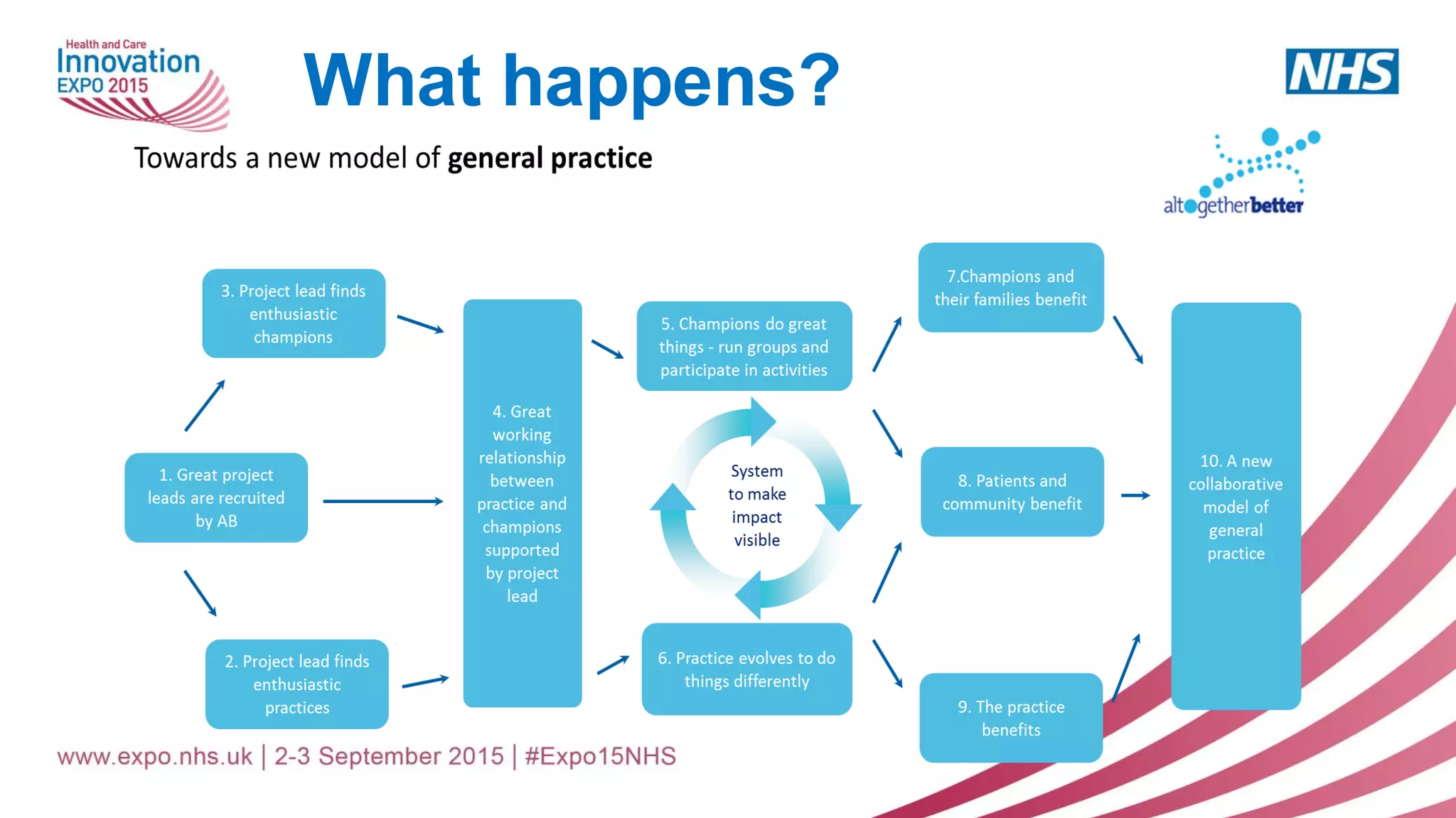
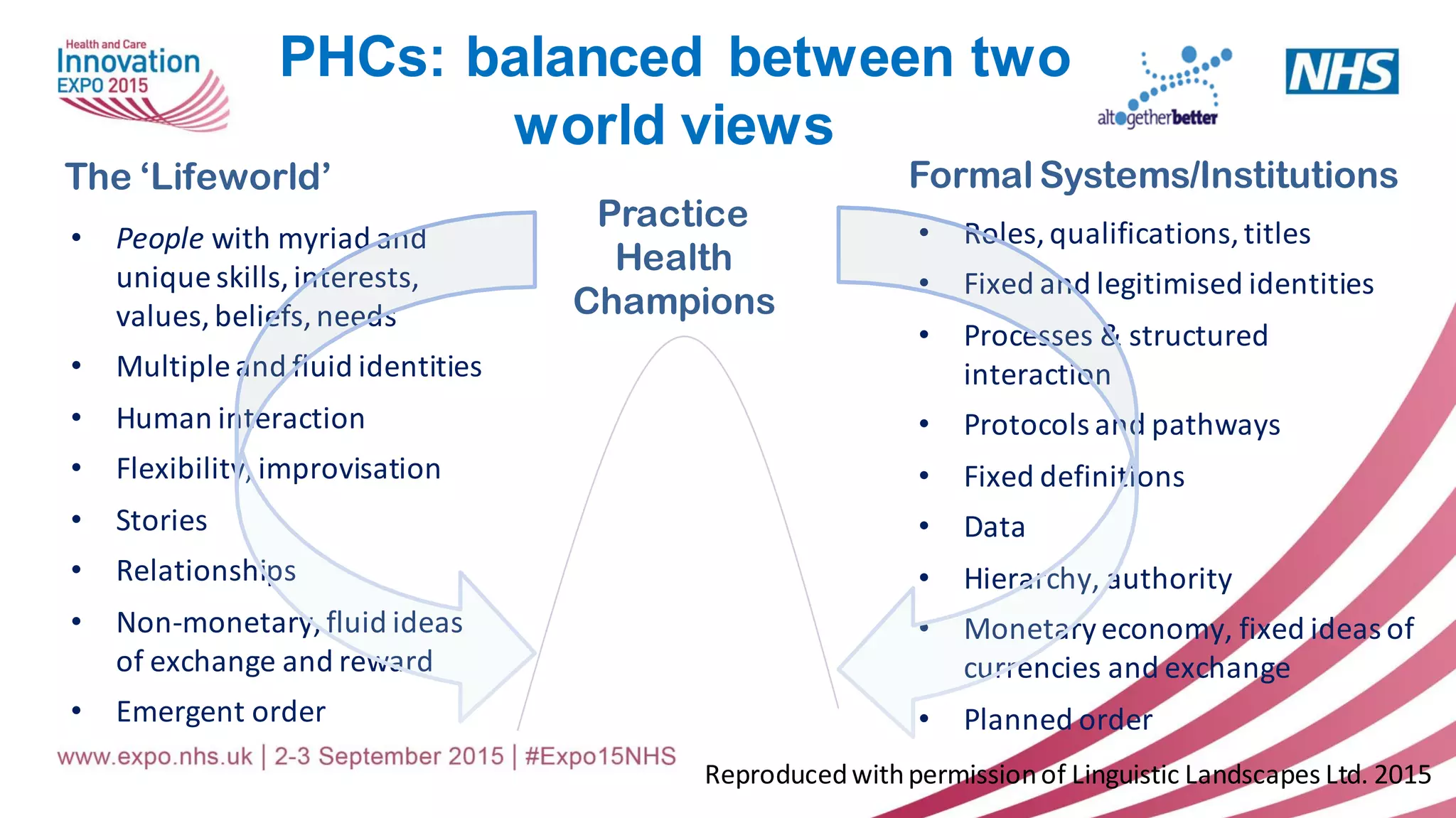
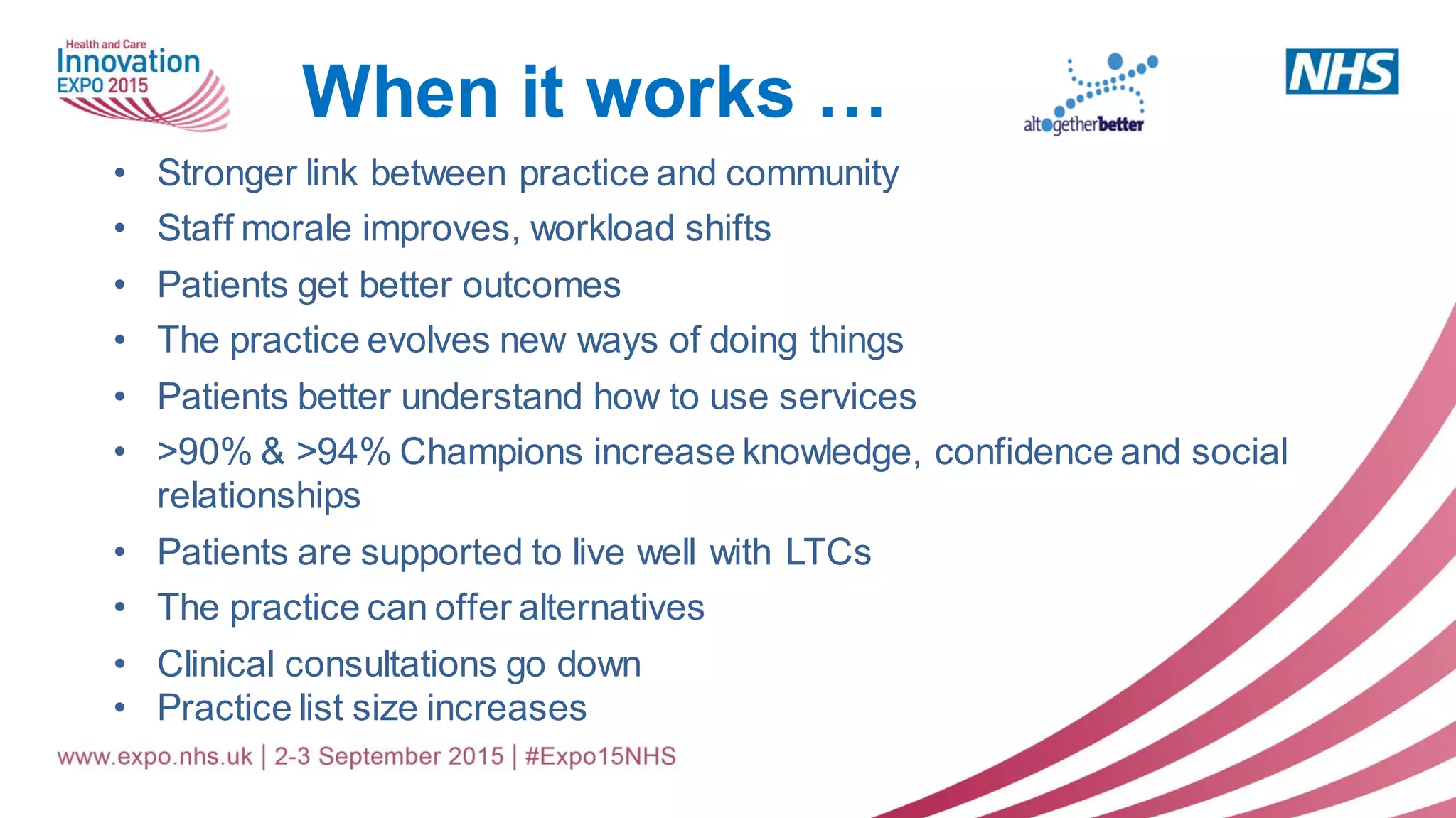
