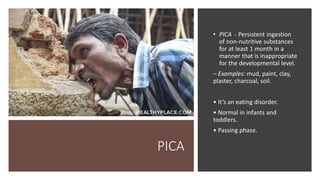
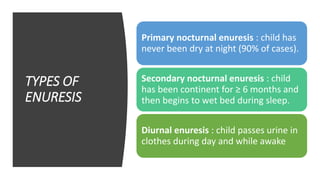
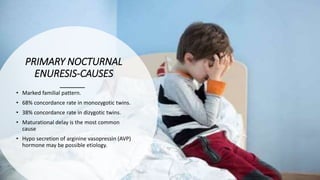
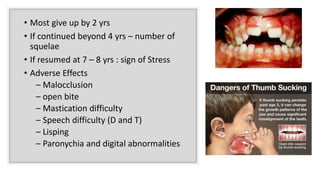
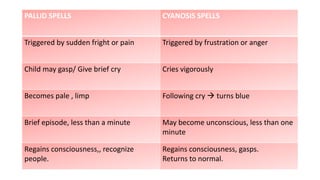
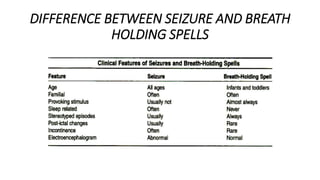
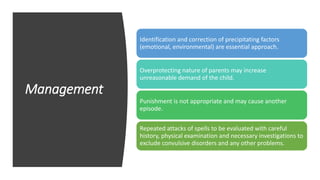
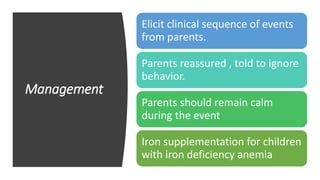
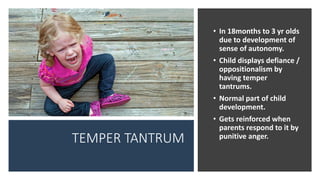
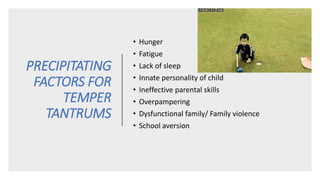
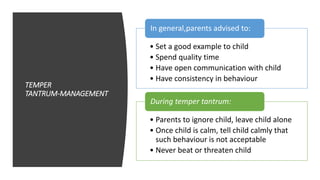
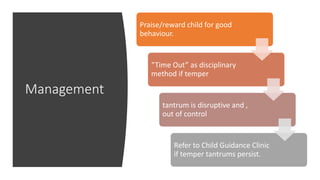
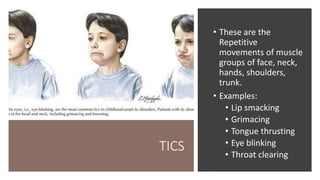
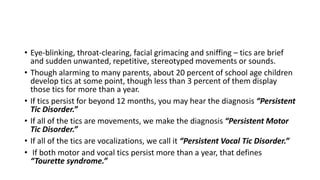
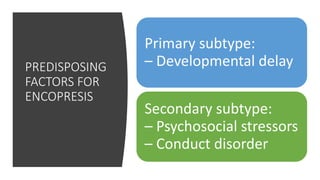
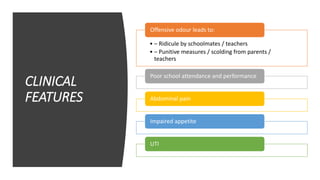
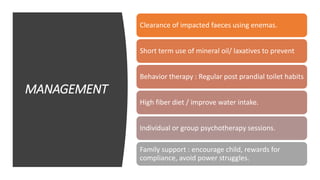
This document provides information on common behavioral problems in children. It discusses causes of behavioral disorders like faulty parental attitudes, inadequate family environment, and influence of social relationships. It describes types of behavioral problems stemming from emotional, physical, and social deprivation including temper tantrums, bedwetting, thumb sucking, and more. Assessment and management strategies are outlined for each condition. The document emphasizes the importance of parental support, clear communication, and developing a child's independence and social skills to address behavioral issues.