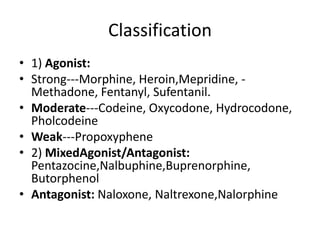
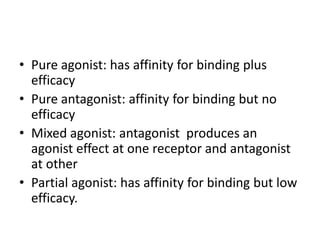
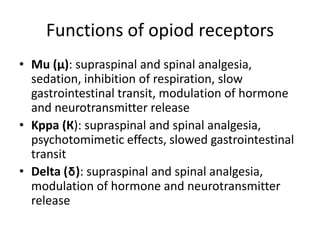
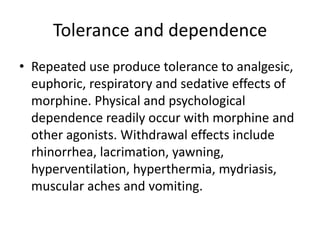
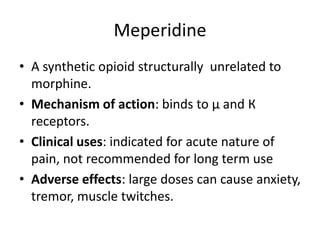
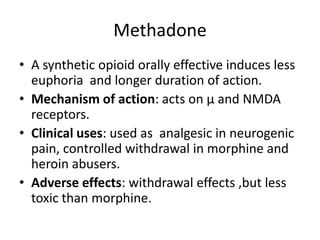
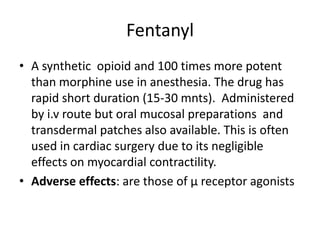
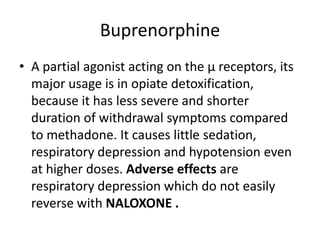
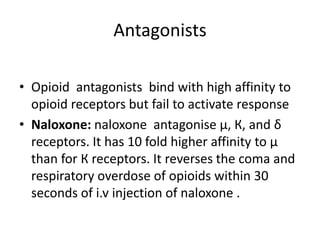
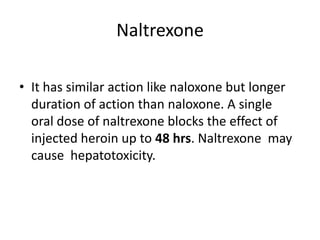
Opioids act on three types of opioid receptors in the brain and body - mu, kappa, and delta. They produce effects like analgesia, sedation, euphoria, and respiratory depression. Common opioids include morphine, codeine, oxycodone, fentanyl, and heroin. Opioids are used medically to treat severe pain but carry risks of tolerance, dependence, and overdose. Naloxone and naltrexone are opioid antagonists that can reverse the effects of opioid overdose.