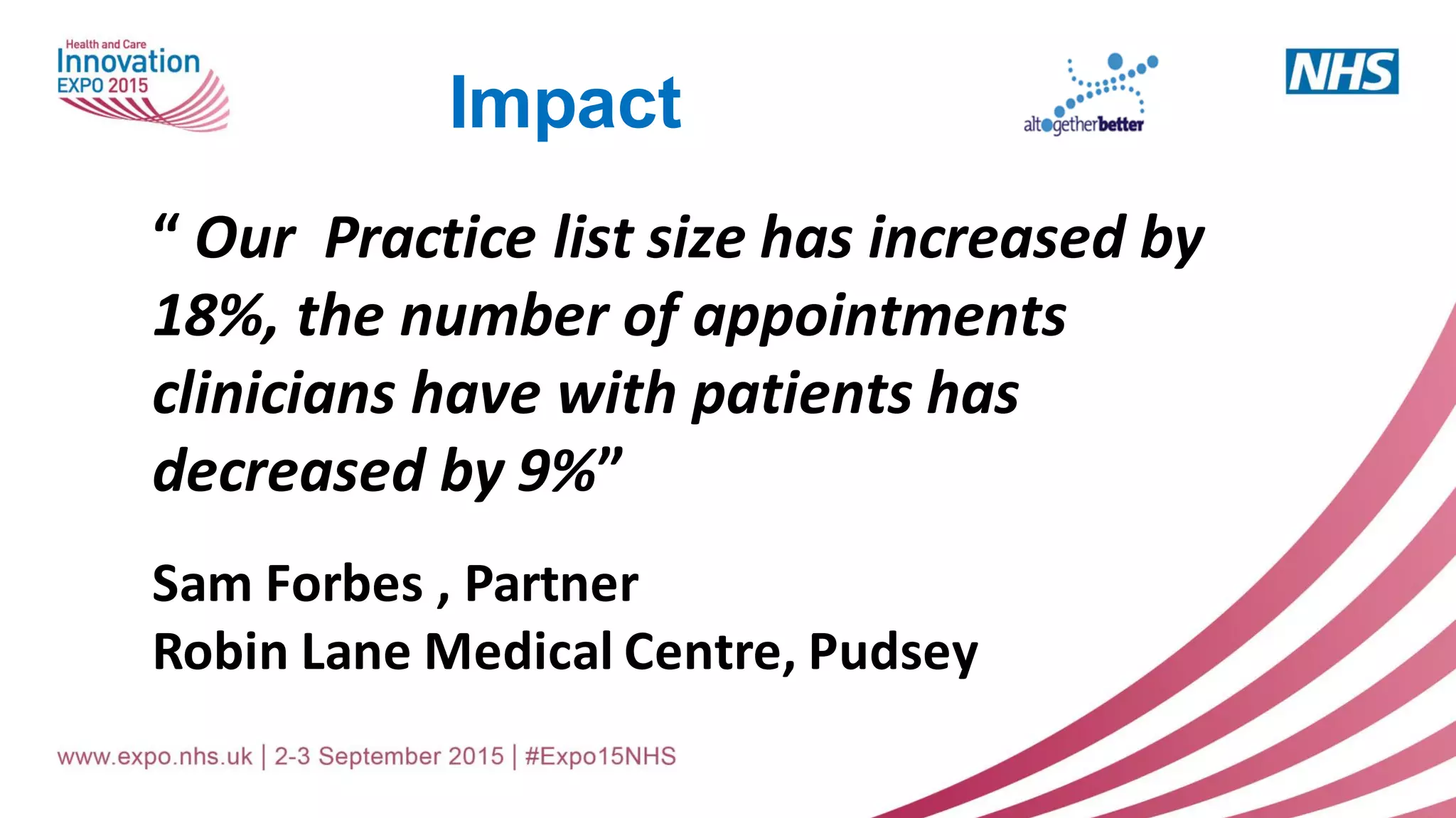
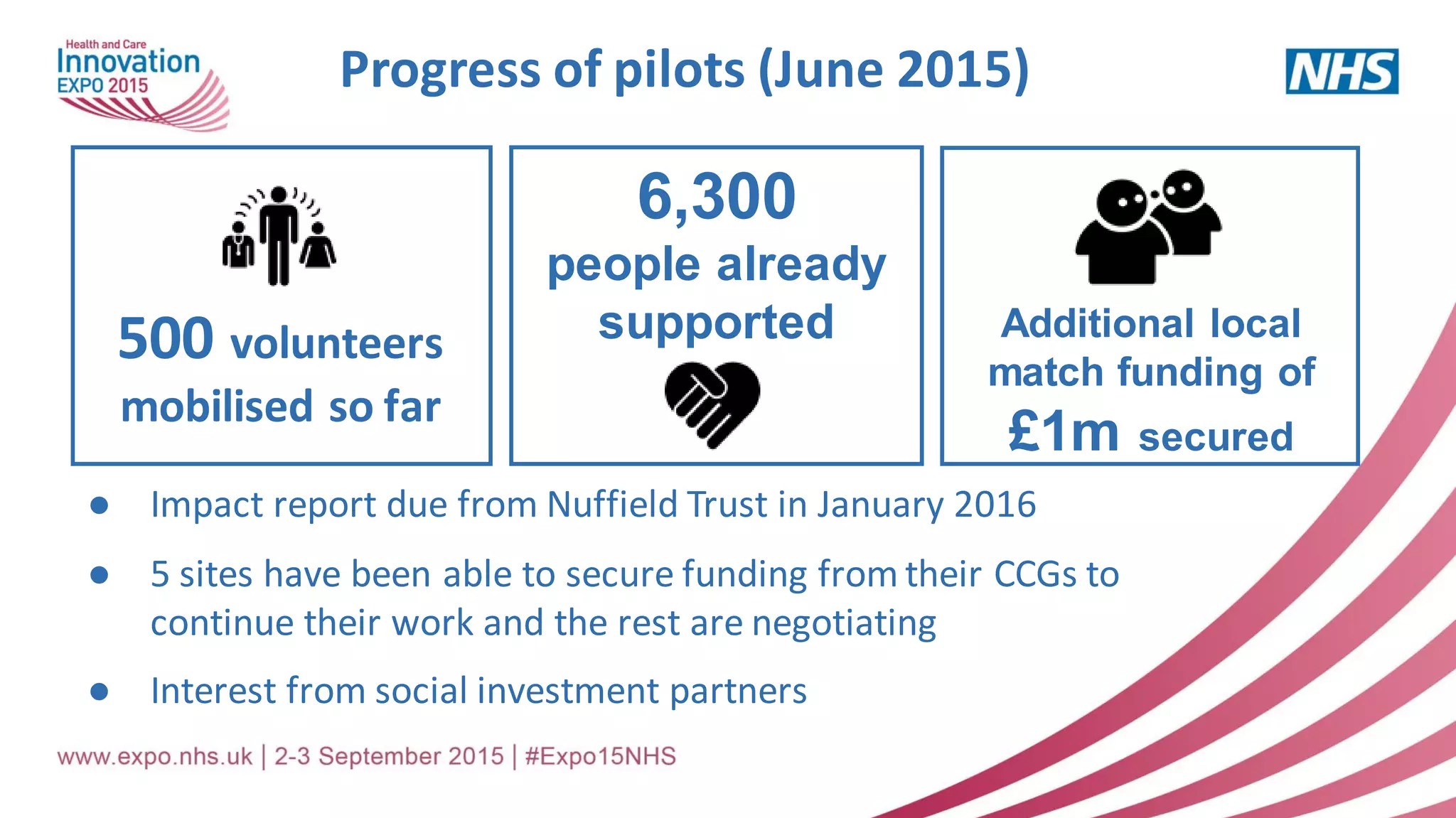
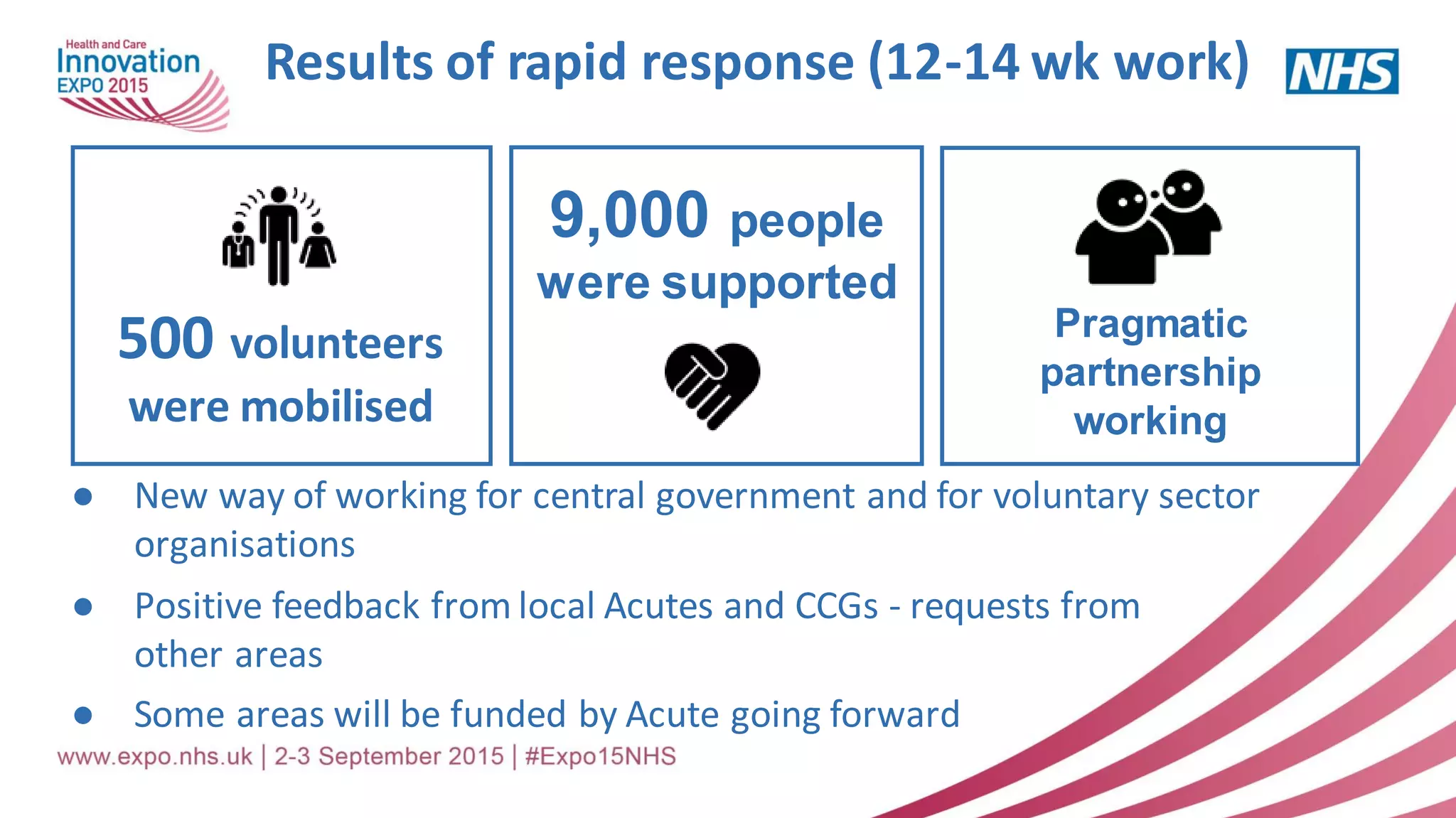
The document presents a transformative approach to healthcare by engaging citizens and communities through the Altogether Better initiative, which has created over 21,000 health champions since its inception in 2008. Emphasizing a community-centered practice, it aims to foster better relationships between patients and services, reduce pressures on the NHS, and improve health outcomes through volunteer involvement. Numerous pilot projects have mobilized volunteers to support individuals, particularly the elderly, thereby addressing rising demands on public services and creating sustainable models of care.