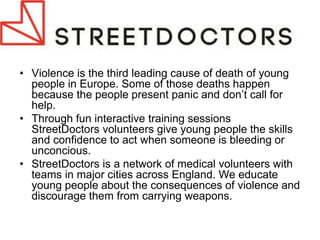
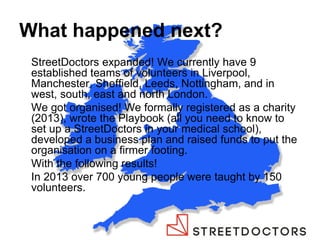
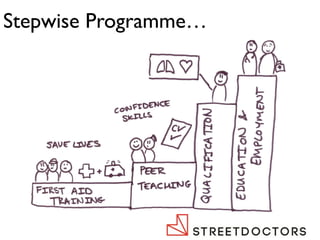
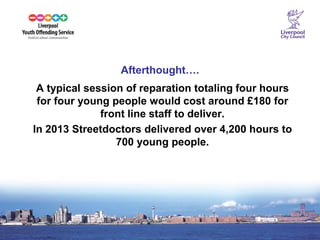
The document discusses the commissioning of social action approaches aimed at helping young people, focusing on initiatives like 'streetdoctors' which trains volunteers to engage with at-risk youth and alleviate youth violence through education and skills training. It describes the expansion of the program across various cities in England, the operational structure of local and national teams, and future goals for increased volunteer involvement and outreach. The document also touches on the broader implications of these social programs in terms of community engagement and the integration of diverse social services.